Psychotropic Medication Expenditures for Community-Dwelling Elderly Persons
Abstract
Psychotropic medication expenditures for community-dwelling elderly persons in the United States were examined with the 1996 Medical Expenditure Panel Survey (MEPS). According to the MEPS, an estimated $1.07 billion was spent on psychotropic agents, and 53 percent of that was paid out of pocket. Antidepressants represented 61 percent of psychotropic expenditures. High expenditures were found for selective serotonin reuptake inhibitors ($469 million, or 44 percent of psychotropic expenditures), benzodiazepines ($241 million, or 22 percent), and tricyclic antidepressants ($119 million, or 11 percent). Estimates for psychotropic expenditures in 2002 totaled $1.41 billion after adjustment for inflation. Although psychotropic prescription costs were substantial, increased generic medication use and Medicare prescription plans could reduce the financial burden on elderly persons.
Elderly patients frequently take psychotropic agents (1,2). Researchers have found that 12.3 percent to 15.1 percent of elderly persons living in the community and up to 75 percent of long-term-care residents receive psychotropic medications (1,2). For clinical and cost reasons, these patterns have necessitated closer examination of psychotropic use. Although psychotropic medication expenditures have been examined in the general population, these studies were geographically limited, not recent, or not specific to the elderly population (3,4).
The study reported here estimated psychotropic medication expenditures for elderly persons in the United States by analyzing the Medical Expenditure Panel Survey (MEPS). The objectives of the study were to estimate total and out-of-pocket psychotropic medication expenditures by elderly persons and to examine these expenditures by psychotropic class. Determining expenditures for psychotropic medications in this population will be useful for policy makers, providers, and researchers to guide mental health care delivery and policy.
Methods
The Agency for Healthcare Research and Quality (AHRQ) and the National Center for Health Statistics conducted the MEPS to provide comprehensive data on health care use and expenditures for the U.S. civilian noninstitutionalized population. Data for the MEPS were obtained from interviews of a nationally representative sample of 21,571 individuals across the nation; respondents were interviewed three times during the year to collect calendar year utilization data. To validate the information obtained from the respondents, utilization data were obtained from providers. The detailed prescription data included drug name, National Drug Codes (NDC), and amount paid to pharmacies. According to the MEPS, weighted data from the sample panel represent national estimates of utilization and expenditure. Additional details about data collection, editing, and estimation procedures for the 1996 MEPS can be found in other sources (5,6).
For this study, all psychotropic medications used by community-dwelling persons aged 65 years or older were extracted from the MEPS prescription file. The psychotropic agents were classified on the basis of the NDC as antidepressants, antianxiety agents, sedative-hypnotics, antipsychotic agents, and stimulants (7). Price-Check PC, which uses the Generic Product Identifier (GPI), was used to extract data on psychotropic medications (8).
The data extraction from the MEPS resulted in a sample of 471 elderly patients who were using 2,847 psychotropic prescriptions. From this sample, we calculated national estimates of psychotropic use and expenditures by using the sampling weights provided by the AHRQ for the MEPS. In the MEPS, prescription expenditures represented the amount paid to pharmacies from all sources, including insurance and patients themselves. SAS version 8.0 was used to extract and analyze the survey data (9). The survey design variables were incorporated into the SAS survey statistical procedures—for example, Proc Survey Means—to accommodate the complex design of the MEPS.
Results
According to the 1996 MEPS, an estimated 36.43 million psychotropic prescriptions were dispensed to community-dwelling elderly persons for an estimated total annual cost of $1.07 billion, or nearly 5 percent of the total prescription expenditure for elderly persons in 1996. This amount represents an expenditure of $1.41 billion in 2002 after adjustment for inflation with the prescription component of the consumer price index. Average total and out-of-pocket payments per psychotropic prescription were $29.47 (95 percent confidence interval [CI], 26.46 to 32.49) and $15.69 (95 percent CI, 13.61 to 17.78), respectively. This finding indicates that elderly persons paid 53 percent of their psychotropic prescription expenses out of pocket.
