Symptoms and Deviant Behavior Among Eight-Year-Olds as Predictors of Referral for Psychiatric Evaluation by Age 12
Abstract
OBJECTIVE: This study examined whether psychiatric symptoms and deviant behavior among eight-year-old children predicted referral for a psychiatric consultation by age 12. METHODS: A total of 1,268 children in Finland were assessed at age eight and again four years later. Three questionnaires—the Rutter A2 Scale for parents, the Rutter B2 Scale for teachers, and the Children's Depression Inventory (CDI)—were used at both time points. Other variables were socioeconomic status, family structure, and residence in an urban, rural, or semirural environment. One-way analysis of variance was used, and risk ratios were calculated to assess the extent to which children who were later referred for evaluation or for whom referral was considered were likely to have had scale scores in the deviant range at age eight. RESULTS: Only 3.3 percent of the children had been referred for an evaluation by age 12. Referral had been considered for another 2.9 percent of the children. The deviance scores of the referred children and those considered for referral were significantly higher on all scales at both time points. When the analysis controlled for gender and the other variables, the referred children were more likely than those not referred or considered for referral to have had high scores four years earlier on the teachers' scale and on the CDI. Children considered for referral were more likely than those not referred or considered for referral to be male and to have scored high on the CDI four years earlier. CONCLUSIONS: Psychiatric problems of younger children predict referral for psychiatric evaluation years later.
Studies of children with psychiatric disturbances have found that referral to mental health services is selective and that most children with psychiatric disorders receive no professional help (1,2). Most cross-sectional studies have shown that referral to and use of services are associated with the psychiatric disorder of the child as well as factors related to the child's family, such as a dysfunctional family climate in which verbal and physical aggression are displayed, the current stress faced by the family, and the burden experienced by the parents as a result of the child's disorder (3,4,5).
Children who experience several psychiatric symptoms (6), including both internalizing aggressive behavior and, in particular, externalizing aggressive behavior (4,7,8), are more likely than other children to be referred for psychiatric evaluation. Impaired functioning and severity of illness also have been reported to have an impact on the use of mental health services independently of symptoms and diagnosis (2,9).
Our knowledge of the factors that predict referral of children for psychiatric evaluation is rather scanty. Longitudinal prospective studies to evaluate referrals are rare, and no studies have attempted to identify factors related to referrals made by teachers. However, it is known that teachers are likely to identify the mental health problems of children, and they are also in a special position to help children and their families obtain mental health services.
In this study we investigated whether referral of children for psychiatric consultation by the age of 12 can be predicted by psychiatric symptoms and deviant behavior at age eight. We also aimed to identify what kinds of psychiatric deviance, if any, at age eight are associated with a higher probability of referral by age 12. Use of the word "deviance" to describe the behavioral problems of children might be considered pejorative by some, and there is, rightly, a move away from the use of stigmatizing language. However, for the sake of brevity we use "deviance" to refer to such problems.
Methods
Sample
This research was part of a larger study, and the sample and procedures have been described in more detail elsewhere (7,10). The study was conducted at two time points: in the fall of 1989 and in the fall of 1993. As described more fully below, three questionnaires were used as assessment instruments: the Rutter A2 Scale for parents (11), the Rutter B2 Scale for teachers (12), and the Children's Depression Inventory (CDI) (13,14).
The sample of 1,316 children was originally drawn from the total population of 11,518 children born in 1981 and living in the Kuopio University catchment area in eastern Finland. The proportions of children living in urban areas (35.5 percent), suburban areas (16.6 percent), and rural areas (47.9 percent) were reflected in the study sample. The mean age of the children studied was 8.5 years in 1989 and 12.5 years in 1993.
In 1989 all three questionnaires were returned for 1,268 children—646 boys and 622 girls—for a response rate of 96.4 percent. In 1993 the same questionnaires were used for all children who took part in 1989. The Rutter parents' scale was returned for 1,128 children, or 89 percent, and the Rutter teachers' scale for 1,098 children, or 86.8 percent. The CDI was completed by 1,157 children, or 91.2 percent. No significant differences were found in gender, the likelihood of scoring in the deviant range in 1989, and parental socioeconomic status between the children who remained in the study and those who dropped out.
