A National Study of the Effect of Chronic Pain on the Use of Health Care by Depressed Persons
Abstract
OBJECTIVE: The objective of this study was to provide national estimates of the impact of common pain conditions such as back pain, chronic headache, self-reported arthritis, and unspecified chronic pain on the use of health services and quality of care among persons with depression. METHODS: This was a cross-sectional study of data from a U.S. national household survey conducted in 1997-1998. The participants were 1,486 community-dwelling adults who met criteria for major depression or dysthymia according to the Composite International Diagnostic Interview Short-Form. RESULTS: Depressed persons with comorbid pain (N=938) were older, had lower incomes, and reported more severe psychiatric distress than depressed persons who did not have pain. When sociodemographic characteristics and severity of psychological distress were adjusted for, comorbid pain was associated with about 20 percent more visits to medical providers by patients who made at least one visit during a year. However, the patients with comorbid pain were about 20 percent less likely to see a mental health specialist than patients without pain. Pain was also shown to be associated with greater use of complementary or alternative medicine but not with differences in the use of antidepressants. CONCLUSION: Comorbid pain among persons with depression is associated with more intensive use of general medical services but lower rates of use of mental health services.
Depression is a common, serious, and debilitating mental disorder that frequently is unrecognized, untreated, or poorly treated (1,2,3,4). The co-occurrence of physical symptoms and medical disorders may complicate detection and treatment, as indicated by many studies (5,6,7,8,9,10,11). Clinicians are well aware of the simultaneous occurrence of depressive symptoms and pain, but the implications for health care services are far less obvious. Are depressed persons with comorbid pain more likely to receive effective treatment for depression because they have more frequent contacts with health professionals than those who have depression but without somatic complaints? Or are they less likely to receive care for their mental illness because physical complaints distract their physicians from treating their depression? Are they more likely to try alternative forms of health care or self-medication? How does comorbid pain affect the use of antidepressant medications among depressed persons?
Surprisingly, there are no previous national estimates available on how comorbid pain affects patterns of health care use among persons with depression. Almost all research on the interaction between depression and pain has focused on patients who typically receive medical care from physicians who are affiliated with a local academic center. Local service use patterns, even if they can be related to the population, are often idiosyncratic and are unlikely to be representative.
For example, in two U.S. cities heavily represented in the literature—Boston and Seattle—the use of mental health specialty care among adults is higher than in other parts of the United States (12). Among children, the use of mental health specialty care in Boston is more than 2.5 times as high as in Phoenix. The most recent national study of the general household population—the National Comorbidity Survey (13)—does not appear to have analyzed the effects of comorbid pain and depression, and the data are now more than a decade old, preceding both the dramatic increase in the use of new antidepressants and the widespread application of managed behavioral health care.
In this study, we used a recent national household survey to assess differences in the characteristics of depressed persons who reported painful physical conditions and those who did not and assessed how these conditions affect health care use patterns, including the use of general inpatient and ambulatory care, mental health specialty care, antidepressants, and alternative medicine. We also assessed whether the presence of pain was associated with differences in the rates of appropriate treatment for depression, the total costs of inpatient and outpatient medical care, and total out-of-pocket expenditures for health care.
Methods
Data
We used data from the Health Care for Communities (HCC) study, a national household survey conducted in 1998 with 9,585 respondents (14). The HCC survey reinterviewed adult participants of the Community Tracking Study (CTS) an average of 15 months after their CTS interview. The CTS sample is representative of the U.S. civilian, noninstitutionalized population (15). After interviews that were conducted with ineligible respondents were discarded, there were a total of 9,585 complete interviews out of 14,985 attempts, for a response rate of approximately 64 percent.
Because the HCC study was linked to CTS participants, it was able to oversample persons who were likely to have mental health problems. As a consequence, the proportion of persons with probable mental health disorders was about 50 percent higher than in a similarly sized random population sample. The results were weighted on the basis of the inverse of the probability of selection, nonresponse, and households with no telephones. A complete description of the study has been published previously (14).
The HCC survey assessed major depressive and dysthymic disorder by using the screening versions of the Composite International Diagnostic Interview Short-Form (CIDI-SF) (16). A total of 1,486 respondents exceeded the cutoff point for probable depressive disorder and constituted the primary group of interest for this study. The survey also asked about chronic health conditions and prompted specifically for three conditions commonly associated with body pain—arthritis or rheumatism (N=2,584), chronic back problems (N=1,850), and chronic severe headache (N= 1,370)—as well as other chronic pain conditions (N=952). All survey items were single-item yes-or-no questions.
