Perceived Coercion at Hospital Admission and Adherence to Mental Health Treatment After Discharge
Abstract
The authors investigated whether mental health inpatients' perceptions of coercion were associated with later treatment adherence. Psychiatric inpatients receiving acute care at three sites were interviewed during their hospitalization and up to five times after discharge. Patients' perceptions of coercion were measured at admission. Adherence to medication and clinical treatment was measured every ten weeks for one year after discharge. Among the 825 patients who had a perceived coercion score and ten-week follow-up data and who reported that outpatient treatment was prescribed, perceived coercion scores were not associated with treatment adherence. The authors concluded that perceived coercion neither increases nor decreases psychiatric inpatients' medication adherence or use of treatment services after discharge.
Coercion plays a highly controversial role in the provision of mental health services. Although debate about coercion in mental hospital admission often rests on moral issues, empirical rationales for and against coercion are frequently invoked as well (1). Many patient advocates believe that coerced treatment is less effective than voluntary treatment and can even have antitherapeutic effects (2). On the other hand, many mental health care practitioners feel the need to use coercion to varying degrees in the best interest of patients who may not be capable of making their own medical decisions (3).
The effects of perceived coercion on patient outcomes and adherence have important policy implications and require further research (4). One study of 123 patients found that the perceived benefits of hospitalization, the duration of hospitalization, and functioning as measured by the Global Assessment Scale among patients who perceived high levels of coercion were similar to those among patients who perceived little or no coercion (5). However, another study of 59 patients found that those who felt that their admission was coerced were less likely to take medications, use mental health center services, or show improvement in functioning or symptoms over time (6).
In this study we focused on a question that Parrish (7), Campbell and Schraiber (2), and Lidz (4) have raised: is coercion associated with future treatment adherence? We examined perceived coercion at the time of hospital admission and explored the relationship of this perception with self-reported adherence to treatment after discharge to the community. Our data came from a multisite study of acute psychiatric inpatients who were interviewed in the hospital and up to five times in the year following their discharge.
Methods
Our study involved analysis of data generated by the MacArthur Violence Risk Assessment Study, which has been described in detail elsewhere (8). No institutional review board approval was required for these analyses, because the data are now available for public use and void of identifiers. From mid-1992 until October 1994, admissions were sampled from acute psychiatric inpatient facilities at three sites, located in Pittsburgh, Pennsylvania; Kansas City, Missouri; and Worcester, Massachusetts. Study participants were civil admissions, aged 18 to 40, English speaking, and white or African American, or, in Worcester only, Hispanic. They had been hospitalized less than 21 days before recruitment and had a chart diagnosis of schizophrenia, schizophreniform disorder, schizoaffective disorder, depression, dysthymia, mania, brief reactive psychosis, delusional disorder, alcohol or drug abuse or dependence, or personality disorder. The Admission Experience Survey (9) and a number of other research instruments were administered to all enrolled patients (N=1,136).
It was planned that participants would be reinterviewed five times, taking part in one interview every ten weeks during the year following their discharge from the hospital. The data analyzed in the study reported here are from the first interview at ten weeks after discharge. Patients were asked a broad range of questions, including whether medication or other outpatient mental health treatment had been prescribed for them after their hospitalization and the degree to which they adhered to medication and other treatment.
This study focused on perceived coercion as measured by the MacArthur Perceived Coercion Scale, which was created for the larger study (8) and which consists of five true-false items in the Admission Experience Survey: "I felt free to do what I wanted about coming to the hospital"; "I chose to come into the hospital"; "It was my idea to come to the hospital"; "I had a lot of control over whether I went into the hospital"; and "I had more influence than anyone else on whether I came into the hospital."
Each "true" is scored 0 and each "false" is scored 1. The scale has been shown to be psychometrically sound in that it is closely correlated with lengthier interview-based measures of perceived coercion (9) and is stable over time (5).
Adherence to prescribed outpatient treatment sessions was measured with a series of questions asking study participants what kind of treatment had been prescribed for them, how often they were supposed to attend sessions, and how often they actually attended. A ratio of the number of sessions attended to the number of sessions assigned was calculated to measure treatment adherence. Participants were considered adherent if they attended at least 75 percent of their prescribed treatment sessions.
To measure adherence to prescribed medication treatment, patients were asked what medications—if any—they were prescribed and whether they ever took more or less medication than prescribed. Patients were considered nonadherent if they refused to take prescribed medication, increased or decreased their dosages, or did not fill their prescriptions. It should be noted that some patients reported that no outpatient treatment sessions or medications had been prescribed for them.
Results
An initial interview, including calculation of a perceived coercion score, was conducted while the patient was hospitalized. Of the 1,136 patients who had initial interviews, 951 took part in the first ten-week follow-up interview. Of these 951 patients, 825 had a valid coercion score and information available from the first follow-up at ten weeks.
Because scores on the Perceived Coercion Scale during the baseline hospitalization were bimodally distributed, they were dichotomized. Scores of 0, 1, and 2 were classified as "low perceived coercion" (N=490, or 59.4 percent of the sample), and scores of 3, 4, and 5 were classified as "high perceived coercion" (N=335, or 40.6 percent of the sample).
The patients in the high-coercion group were significantly more likely to have a primary diagnosis of substance dependence or abuse and to be female, white, and involuntarily admitted and were less likely to have a primary diagnosis of depression. Number of prior hospitalizations, age, and employment status did not differ between the high- and the low-coercion groups.