Procedures
In 1989 the researchers visited each school and informed the teachers and children about the study. They gave each child the Rutter parents' scale and a letter about the study to take home. The parents were asked to return the questionnaire to the school in a sealed envelope. The children whose parents consented to their participation in the study completed the CDI in class, and teachers completed the Rutter teachers' scale for each child. In 1993 the procedure was the same except that the researchers did not visit the schools. Instead, teachers were asked by letter to give the Rutter parents' scale to the children to take home along with a letter providing information about the study. In both 1989 and 1993 the teachers returned all the material to the researchers. The research was approved by the ethical committee of Kuopio University and Kuopio University Hospital.
The Rutter parents' and teachers' scales and the CDI are reliable and widely used instruments for studying psychiatric disturbances (14,15,16). The Rutter parents' scale is a 31-item questionnaire that measures psychiatric symptoms and deviant behavior. Items are grouped into three sections: eight questions address health problems, such as headache and bed-wetting; five questions address sleeping, eating, speech, and stealing; and 18 questions address other aspects of the child's behavior. The answers are rated on a scale of 0 to 2, with higher ratings indicating more severe symptoms. Possible ratings on the scale range from 0 to 62.
The Rutter teachers' scale is a 26-item questionnaire designed to evaluate behavior at school. Answers are rated on a scale of 0 to 2, with higher ratings indicating more severe symptoms. Possible ratings on the scale range from 0 to 52.
The CDI consists of 27 items designed to screen for depression among children. Each item consists of three sentences, and the child is asked to choose the one that best suits him or her. The CDI item about suicide was excluded in 1989 because we thought it would be distressing to eight-year-old children. Responses are rated on a scale of 0 to 2, with higher ratings indicating more severe symptoms. Possible ratings on the scale ranged from 0 to 52 in 1989 and 0 to 54 in 1993.
We added questions about socioeconomic status and the structure of the family to the Rutter parents' scale. A question about whether the child had been referred for psychiatric evaluation or treatment because of behavioral or emotional difficulties was added to the teachers' scale along with a question about whether such a referral had been considered at the school.
Children whose scores were in the 90th percentile for deviance on the scales used were considered to be psychologically deviant.
Statistical methods
Descriptive statistics were computed, and Kruskal-Wallis one-way analysis of variance was used to examine the differences. We conducted post hoc analyses using the Mann-Whitney U test with the Bonferroni correction. Odds ratios were calculated to assess the extent to which children who were later referred for a psychiatric evaluation or considered for referral were likely to have scored in the deviant range in 1989. Further analysis used subsequent referral as the dependent variable and examined the extent to which a deviant score on each of the three scales predicted referral. Gender, socioeconomic status, family structure, and the environment in which the child lived were included in the logistic regression models because these factors are known to influence children's behavior. For each of the instruments, psychiatric deviance was measured as a dichotomous variable—a score in the 90th percentile or below the 90th percentile. Family structure was categorized into four groups according to whom the child lived with—both natural parents, a natural parent and a stepparent, the natural mother or father, and other. Socioeconomic status was that of the father; if that information was not available, the status of the mother was used. Socioeconomic status was categorized into three groups: professionals; minor professionals, such as owners of small businesses and nurses, and skilled workers; and other. Three categories were used to describe the child's environment—urban, semirural, and rural. Four logistic regression analyses were conducted.
Results
The questions concerning referral for psychiatric consultation were answered for 1,087 children. By 1993 a total of 36 children (3.3 percent) had been referred for psychiatric consultation because of behavioral or emotional problems reported by the teacher. Referral had been considered for 31 children (2.9 percent) but had not occurred. The remaining 1,020 children (93.8 percent) had neither been referred nor considered for referral.
Children who were referred or considered for referral scored significantly higher than other children on all three scales in 1993 (Rutter parents' scale, χ2=36.3, df=2, p<.001; Rutter teachers' scale, χ2=156.2, df=2, p<.001; CDI, χ2=16.2, df=2, p<.001).