A total of 938 respondents reported both depression and at least one of the four chronic pain categories. For simplicity of presentation, we refer to participants who reported one or more of these conditions as having pain, but we recognize the diversity of possible explanations for this pain. We come back to this concept and how it may influence our conclusions in the discussion section below.
In addition, the HCC study assessed common chronic medical problems on the basis of self-report, including asthma, diabetes, hypertension, a physical disability (such as loss of a limb, loss of sight or hearing, or a birth defect), breathing difficulties, cancer diagnosed within the previous three years, stroke or major paralysis, other neurologic conditions, angina, heart failure or coronary artery disease, stomach ulcer, chronic inflamed bowel, enteritis or colitis, chronic liver disease, chronic problems urinating or bladder infections, and chronic gynecologic problems.
Service use variables included measurements of health care use, imputed costs of care, and patient out-of-pocket expenditures. A first set of service use variables reflected use of overall medical care and was based on responses to the CTS. These two measures were number of physician visits and number of hospital stays, both with a 12-month recall period. The second set of service use variables, based on responses to the HCC survey, measured the use of mental health care received by respondents. Counseling and other mental health services received from primary care physicians were not included in this measure but were included in the counts of total use of medical care. The third set of service use variables measured use of medications, including antidepressants, and self-reported use of supplements or herbs or other alternative medicines. These measures were also from the HCC survey. Although there were some differences, overall levels of service use found in the HCC were similar to those found in the Medical Expenditure Panel Survey (17,18).
Appropriate care was defined as the use of an antidepressant medication or psychotherapy during the previous year in a manner consistent with published guidelines (4). Specifically, medication treatment was considered appropriate if it was used at a dosage exceeding the recommended minimum for an adequate duration (two months) as defined by the Agency for Healthcare Research and Quality, updated for newer medications (19). Effective mental health counseling was defined as at least four visits to a mental health specialist.
We also investigated the potential difference in health care costs between the patients who reported pain and those who did not. In particular, we looked at (imputed) total costs of inpatient and outpatient services, using unit costs estimated from the Medical Expenditure Panel Survey, as well as patient self-reported out-of-pocket expenditures on all types of care.
Statistical methods
We first prepared descriptive statistics of sociodemographic characteristics and major indexes of physical and mental health status of the two groups of patients—those who reported comorbid pain and those who did not. To provide a reference point, we also calculated corresponding statistics for the general population (further analysis not shown here). The statistics were weighted to be representative of the corresponding U.S. population.
Because depressed persons with and without pain differ in other characteristics, listed in Table 1, we used multivariate analysis to estimate the effect of comorbid pain on service use. Probit models were used for dichotomous variables—any physician visit, any inpatient stay, any outpatient mental health specialty visit, any antidepressant medication, any use of alternative medicine, any use of either mental health specialty care or an antidepressant, and appropriate mental health specialty care or appropriate course of antidepressant treatment. Log-linear models were used for continuous dependent variables—number (non-zero) of outpatient visits, number of hospital stays, number of mental specialty visits, total out-of-pocket expenditures, and total inpatient and outpatient medical care costs.
Control variables included type of individual health insurance plan (employment-based insurance or insurance purchased in the individual market, Medicare, Medicaid, other insurance, or no insurance, with employment-based or individually purchased insurance as the reference group), number of chronic conditions other than pain, log of total family income, respondent's age category (19 to 24, 25 to 34, 35 to 44, 45 to 54, 55 to 64, or above 65 years, with 19 to 24 years as the reference group), race or ethnicity, marital status, and education (less than high school, high school, some college, or college or higher, with less than high school as the reference group).
We controlled for the severity of psychological distress by using the Mental Health Inventory (MHI-5), which produces a score based on answers to the five-item mental health scale included in the Short Form 36 (SF-36) Health Status Questionnaire (3). Possible scores range from 0 to 100, with higher scores indicating better mental status. All regression analyses were conducted with a correction for clustering at the HCC sites. Standard errors are Huber-White robust standard errors.
We show adjusted results, which are based on predictions from the multivariate regressions. These results are interpreted as the average effect of comorbid pain among depressed persons in the United States. We tested models that allowed the effects of different pain conditions to differ, but the effects on service use were not significantly different. Therefore, in the following section, we present results with different pain conditions combined.
