Management of Negative Symptoms Among Patients With Schizophrenia Attending Multiple-Family Groups
Abstract
OBJECTIVE: Outcomes for negative symptoms over a one-year period were examined in two groups of patients, one receiving psychoeducational multiple-family group treatment and one receiving standard care. METHODS: A total of 63 outpatients, ages 18 to 45 years, with DSM-IV diagnoses of schizophrenic disorders were randomly assigned to standard care or multiple-family group psychoeducation treatment at a large mental health center in Spokane, Washington. Treatment assignment was stratified by whether patients were taking typical or atypical antipsychotic medications. Negative symptom status was monitored monthly for one year by raters blind to group assignment and measured as a composite of five symptoms using the Modified Scale for the Assessment of Negative Symptoms. RESULTS: When the analysis controlled for baseline negative symptoms, participants in the multiple-family group experienced significantly reduced negative symptoms compared with those receiving standard care. Taking atypical antipsychotic medication or having a diagnosis of substance abuse was not associated with the severity of negative symptoms. An additional analysis of the five individual negative symptoms indicated small but consistent group differences on all dimensions except inattention. Negative symptoms were significantly correlated with relapse to acute illness but not with outpatient or inpatient service use. CONCLUSIONS: The study demonstrated that a psychoeducational multiple-family group intervention was more effective than standard care in managing negative symptoms over a 12-month period. The results are particularly relevant because negative symptoms are associated with relapse, poor social and occupational functioning, cognitive impairment, and lower subjective quality of life.
Support is growing for the efficacy and cost-effectiveness of family psychoeducation in the management of schizophrenia, particularly in preventing relapse and rehospitalization (1,2,3,4,5,6,7,8). Common elements in a number of psychoeducational approaches include engagement of the family as an ally in the treatment process and presentation of detailed information about schizophrenia and its management, such as improving communication, problem solving, medication compliance, and crisis intervention and developing social support networks and coping skills (9,10).
One psychoeducational approach, the multiple-family group, was recently developed by McFarlane and colleagues (7,8). It borrows heavily from the work of Hogarty and colleagues (3) and Falloon and associates (2). The multiple-family group format consists of a group of six to eight families, including the identified patients. The group is directed by two clinicians. A formal multisite evaluation of the effectiveness of the multiple-family group approach with a large sample indicated that compared with the single-family format, the multiple-family group approach significantly extended remission over a four-year period (7).
Results thus far support the effectiveness of psychoeducation and support interventions in managing the positive symptoms of schizophrenia. However, little investigation has been done of the impact on negative symptoms. One exception is a study by McFarlane and colleagues (8), who reported a reduction in negative symptoms in a sample of acutely psychotic inpatients. Between index admission and discharge, patients receiving the multiple-family group intervention evidenced a greater reduction in negative symptoms than did patients in the single-family format.
Several other psychosocial interventions have been shown to be effective in reducing negative symptoms (11,12,13); however, many of these studies did not include a control group. The report by Halford and colleagues (12) is representative. Although they found improvement in negative symptoms and quality of life among chronic patients after a broad psychoeducational rehabilitation program, the study was small, did not include a control group, and included patients who had been diagnosed as having affective disorder with psychotic features.
The shortage of research examining the impact of psychoeducational approaches on negative symptoms may partly reflect the use of study methods that favor the selection of patients with a high level of positive symptoms. That is, participants in family education and support studies typically enter the studies while they are inpatients in an acute exacerbation stage of their illness.
Although it is an oversimplification to divide schizophrenia into positive and negative symptoms (14), these terms refer descriptively to exaggerations and losses of normal function, respectively. Positive symptoms are the florid symptoms associated with exacerbations of the illness, whereas negative symptoms tend to have a more basic underlying persistence (14,15,16). Negative symptoms as measured by the Modified Scale for the Assessment of Negative Symptoms (MSANS) (17) include the following five features: affective flattening, anhedonia, avolition-apathy, alogia, and attentional impairment. Besides being more stable over time than the more episodic positive symptoms, negative symptoms are associated with a variety of functional difficulties, including social and vocational impairment (18,19,20,21), cognitive impairment (22), lower quality of life (23,24), and poor long-term prognosis (25,26,27).