Post hoc analyses showed that the 1993 scores of the referred children were significantly higher than those of the children who were not referred or not considered for referral (Rutter parents' scale, Z=5.21, p<.001; Rutter teachers' scale, Z=9.02, p<.001; CDI, Z=2.62, p=.03). Children considered for referral also scored higher than the children not referred or not considered for referral (Rutter parents' scale, Z=3.2, p<.005; Rutter teachers' scale, Z=9.05, p<.001; CDI, Z=3.13, p=.005). No significant differences in scores were found between the referred children and those considered for referral.
In 1989 the mean±SD score of the referred children on the Rutter teachers' scale was 11±6.6. A Kruskal-Wallis one-way analysis of variance indicated that this mean score was significantly higher (p<.001) than that of the children considered for referral, 8.5±6.4, and that of the children who were neither referred nor considered for referral, 3.2±4.5. A Kruskal-Wallis test also showed significant differences (p<.001) in mean scores in 1989 on the Rutter parents' scale: 10.1±5.6 for the referred children, 8.5±6.5 for those considered for referral, and 5.9±4.4 for the remaining children.
In 1989 the mean±SD CDI scores of the referred children and those considered for referral were similar (10.2±6.5 and 10.7±6.3). A Kruskal-Wallis test indicated that the mean CDI score of the remaining children, 6.1±5.2, was significantly lower (p<.001). Post hoc analyses using the Bonferroni correction showed that the referred children's 1989 scores on all three instruments differed significantly from those of the children who were not referred or not considered for referral (Rutter parents' scale, Z= 5.04, p<.001; Rutter teachers' scale, Z=7.36, p<.001; CDI, Z=4.02, p<.001). Scores of the children who were considered for referral differed significantly on two scales from those of the children neither referred nor considered for referral—the Rutter teachers' scale (Z= 5.47, p<.001) and the CDI (Z=4.31, p<.001). No statistically significant differences in 1989 CDI scores were found between referred children and those considered for referral.
Risk ratios were calculated to assess the likelihood that the 1989 scores of the children who were referred or considered for referral were in the 90th percentile on each scale—and on at least one of the scales—compared with the scores of the remaining children. The same method was used to examine whether the scores of the referred children differed in this respect from the scores of those considered for referral.
As Table 1 shows, both the referred children and those considered for referral were more likely than the remaining children to have had high scores in 1989. However, no significant differences were found between the referred children and those considered for referral in the relative risk of a high score in 1989. The referred children were 7.3 times as likely to score in the high range on at least one of the scales as the children who were not referred or not considered for referral—that is, all remaining children in the sample. The relative risk was 5.2 for children who were considered for referral compared with the remaining children. The higher 1989 scores for the referred children were most apparent on the Rutter teachers' scale, on which the referred children were 8.6 times as likely to score in the high range. However, the referred children also were more likely than the remaining children to score high on the other scales—four times as likely on the Rutter parents' scale and 4.4 times as likely on the CDI. The children considered for referral were also more likely to have higher 1989 scores than the remaining children; the relative risks were lower but clearly significant.
Four logistic regression analyses examined the relationships between whether a child had been referred for a psychiatric evaluation by 1993 and the child's 1989 deviance scores, socioeconomic status, family structure, and gender. The analysis first compared the referred children and the remaining children. As shown in Table 2, a score in the high range on the Rutter teachers' scale in 1989 increased the probability of referral 5.2 times. The probability of referral was 2.3 times greater if a child had high scores on the CDI in 1989.
In the second analysis, the children considered for referral and the remaining children were compared. A high score on the CDI increased the likelihood of referral 3.3 times, and being male increased the likelihood 4.3 times. The third analysis included the referred children and those considered for referral and showed no statistically significant differences.
In a further analysis, the referred children and those considered for referral were grouped together and compared with the remaining children. Being referred or considered for referral was 3.5 times as likely if the child had a score in the high range on the Rutter teachers' scale in 1989, 2.8 times as likely if the child had a high score on the CDI, 2.4 times as likely if the child was male, and 5.7 times as likely if the child was from a family of low socioeconomic status.