Results
Descriptive statistics
Sociodemographic characteristic of the two groups of patients are summarized in Table 1. The depressed patients with comorbid pain were an average of ten years older than those without pain and were significantly more likely to be married, to have less education, and to have a much lower average annual family income than those without pain. Although the average annual family income among the depressed persons who did not have pain was slightly higher than in the general population, the average annual family income among those with both depression and pain was 38 percent lower than in the general population.
Health status also varied between the two groups. The patients with comorbid pain had significantly lower scores on the physical and mental health components of the SF-12 (a shorter version of the more commonly used SF-36) than those with no pain (41 and 40.1 compared with 46.9 and 42.4, respectively; a score of above or below 50 indicates whether the respondent falls above or below, respectively, the average in the general U.S. population). Those with pain also had much lower mental health inventory scores than those without pain (52.4 compared with 63.3).
Given that health care seeking among persons with depression is likely to be influenced by individual characteristics other than the presence of pain—which differed substantially between the two groups—in presenting the results from multivariate analyses we show only those for which severity of depression, presence of other chronic diseases, insurance status, education, income, marital status, and cultural and ethnic background were adjusted for.
Service use and health care expenditure
Our multivariate analyses showed that pain was significantly associated with three service use outcomes: a lower likelihood of having any mental health specialty visits, a greater likelihood of visiting a medical provider among patients who had at least one visit, and a greater likelihood of using complementary and alternative medicine. Pain was also positively associated with both cost variables—total health care costs and total out-of-pocket expenditures—although neither association was statistically significant.
Table 2 shows the predicted effect of pain on each of the general medical use variables, total health care costs, and total out-of-pocket expenditures. Although the presence of comorbid pain was not significantly associated with a greater likelihood of a patient's seeing a physician during the course of a year, it was associated with a significantly greater intensity of outpatient care, resulting in a 20 percent increase in the expected number of physician visits, or about one additional physician visit per year. Expected use of alternative medicine was also significantly higher among the patients with comorbid pain, who had a utilization rate of 23.7 percent, compared with 18.5 percent among those without pain, a difference of more than a quarter. Expected total health care costs were about $5,053 per year among patients without pain, compared with $5,949 per year among those with pain, a nonsignificant difference of slightly less than one-fifth. Out-of-pocket health care expenditures were higher among the patients with pain ($3,821 compared with $3,202), but the difference was not statistically significant.
Table 2 also shows the predicted effect of pain on the use of services specific to mental health. The presence of pain was associated with a 21 percent lower likelihood of a patient's seeing a mental health specialist (23.9 percent, compared with 30.3 percent for patients without pain). However, comorbid pain was not significantly associated with the number of visits among patients who had at least one visit to a mental health specialist. In combination, these two results suggest that patients with comorbid pain had 20 percent fewer mental health specialty visits overall. Pain was not associated with significant differences in the likelihood of antidepressant use or the likelihood of having either a mental health specialty visit or using an antidepressant. Nor was pain significantly associated with use of appropriate mental health care.
The presence of comorbid pain was associated with other patient characteristics, including age and psychological distress (Table 1). Of these covariates, psychological distress as measured by the MHI-5 had the most pronounced effect on the use and costs of health services. Greater psychological distress was associated with a greater number of physician visits, greater use of any mental health care service, greater likelihood of seeing a mental health specialist, greater use of antidepressants, and greater likelihood of receiving appropriate mental health care (data not shown).
Discussion and conclusions
This study had three main findings. First, the characteristics of depressed persons differed significantly according to whether these individuals reported one of the chronic pain conditions. Specifically, compared with the depressed patients who did not report comorbid pain, those who did report pain tended to be older, to have a lower family income, to have poorer physical and mental health status, and to have higher levels of psychological distress. Second, the patients with pain had several significant differences in their patterns of health service use after other population differences were controlled for. Pain was associated with more visits to medical providers (but not a higher probability of having at least one visit), fewer visits to mental health specialists (but not the number of visits per user), and greater use of complementary or alternative medicine (but not with lower rates of antidepressant use). Finally, the results of our study confirm earlier findings that only about a third of depressed persons receive care consistent with current recommendations (4,19) and extend those findings to the subset of patients who have comorbid pain.
Our findings are consistent with the belief that pain prompts persons with depression to use primary care instead of specialty care. This could occur via multiple pathways. Some people may assign pain symptoms higher levels of medical priority, especially given the stigma associated with obtaining mental health specialty care. In the presence of pain, patients perceive more reasons not to seek help from mental health specialists, especially if they interpret their emotional symptoms as the consequence of physical illness.
