Datapoints: Detection of Substance Use Disorders in Veterans Affairs Primary Care Clinics
Increasingly, primary care providers are being called on to screen for at-risk substance use. The literature documents the continuing struggle in primary care to incorporate such screening into routine care (1,2). The objective of this study was to investigate patterns of diagnosis of substance use disorders in Department of Veterans Affairs (VA) primary care clinics over the past several years. Specifically, we wanted to determine whether the mandatory implementation of the Prevention Index in 1999 had an impact on rates of diagnosis of substance use disorders. The Prevention Index includes a screen for at-risk drinking.
Data on all primary care visits were gathered from the VA's national outpatient service use database for five fiscal years—1997 through 2001. All visits are coded with a primary diagnosis and up to ten secondary diagnoses. The secondary diagnoses indicate additional problems to be addressed during the visit and complicating factors associated with the primary diagnosis. Scrambled Social Security numbers allow for identification of unique patients.
Overall, rates of diagnosis for substance use disorders increased (Figure 1). As a percentage of all primary care patients in the VA system, the rate of primary care VA patients receiving either a primary or a secondary diagnosis went from 6.4 percent in 1997 to 9.9 percent in 2001. The increase was a result of secondary diagnoses, which increased from 4.1 percent in 1997 to 8.7 percent in 2001. Rates of a primary diagnosis of a substance use disorder did not change from 1997 to 2001. All yearly changes in rates from 1997 through 2001 were significant at p<.001. The increases in 2000 and 2001 for secondary diagnoses and for primary and secondary combined were higher than those in previous years.
The increases in rates may be partly attributable to screening for alcohol problems by use of the Prevention Index. We have no reason to believe that an increase in the prevalence of substance use disorders in the population served by the VA occurred. However, we cannot ascribe a causal relationship between use of the Prevention Index and the increase in diagnosis rates.
That the increase resulted solely from secondary diagnoses was unexpected. This finding may indicate that primary care providers are reluctant to record primary diagnoses of substance use disorders or that VA patients with more severe substance use problems may be less likely to come to primary care clinics and more likely to go directly to a VA substance abuse treatment program. More focused research at the clinic level could improve our understanding of these results.
Acknowledgment
This work was supported by VA Health Services Research and Development Service grant IIR-98086-3.
The authors are affiliated with the Health Services Research and Development Center for Mental Healthcare and Outcomes Research of the Central Arkansas Veterans Healthcare System, 2200 Fort Roots Drive, Building 58 (Slot 152-NLR), North Little Rock, Arkansas 72114 (e-mail, [email protected]). Dr. Curran, Dr. Kirchner, and Dr. Booth are also with the department of psychiatry and behavioral sciences at the University of Arkansas for Medical Sciences in Little Rock. Data from this study were presented at the annual meeting of the Research Society on Alcoholism, held June 28 to July 3 in San Francisco. Harold Alan Pincus and Terri L. Tanielian, M.A., are editors of this column.
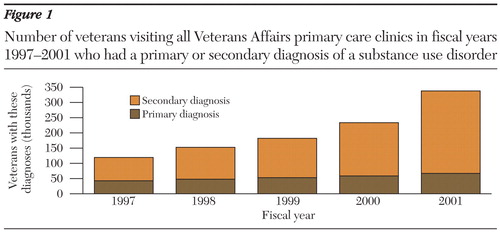
Figure 1. Number of veterans visiting all Veterans Affairs primary care clinics in fiscal years 1997-2001 who had a primary or secondary diagnosis of a substance use disorder
1. Spandorfer JM, Israel Y, Turner BJ: Primary care physicians' views on screening and management of alcohol abuse: inconsistencies with national guidelines. Journal of Family Practice 48:899–902, 1999Medline, Google Scholar
2. Rost K, Zhang M, Fortney J, et al: Persistently poor outcomes of undetected major depression in primary care. General Hospital Psychiatry 20:12–20, 1998Crossref, Medline, Google Scholar