Discussion and conclusions
The results of this study suggest that the psychiatric problems of children that lead to referral or consideration for referral by the age of 12 already exist when the child is in early elementary school. In our study, children who had been referred or considered for referral by age 12 had scored in the deviant range on the Rutter teachers' scale and the CDI four years earlier. In addition, the child's gender and socioeconomic class appeared to be related to referral or consideration for referral.
To our knowledge, this study is the first to show that referrals of children for psychiatric evaluations that are initiated by school professionals can be predicted on the basis of psychiatric symptoms and deviant behavior assessed four years earlier. The strengths of this study include its longitudinal, prospective, and epidemiological design, the large representative sample of children, and the high response rate. Moreover, the methods used are well documented, and the instruments are considered to be reliable for studying the general population (15,16), although questionnaires have known limitations. It should be noted that because the study examined eight-year-old children and outcomes four years later, the results may not be generalizable to other age groups.
Only a small proportion of the children in the sample were referred for evaluation or considered for referral, which was expected. A considerable number of children who need psychiatric evaluation and treatment do not receive professional help (5,8,17-19). Our study differs from previous studies in its focus on referral specifically by teachers. However, our findings are broadly in line with those of other studies that investigated children's use of mental health services and related factors (2,5,20).
The results suggest that teachers are not very active in initiating referrals, as has been found to be the case among general practitioners and pediatricians (21,22). Goodman (23) suggested that parents and teachers experience growing concern as symptoms persist but that they are pessimistic about the success of treatment and see symptoms as personality traits rather than reversible states. This notion might be applicable to our sample. Teachers may have felt troubled by the behavior of certain children but may not have made an effort to contact mental health services for these reasons.
The scores of the referred children were higher in 1989 and 1993 than the scores of children considered for referral and the scores of other children. This finding is consistent with results of other studies in which the mean number of symptoms was higher among referred children than among other children (9). In our study the scores of referred children and of those considered for referral were similar, which supports the idea that factors other than the number of current psychiatric symptoms affect judgments about whether psychiatric consultation is needed.
The finding that children from families of lower socioeconomic status were more likely to be referred or considered for referral cannot be explained by the data in our study. Some researchers have suggested that the association between socioeconomic status and referral is related to the availability of services. However, children's mental health services are equally available to all socioeconomic groups in Finland, and at the time of the study private services for children in the study area were practically nonexistent. Thus other factors are probably more important.
Teachers may be more likely to consider referring children from families of lower socioeconomic status. In addition, they may assume that families of higher socioeconomic status will contact the services themselves without any interference from the teacher. A study by Garralda and Bailey (9) found that children referred for psychiatric evaluations were more likely to be from socioeconomically disadvantaged families. Koot and Verhulst (8) reported a similar association between socioeconomic status and referral of children to mental health services.
The results of our study suggest that gender influences whether a child is considered for referral but not whether the child is actually referred. Similar findings have been reported by researchers in the Netherlands (5,8). In general, boys outnumber girls among children who are referred to mental health or social service agencies or who have been in contact with such agencies (1,9). Boys also outnumber girls in inpatient psychiatric settings (24).
However, the predominance of boys has been noted in studies of clinical populations or populations that are not purely epidemiological. An epidemiological setting is far more suitable for studying whether boys are more likely to be considered for referral but not actually referred. Szatmari and colleagues (25) observed that studies of community samples are potentially more informative if the aim is to determine the correlates of a psychiatric disorder. Their observation arguably applies to studies of referral for psychiatric consultation. Only studies based on epidemiological data can simultaneously take into account referral, psychiatric symptoms, and deviant behavior in the community, which is the approach needed to determine whether children with certain types of psychiatric problems are more likely to be referred irrespective of gender. Some interaction between referral, psychiatric symptoms, deviant behavior, and gender may occur; however, we could not conduct an analysis of this interaction because our sample was too small to permit firm conclusions. This issue warrants further research with large epidemiological samples.
Boys may have been more frequently considered for referral because of the burden caused by externalizing symptoms and problems, which are more common among boys (26). Achenbach and associates (26) have suggested that the higher rate of referral to mental health services among boys may result from the conflicts between boys' behavior and accepted norms rather than from quantitative differences in the psychiatric problems of boys and girls. Our findings support this explanation.