Of the 825 patients who had valid coercion scores and information available from the first follow-up at ten weeks, 27.6 percent (223 of 809) reported that no postdischarge medication was prescribed, and 34.8 percent (252 of 724) reported that no postdischarge outpatient treatment sessions were prescribed.
No significant differences were found in reported adherence (to medication or outpatient treatment sessions) after discharge between patients with high coercion scores and those with low coercion scores. This remained the case at all five follow-ups, regardless of whether participants who reported that no postdischarge treatment had been prescribed for them were included in the sample.
As shown in Table 1, no significant bivariate correlations were found between perceived coercion at admission and adherence reported by patients at the first follow-up. Nor was perceived coercion a significant predictor of adherence (to medication or outpatient treatment sessions at any follow-up period) in a regression model that controlled for the background variables listed in Table 1.
As a further check, we used a mixed-model approach, analyzing each follow-up as a separate case and allowing multiple observations for each person. The results based on this approach generally confirmed the analyses reported above.
Discussion and conclusions
These data are among the first systematic data to be reported on the associations between perceived coercion at the time of hospital admission and patient adherence to medication and other treatment after discharge. In this data set, such associations were not found. We found no support for the belief that higher levels of perceived coercion at the time of hospitalization lead to future nonadherence to prescribed mental health care.
We emphasize that our empirical findings do not address—and run the risk of diverting attention from—important and contested issues related to the prospective service recipients' moral rights to decision-making autonomy and human dignity.
Certainly, within the empirical domain, we have not measured all potentially relevant outcomes of coerced hospitalization, such as the effects of coercion on patients' functioning and quality of life or on service providers or family members. There are also limitations to the outcome measures on which we did focus: the adherence data were obtained from patient self-reports. This issue illustrates the need to use, in future work, some additional measures of adherence to medications and other treatments. Perhaps including service providers in data collection, as Steadman and associates (10) did in their assessment of a New York outpatient commitment program, would produce more accurate estimates of adherence.
Acknowledgments
This study was supported by the John D. and Catherine T. MacArthur Foundation's MacArthur Initiative on Mandated Community Treatment. The authors would like to thank Steven Banks, Ph.D., for his assistance in data analysis.
Ms. Rain, Ms. Robbins, Dr. Steadman, and Dr. Vesselinov are affiliated with Policy Research Associates, Inc. Ms. Williams is affiliated with the Center for Mental Health Services Research at The University of Massachusetts Medical Center in Worcester, Massachusetts. Dr. Monahan is affiliated with the University of Virginia School of Law in Charlottesville, Virginia. Send correspondence to Ms. Robbins at Policy Research Associates, Inc., 345 Delaware Ave., Delmar, New York 12054 (e-mail, [email protected]).
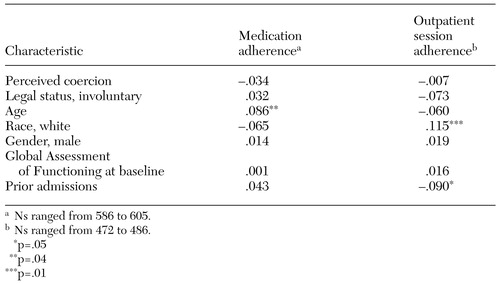 |
Table 1. Pearson correlations between patient characteristics and self-reported treatment adherence at the ten-week follow-up interview after hospital discharge
1. Wertheimer A: A philosophical examination of coercion for mental health issues. Behavioral Sciences and the Law 11:239-258, 1993Crossref, Google Scholar
2. Campbell J, Schraiber R: In Pursuit of Wellness: The Well-being Project. Sacramento, Calif, California Department of Mental Health, 1989Google Scholar
3. Group for the Advancement of Psychiatry: Forced Into Treatment: The Role of Coercion in Clinical Practice. Washington, DC, American Psychiatric Press, 1994Google Scholar
4. Lidz CW: Coercion in psychiatric care: what have we learned from research? Journal of the Academy of Psychiatry and the Law 26:631-637, 1998Google Scholar
5. Nicholson RA, Ekenstam C, Norwood S: Coercion and the outcome of psychiatric hospitalization. International Journal of Law and Psychiatry 19:201-217, 1996Crossref, Medline, Google Scholar
6. Kaltiala-Heino R, Laippala P, Salokangas RKR: Impact of coercion on treatment outcome. International Journal of Law and Psychiatry 20:311-322, 1997Crossref, Medline, Google Scholar
7. Parrish J: Involuntary use of interventions: pros and cons. Innovations and Research 2:15-22, 1993Google Scholar
8. Monahan J, Steadman HJ, Silver E, et al: Rethinking Risk Assessment: The MacArthur Study of Mental Disorder and Violence. New York, Oxford University Press, 2001Google Scholar
9. Gardner W, Hoge S, Bennett N, et al: Two scales for measuring patients' perceptions of coercion during mental hospital admission. Behavioral Sciences and the Law 11:307-321, 1993Crossref, Medline, Google Scholar
10. Steadman HJ, Gounis K, Dennis D, et al: Assessing the New York City involuntary outpatient commitment pilot program. Psychiatric Services 52:330-336, 2001Link, Google Scholar



