Datapoints: Moving From Inpatient to Residential Substance Abuse Treatment in the VA
Beginning in 1995 the Department of Veterans Affairs (VA) began shifting the focus of health care away from intensively staffed inpatient hospital units, particularly for patients with psychiatric and substance use disorders (1). At the same time, the VA began expanding lower-cost, lower-intensity beds in residential settings such as domiciliaries and therapeutic residences for patients who need care in a 24-hour setting. This column describes the nature of these changes and their impact on substance abuse patients and staff.
Data on program structure, staffing, and patients were gathered through surveys conducted in October of 1994, 1997, and 2000 of all VA substance abuse treatment programs (2). For this report, all data were aggregated to the national level.
By October 2000, inpatient substance abuse treatment beds were almost eliminated at VA facilities (see Figure 1). The number of residential beds more than doubled from 1994 to 2000, but this increase was not enough to fully offset the 91 percent decrease in inpatient substance abuse beds. The net result of these two trends is a system that is about half the size of the former system and that has moved from relying primarily on medical inpatient beds to relying almost exclusively on lower-cost residential beds in nonmedical settings.
Concurrent with these changes, the proportion of substance abuse treatment programs that had patients on waiting lists rose from 68 percent to 75 percent for inpatient programs and from 58 percent to 80 percent for residential programs. These increases likely reflect the reduction in the absolute number of beds as well as the fact that the residential beds become available infrequently because the average length of stay for patients in these settings is 38 days.
Psychiatrists were significantly affected by the shift from inpatient to residential substance abuse treatment beds. VA substance abuse programs in inpatient settings average one full-time psychiatrist on staff for every 18 beds, compared with one psychiatrist per 83 beds in residential settings. The shift to residential care thus resulted in a substantial diminishment of the role of psychiatrists in 24-hour substance abuse care settings in the VA health system. Thus the shift in locus of care from inpatient to residential settings has significantly altered the content of substance abuse care in the VA system as well as its structure and accessibility.
Acknowledgments
This work was funded by the VA Mental Health Strategic Healthcare Group.
The authors are affiliated with the VA Program Evaluation and Resource Center, 795 Willow Road (152), Menlo Park, California 94025 (e-mail, [email protected]). Harold A. Pincus, M.D., and Terri Tanielian, M.A., are editors of this column.
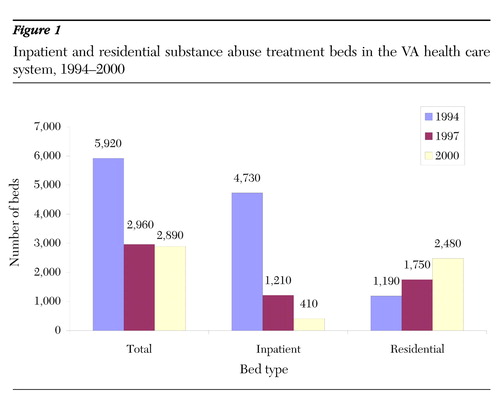
Figure 1. Inpatient and residential substance abuse treatment beds in the VA health care system, 1994-2000
1. Humphreys K, Huebsch PD, Moos RH, et al: The transformation of the Veterans Affairs substance abuse treatment system. Psychiatric Services 50:1399-1401, 1999Link, Google Scholar
2. Humphreys K, Horst D: The Department of Veterans Affairs substance abuse treatment system, July 2001. Available at www.chce.research.med.va.gov.Google Scholar