Psychotropic prescription utilization and expenditure estimates are presented in Table 1. Antidepressants represented 61 percent of the psychotropic prescription expenditures; in this class the largest amount was spent on selective serotonin reuptake inhibitors (SSRIs)—44 percent of the cost of all psychotropic medications and more than 70 percent of the expenditures for antidepressants.
Tricyclic antidepressant expenditures were $119 million, or 18 percent of the total antidepressant cost. In addition, the percentage of antidepressant expenditures for tertiary-amine tricyclic antidepressants was more than one and three-fourths times that for secondary-amine tricyclic antidepressants.
Expenditures for antianxiety agents, $256 million, were more than double those for sedative-hypnotics, $127 million. These two classes combined accounted for more than one-third of the dollars spent on psychotropic prescriptions. Overall, expenditures for benzodiazepines in both antianxiety and sedative-hypnotic classes totaled $241 million and accounted for 22 percent of the psychotropic prescription costs. Expenditures for long-acting benzodiazepines, $48 million in both psychotropic classes, represented 20 percent of the benzodiazepine expenditure. Antipsychotic medications accounted for slightly more than 3 percent of the psychotropic prescription expenditures, and expenditures for atypical antipsychotics were three times those for typical antipsychotics. Expenditures for stimulants were very low.
Discussion
According to the 1996 MEPS, an estimated $1.07 billion was spent on psychotropic prescriptions for elderly persons, and more than half of that was paid out of pocket. This amount represents $1.41 billion in 2002, adjusted for inflation. Zorc and associates (4) reported psychotropic prescription expenditures of $1.45 billion for the entire U.S. outpatient population in 1985, which may indicate either increased psychotropic prescription use among community-dwelling elderly persons or an increase in the cost of psychotropic agents, or both, in 1996. The recently proposed Medicare prescription coverage plans can significantly assist elderly persons in reducing this burden.
This study found that antidepressant and antianxiety prescription use among elderly persons accounted for 60 percent and 24 percent, respectively, of all psychotropic medication expenditures. In contrast, findings involving a general population from 1985 showed that antianxiety and sedative-hypnotic agents accounted for the majority of these expenses, whereas antidepressants represented only a minor portion (4). These findings may reflect changes in utilization and cost patterns of psychotropic agents.
In this study, SSRIs accounted for more than two-thirds of the expenditures for antidepressant agents and nearly half of the total psychotropic expenses, possibly because of their high use or cost, or both. High use of SSRIs by elderly persons may be attributed to the more favorable side effect profile of SSRIs compared with tricyclic antidepressants (10). The high use of the SSRIs combined with their high costs, as shown in Table 1, contributes significantly to psychotropic expenditures. Availability of low-cost or generic SSRIs could greatly reduce the burden on elderly persons.
Tricyclic antidepressants accounted for almost one-fifth of antidepressant expenditures and more than one-tenth of psychotropic expenditures. The larger expenditure for tertiary-amine tricyclic antidepressants was due to the nearly sevenfold greater use of these agents than of the secondary-amine group; the expenditure was higher even though the average prescription cost of the secondary amines was nearly four times as high. Zorc and associates (4) also found much higher expenditures for tertiary-amine than for secondary-amine tricyclics in 1985. However, high use of tertiary-amine tricyclics by elderly persons is of concern because of their more problematic side effect profile (10). Use of secondary-amine in place of tertiary-amine tricyclics will increase expenditures, judging from the average prescription price shown in Table 1, but the change will reduce drug-related morbidity (10).
Expenditures for benzodiazepine agents accounted for 22 percent of total psychotropic expenditures. This amount is lower than previously reported, which may be attributed to decreased usage or availability of generic antianxiety agents (4). Although only one-fifth of benzodiazepine expenditures were for long-acting agents, this usage pattern should be carefully examined, because long-acting agents can accumulate in the body and cause adverse outcomes (10).
This study provided comprehensive information on psychotropic expenses by using a nationally representative sample of the elderly population in the United States. However, the findings may be limited to the definitions and data source used in the study. This limitation includes the operational definitions of "psychotropics" and the expenditure estimation procedure. Other limitations lie in the inherent disadvantages of using secondary data, such as difficulty in evaluating accuracy because of errors in data collection, editing, and imputations. Even though the total psychotropic expenditure and utilization estimates are stable, the estimates from subsamples could create potential problems in the confidence levels of smaller estimates.