Children who scored high on the self-rated depression scale also were more likely to be considered for referral. In these cases, the teachers seemed to realize that something was wrong with the child and considered referral, but they eventually decided that the problem did not justify it. This finding again shows that the severity of the burden and stress that adults experience as a result of a child's behavior strongly influence which children will gain access to mental health services and which will not, even among children having a roughly equal number of psychiatric symptoms (3,9,23).
These results also highlight the adult orientation of children's services. The younger the child is, the more he or she depends on adults to ensure that needed services are provided. We cannot assume that children of elementary school age are capable of seeking out services for themselves. Adults must take responsibility for referral. Teachers and school health professionals should receive more education about child development and psychiatric problems. In particular, they should have opportunities to practice the skills needed to deal with psychiatric problems that arise in the classroom.
Collaboration between many agencies is needed to ensure that relevant services are delivered to children promptly and effectively. Many children would benefit from early intervention in schools and primary health care settings. Such an approach may prevent the need for more specialized services later. Furthermore, mental health services should be more readily available at school so that children themselves can initiate a consultation. School-based services would also be less stigmatizing than more specialized services located elsewhere. Psychiatric problems interfere with scholastic achievement, and thus they can have long-term effects on adult life. Efforts to identify such problems early are clearly in the best interests of children.
Dr. Kumpulainen is affiliated with the department of child psychiatry at Kuopio University Hospital, P.O.B. 1777, Fin-70211, Kuopio, Finland (e-mail, [email protected]). Dr. Räsänen is with the department of child psychiatry at Kuopio University.
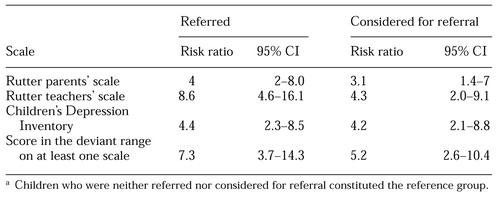 |
Table 1. Relative risk of having a score in the deviant range on three scales among eight-year-old children who were found by age 12 to have been referred for a psychiatric evaluation or considered for referrala
a Children who were neither referred nor considered for referral constituted the reference group
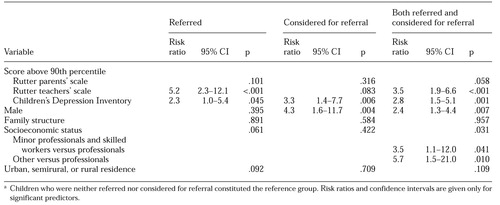 |
Table 2. Variables assessed among eight-year-old children by logistic regression analysis for their significance as predictors of referral for a psychiatric evaluation or consideration for referral by age 12a
a Children who were neither referred nor considered for referral constituted the reference groupRisk ratios and confidence intervals are given only for significant predictors.
1. Costello EJ, Janiszewski S: Who gets treated? Factors associated with referral in children with psychiatric disorders. Acta Psychiatrica Scandinavica 81:523-529, 1990Crossref, Medline, Google Scholar
2. Leaf PJ, Algeria MA, Cohen P, et al: Mental health service use in the community and schools: results from the four-community MECA study. Journal of the American Academy of Child and Adolescent Psychiatry 35:889-897, 1996Crossref, Medline, Google Scholar
3. Angold A, Masser SC, Stangl D, et al: Perceived parental burden and service use for child and adolescent psychiatric disorders. American Journal of Public Health 88:75-80, 1998Crossref, Medline, Google Scholar
4. Dumas JE: Why was this child referred? Interactional correlates of referral status in families of children with disruptive behavior problems. Journal of Clinical Child Psychology 25:106-115, 1996Crossref, Google Scholar
5. Verhulst FC, van der Ende J: Factors associated with child mental health service use in the community. Journal of the American Academy of Child and Adolescent Psychiatry 36:901-909, 1997Crossref, Medline, Google Scholar