Despite the importance of negative symptoms, as Halford and Hayes (28) observed, it is unclear whether aspects of schizophrenic symptoms other than those observed at relapse respond to family psychoeducation. They outlined three possible outcome patterns. First, negative symptoms might not be responsive to psychologically based interventions, simply because they are diagnostic of a chronic course (29). Second, negative symptoms that result from underlying neurological impairments may be refractory to psychologically based treatments (30). Third, negative symptoms might be highly responsive to interventions that target problem solving and communication skills (31).
The study reported here builds on earlier work with acutely psychotic patients by applying the multiple-family group intervention to relatively stable outpatients. Given that negative symptoms can be unstable in acutely ill patients (32), the sample was believed to be ideally suited to evaluate the impact of the intervention on chronic schizophrenia and, perhaps, persistent negative symptoms. Accordingly, we compared participants who had been randomly assigned to the multiple-family group or standard care during the first year of a two-year intervention.
The protocol included full specification of the multiple-family group intervention in a treatment manual, extensive training, close supervision of experienced clinicians at the field site, and measures of patient outcomes. The primary symptom measures were collected monthly during the two-year period. The main hypothesis tested was that when the analysis controlled for baseline symptoms (using baseline scores as a covariate) and for whether a patient was taking an atypical antipsychotic, patients receiving the multiple-family group intervention would be more likely to have reduced negative symptom scores than those receiving standard care over the 12-month period.
Methods
Subjects and sample
The criteria for inclusion in the study were a diagnosis of schizophrenia or schizoaffective disorder according to DSM-IV criteria (33), age between 18 and 45 years, enrollment for mental health services in a community outpatient facility (Spokane Mental Health), residence with the family of origin or in regular contact with the family, patient and family consent to participate, and minimum attendance by one family member for at least five face-to-face contacts. Patients with either a history of substance abuse or current substance abuse were not excluded.
Table 1 presents demographic characteristics of the total sample, which included 63 outpatients receiving treatment at a large mental health center in Spokane, Washington. The mean age of the clients was 33 years. Most were Caucasian males who had been in and out of the hospital five times over ten years of illness. Two-thirds of the sample were on atypical antipsychotics at baseline.
Measures taken during baseline suggested that, on average, participants had very mild positive symptoms as measured by the Brief Psychiatric Rating Scale (BPRS) and slightly greater than mild negative symptoms as measured by the MSANS. Five items from the BPRS were used to measure positive symptoms. Possible total scores range from 5, indicating no symptoms, to 35, indicating severe symptoms. The five-item MSANS composite score measuring negative symptoms could range from 5, indicating no symptoms, to 25, indicating severe symptoms.
Local university and state institutional review boards approved the study. Participants were recruited in cohorts of 14 to 18 persons between February 1996 and March 1997 and randomly assigned by cohort to a treatment group after the diagnostic and baseline assessments. Medication status—atypical versus conventional antipsychotic—was stratified within each cohort so that an equal number of persons in the multiple-family group and the standard-care group were on atypical medications such as clozapine, risperidone, and olanzapine.
Treatments
Standard care. The outpatients assigned randomly to standard care received the usual services provided to Spokane Mental Health clients. These services were delivered by a treatment team consisting of a case manager, nurse, psychiatrist, and social worker in a long-term track for persons with severe and persistent mental illness. They included medication management, case management, and, for some, therapeutic and rehabilitative services. The client's case management team provided clinical case management and out-of-facility services when they were needed. Rehabilitative services included a work-ordered day program, a social program on evenings and weekends, and a supported employment program.
Multiple-family group intervention. The multiple-family group treatment, which was superimposed on standard care, was designed to help families and patients improve their coping and illness management skills. This general strategy was derived from work previously reported by Goldstein and associates (1), Falloon and colleagues (2), Hogarty and coworkers (3), and Leff and associates (6).