Furthermore, the fact that health insurance benefits for specialty mental health care are more restrictive than benefits for other types of care may serve as an additional incentive to use primary care. Finally, it may be appropriate for some persons with depression to substitute general or subspecialty medical care for mental health specialty care in circumstances in which the severity of the physical pain requires very high levels of overall medical care. Further research is needed to clarify whether one or more of these possibilities explain our general finding.
Given that this study included antidepressants in the definition of effective mental health care, our findings may overestimate the likelihood that depressed patients with pain are intentionally receiving treatment for depression. Antidepressant medications may be effective for several conditions we used to define comorbid pain, including chronic back pain (20), headache (21), and unexplained but painful conditions (22). Because we do not know the reasons for antidepressant use in this patient sample, it is possible that some of the antidepressant use was for treatment of the pain and that depression was not even diagnosed.
Among the main limitations of the study was its short assessment of conditions and its cross-sectional design. Depression was assessed by a clinical screening instrument (the CIDI-SF), not a full diagnostic interview. However, this instrument has been subjected to extensive validity testing and is very specific but not very sensitive (4,23). Thus one would expect that most individuals who are classified as being depressed have a depressive disorder. Conditions associated with pain are also assessed by single-item questions without regard to the nature or severity of the symptoms or their causation. The cross-sectional design of the study did not allow us to assess the temporal relationship between pain and depression or the effect of treatment. Also, we could not distinguish patients with chronic depression from those who were experiencing a first episode. Finally, the accuracy of the results could have been affected by response rates, in this case compounded by response rates to the initial survey (the CTS).
The results of our study may have important implications for practicing physicians and for mental health policy analysts who are interested in minimizing the number of depressed persons who go untreated. Physicians readily acknowledge the co-occurrence of depression and pain but may not recognize the degree of psychiatric distress that appears to be present in this group of patients. Such distress suggests that persons who have both depression and pain should on balance receive more—not less, as we have found to be the case—mental health specialty care than that received by depressed persons who do not have pain. Until further research is complete, general medical practitioners will want to carefully determine the nature and degree of this distress and may find referral for specialty care appropriate in some circumstances. Furthermore, from a policy perspective, analysts should carefully consider policies that may reduce potential barriers to mental health care for this vulnerable population.
Acknowledgments
This study was funded by Eli Lilly and Company. HealthCare for Communities is a project funded by the Robert Wood Johnson Foundation.
Ms. Bao and Dr. Sturm are affiliated with Rand, 1700 Main Street, Santa Monica, California 90407 (e-mail, [email protected]). Dr. Croghan is with Eli Lilly and Company Research in Indianapolis.
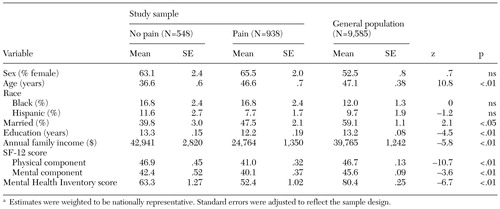 |
Table 1. Sociodemographic characteristics of depressed patients with and without comorbid paina
a Estimates were weighted to be nationally representative. Standard errors were adjusted to reflect the sample design.
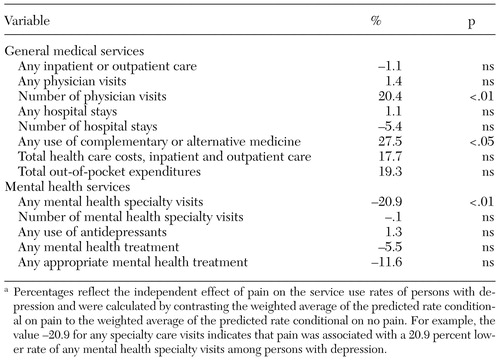 |
Table 2. Predicted effect of comorbid pain on the use of general medical and mental health services by persons with depression (N=938)a
a Percentages reflect the independent effect of pain on the service use rates of persons with depression and were calculated by contrasting the weighted average of the predicted rate conditional on pain to the weighted average of the predicted rate conditional on no pain. For example, the value -20.9 for any specialty care visits indicates that pain was associated with a 20.9 percent lowerrate of any mental health specialty visits among persons with depression.