6. Anderson JC, Williams S, McGee R, et al: DSM-III disorders in preadolescent children. Archives of General Psychiatry 44:69-76, 1987Crossref, Medline, Google Scholar
7. Kumpulainen K, Räsänen E, Henttonen I, et al: Bullying and psychiatric symptoms among elementary school-age children. Child Abuse and Neglect 22:705-717, 1998Crossref, Medline, Google Scholar
8. Koot HM, Verhulst FC: Prediction of children's referral to mental health and special education services from earlier adjustment. Journal of Child Psychology and Psychiatry 33:717-729, 1992Crossref, Medline, Google Scholar
9. Garralda ME, Bailey D: Child and family factors associated with referral to child psychiatrists? British Journal of Psychiatry 153:81-89, 1988Google Scholar
10. Kumpulainen K, Räsänen E, Henttonen I: The persistence of psychiatric disturbance among children. Social Psychiatry and Psychiatric Epidemiology 32:113-122, 1997Medline, Google Scholar
11. Rutter M, Tizard J, Whitmore K: Education, Health, and Behaviour. London, Longman, 1970Google Scholar
12. Rutter M: A children's behaviour questionnaire for completion by teachers: preliminary findings. Journal of Child Psychology and Psychiatry 8:1-11, 1967Crossref, Medline, Google Scholar
13. Kovacs M: Rating scales to assess depression in school-aged children. Acta Paedopsychiatrica 46:305-315, 1980Google Scholar
14. Kovacs M: Children's Depression Inventory. New York, MHS, 1992Google Scholar
15. Elander J, Rutter M: An update on the status of the Rutter Parents' and Teachers' Scales. Child Psychology and Psychiatry Review 31-35, 1996Google Scholar
16. Elander J, Rutter M: Use and development of the Rutter Parents' and Teachers' Scales. International Journal of Methods in Psychiatric Research 6:63-78, 1996Crossref, Google Scholar
17. Ikäheimo K: Lastenpsykiatrinen hoitoonohjautumisprosessi [the child psychiatric referral process]. In Finnish, with English summary. Doctoral dissertation, Department of Child Psychiatry, Turku, Finland, Turku University Publications, 1999Google Scholar
18. Offord DR, Boyle MH, Szatmari P, et al: Ontario Child Health Study: II. six-month prevalence of disorders and rates of service utilization. Archives of General Psychiatry 44:832-836, 1987Crossref, Medline, Google Scholar
19. Wu P, Hoven CW, Bird HR, et al: Depressive and disruptive disorders and mental health service utilization in children and adolescents. Journal of the American Academy of Child and Adolescent Psychiatry 38:1081-1090, 1999Crossref, Medline, Google Scholar
20. Zahner GEP, Pawelkiewicz W, DeFrancesco JJ, et al: Children's mental health service needs and utilization patterns in an urban community: an epidemiological assessment. Journal of the American Academy of Child and Adolescent Psychiatry 31:951-960, 1992Crossref, Medline, Google Scholar
21. Costello EJ: Primary care pediatrics and child psychopathology: a review of diagnostic, treatment, and referral practices. Pediatrics 78:1044-1051, 1986Medline, Google Scholar
22. Bailey D, Garralda ME: Referral to child psychiatry: parent and doctor motives and expectations. Journal of Child Psychology and Psychiatry 30:449-458, 1989Crossref, Medline, Google Scholar
23. Goodman R: The extended version of the Strengths and Difficulties Questionnaire as a guide to child psychiatric caseness and consequent burden. Journal of Child Psychology and Psychiatry 40:791-799, 1999Crossref, Medline, Google Scholar
24. Piha J, Spurkland I: Portraits of child psychiatric inpatient treatment in Finland and Norway. European Child and Adolescent Psychiatry 1:201-208, 1992Crossref, Google Scholar
25. Szatmari P, Offord DR, Boyle MH: Correlates, associated impairments, and patterns of service utilization of children with attention deficit disorder: findings from the Ontario Child Health Study. Journal of Child Psychology and Psychiatry 30:205-217, 1989Crossref, Medline, Google Scholar
26. Achenbach TM, McConaughy SH, Howell CT: Child/adolescent behavioral and emotional problems: implications of cross-informant correlations for situational specificity. Psychological Bulletin 101:213-232, 1987Crossref, Medline, Google Scholar