Conclusions
Based on the MEPS, this study estimated that more than a billion dollars was spent in 1996 on psychotropic agents for community-dwelling elderly persons in the United States and that they paid more than half the cost out of pocket. Antidepressants represented a major portion of psychotropic prescription expenditures, and SSRIs accounted for the highest percentage of psychotropic expenditures by category. Therefore, efforts to reduce psychotropic medication expenditures for elderly persons need to focus on antidepressants, more specifically SSRIs. Availability of low-cost SSRIs, increased use of generic psychotropic agents, and Medicare prescription coverage plans can help reduce the burden on elderly persons.
Acknowledgments
This research was supported by grant AHRQ-RO3-HS-10813 from the Agency for Healthcare Research and Quality.
The authors are affiliated with the College of Pharmacy at South Dakota State University, Box 2202 C, 1 Administration Lane, Brookings, South Dakota 57007 (e-mail, [email protected]). This paper is based partly on a presentation at the annual meeting of the American Pharmaceutical Association, held March 28 to April 1, 2003, in New Orleans.
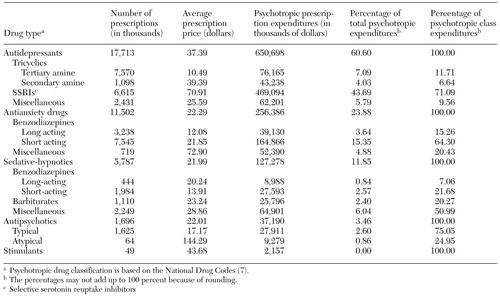 |
Table 1. Estimated expenditures for psychotropic medications by elderly community-dwelling persons in the United States, 1996
1. Dealberto MJ, Seeman T, McAvay GJ, et al: Factors related to current and subsequent psychotropic drug use in an elderly cohort. Journal of Clinical Epidemiology 50:357-364,1997Crossref, Medline, Google Scholar
2. Avorn J: Drug prescribing, drug taking, adverse reactions, and compliance in elderly patients, in Clinical Geriatric Psychopharmacology. Edited by Salzman C. Baltimore, Williams & Wilkins, 1998Google Scholar
3. Cafferata GL, Kasper JA: Psychotropic drugs: use, expenditures, and source of payment. Data Preview 14, National Medicare Care Expenditure Survey. DHHS no 83-3335. Rockville, Md, Agency for Health Care Policy Research, 1983Google Scholar
4. Zorc JJ, Larson DB, Lyons JS, et al: Expenditures for psychotropic medications in the United States in 1985. American Journal of Psychiatry 148:644-647, 1991Link, Google Scholar
5. Cohen SB, DiGaetano R, Goksel H: Estimation Procedures in the 1996 Medical Expenditure Panel Survey Household Component. MEPS Methodology Report, No 5. Pub no 99-0027. Rockville, Md, Agency for Health Care Policy and Research, 1999Google Scholar
6. Moeller JF, Stagnitti MN, Horan E: Outpatient Prescription Drugs: Data Collection and Editing in the 1996 Medical Expenditure Survey (HC-010A). MEPS Methodology Report, No 12. Pub No 01-0002. Rockville, Md, Agency for Health Care Policy and Research, 2001Google Scholar
7. Aparasu RR, Mort JR, Brandt H: Psychotropic prescription use by community-dwelling elderly in the United States. Journal of the American Geriatrics Society, in pressGoogle Scholar
8. Price-Check PC User's Guide. Indianapolis, First DataBank, 2000Google Scholar
9. SAS/STAT User's Guide, Release 8.0. Cary, NC, SAS Institute Inc, 2000Google Scholar
10. Jenike MA: Psychiatric illnesses in the elderly: a review. Journal of Geriatric Psychiatry and Neurology 9:57-82, 1996Crossref, Medline, Google Scholar