1. Greenberg PE, Stiglin LE, Finklestein SN, et al: The economic burden of depression in 1990. Journal of Clinical Psychiatry 54:405-418, 1993Medline, Google Scholar
2. Kessler RC, McGonagle KA, Shanzang Z, et al: Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: results from the National Comorbidity Survey. Archives of General Psychiatry 51:8-19, 1994Crossref, Medline, Google Scholar
3. Wells KB, Sturm R, Sherbourne CD, et al: Caring for Depression. Cambridge, Mass, Harvard University Press, 1996Google Scholar
4. Young AS, Klap R, Sherbourne CD, et al: The quality of care for depressive and anxiety disorders. Archives of General Psychiatry 58:55-61, 2001Crossref, Medline, Google Scholar
5. Simon GE, VonKorff M, Piccinelli M, et al: An international study of the relation between somatic symptoms and depression. New England Journal of Medicine 341:1329-1335, 1999Crossref, Medline, Google Scholar
6. Gerber PD, Barrett JE, Barrett JA, et al: The relationship of presenting physical complaints to depressive symptoms in primary care patients. Journal of General Internal Medicine 7:170-173, 1992Crossref, Medline, Google Scholar
7. Kirmayer LJ, Robbins JM, Dworkind M, et al: Somatization and the recognition of depression and anxiety in primary care. American Journal of Psychiatry 150:734-641, 1993Link, Google Scholar
8. Barsky AJ, Delamater BA, Clancy SA, et al: Somatized psychiatric disorder presenting as palpitations. Archives of Internal Medicine 156:1102-1108, 1996Crossref, Medline, Google Scholar
9. Von Korff M, Simon G: The relationship between pain and depression. British Journal of Psychiatry 30(suppl):101-108, 1996Google Scholar
10. Goldman LS, Neilson NH, Clancy SA, et al: Awareness, diagnosis, and treatment of depression. Journal of Internal Medicine 14:569-580, 1999Google Scholar
11. Katon W, Sullivan M, Walker E: Medical symptoms without identified pathology: relationship to psychiatric disorders, childhood and adult trauma, and personality traits. Annals of Internal Medicine 134:917-925, 2001Crossref, Medline, Google Scholar
12. Sturm R, Andreyeva T, Ringel J: Variations in mental health specialty care across metropolitan areas. Psychiatric Services 53:674, 2002Link, Google Scholar
13. Kessler RC: The National Comorbidity Survey of the United States. International Review of Psychiatry 6:365-376, 1994Crossref, Google Scholar
14. Sturm R, Gresenz C, Sherbourne CD, et al: The design of Health Care for Communities: a study of health care delivery for alcohol, drug abuse, and mental health conditions. Inquiry 36:221-233, 1999Medline, Google Scholar
15. Kemper P, Blumenthal D, Corrigan JM, et al: The design of the Community Tracking Study: a longitudinal study of health system change and its effects on people. Inquiry 33:195-206, 1996Medline, Google Scholar
16. Kessler RC, Andrews G, Mroczek D, et al: The World Health Organization Composite International Diagnostic Interview Short-Form (CIDI-SF). International Journal of Methods in Psychiatric Research 7:171-185, 1998Crossref, Google Scholar
17. Machlin SR, Cohen JW, Zuvekas SH, et al: Health care expenses in the community population, 1996. AHRQ pub 01-0027. Rockville, Md, Agency for Healthcare Research and Quality, 2001Google Scholar
18. Sturm R: The effects of obesity, smoking, and problem drinking on chronic medical problems and health care costs. Health Affairs 21(2):245-153, 2002Google Scholar
19. Depression Guideline Panel: Depression in Primary Care: Treatment of Major Depression. Rockville, Md, Agency for Health Care Policy and Research, 1993Google Scholar
20. Solerno SM, Browning R, Jackson JL: The effect of antidepressant treatment on chronic back pain. Archives of Internal Medicine 162:19-24, 2002Crossref, Medline, Google Scholar
21. Tomkins GE, Jackson JL, O'Malley PG, et al: Treatment of chronic headache with antidepressants: a meta-analysis. American Journal of Medicine 111:54-63, 2001Crossref, Medline, Google Scholar
22. O'Malley PG, Jackson JL, Santoro J, et al: Antidepressant therapy for unexplained symptoms and symptom syndromes. Journal of Family Practice 48:980-990, 1999Medline, Google Scholar
23. Murphy JM, Monson RR, Laird NM, et al: A comparison of diagnostic interviews for depression in the Stirling County Study: challenges for psychiatric epidemiology. Archives of General Psychiatry 57:230-236, 2000Crossref, Medline, Google Scholar