Specific treatment interventions implemented by multiple-family group clinicians were designed to engage key members of the family; provide information about the biologic aspects of schizophrenia and the treatment process using a standardized videotape, lectures, and written guidelines for coping; intervene early in incipient relapse; provide ongoing support and formal clinical problem solving for at least two years; and expand the family's social network.
The two family clinicians who led the group were selected on the basis of interest, clinical skills, and educational level. One had a bachelor's degree, and the other a master's degree. Multiple-family group clinicians were expected to function as the family's educator and consultant, as a coleader of the multiple-family group treatment sessions, and as the principal liaison to the patient's case manager and other treatment team members.
The multiple-family group protocol began with the two family clinicians' each meeting separately with three or four families, without the patients' being present, for three weekly single-family sessions. These sessions started within several weeks to a month after the patient and family gave informed consent. The two clinicians, the principal investigator, and the project psychiatrist then presented an educational workshop for these six to eight families together, again without the patients. This presentation was modeled on the survival skills workshop developed by Anderson and colleagues (34).
Two weeks later, six families in the multiple-family group began to meet biweekly with the patients present, led by the two family clinicians. Meetings were organized around a formal problem-solving procedure designed to develop individualized coping methods; the problem-solving procedures were derived from suggestions by group members. The multiple-family group model has been described elsewhere (8).
Family clinician training and supervision
Each family clinician read the treatment manual and was trained by the clinical supervisors. Training and monitoring for fidelity to the model consisted of systematic review of videotapes by the study supervisors of all family-engagement sessions and every multiple-family group meeting throughout the study period. Supervision occurred weekly by telephone consultation and through additional annual on-site supervision visits. Although clinicians were not required to meet competency criteria, supervision was especially intense during the initial phases of each group. Two multiple-family group clinicians were assigned to each of the first four cohorts.
Diagnosis
The Psychotic Disorders version of the Structured Clinical Interview for DSM-IV (SCID-PD) was completed after the patient gave informed consent. Experienced raters also rated positive and negative symptoms.
Positive and negative symptoms
The interviewers measured positive and negative symptoms monthly. The MSANS contains 30 items that assess alogia, affective blunting, asociality-anhedonia, avolition, and inattention (17). The raters participated in training sessions for rating accuracy and reliability. The BPRS contains 24 items assessing both positive and negative symptoms (35).
Data analysis
Data analysis was conducted in three stages. The first stage summarized descriptive characteristics of the participants and positive and negative symptoms. The second stage assessed the change in the sum of the five MSANS global ratings averaged over four successive three-month time frames during one year. The scores were analyzed using an analysis of covariance (ANCOVA), which assessed differences while controlling for baseline MSANS scores. Other factors in the analysis were medications (atypical versus conventional) and substance abuse (yes or no). The third stage analyzed group differences on each of the five individual negative symptoms. We also computed correlations between mean score for negative symptoms at one year, relapse (a rating of 4 or higher for one of the five psychotic items on the BPRS for two successive months), and outpatient service utilization (minutes per month).
This analysis was based on 42 participants who received treatment for the full 12 months. Of the 63 participants assessed at baseline, 54 were randomly assigned to the study groups and completed at least one postbaseline assessment. An additional 12 participants dropped out of the study during the first year—six from the multiple-family groups and six from standard care. The MSANS scores of the dropouts did not differ significantly from the scores of those who completed treatment. After the manuscript was submitted, we conducted analyses on a larger sample of six cohorts (N=83). An analysis of 70 participants who received at least six months of multiple-family group treatment (N=35) or standard care (N=35) showed a significant effect of group treatment (F=3.7, df=1,67, p=.05). Other analyses indicated that group differences were not detected among participants who received less than six months of standard care or multiple-family group treatment.
Results
As shown in Table 1 the participants were in their early thirties and predominantly male. Approximately two- thirds were on atypical medications at study entry, and 48 percent met criteria for DSM-IV-defined substance abuse disorder. Summed baseline scores on the five-item MSANS measure indicated that the groups did not differ in negative symptoms. Participants did not differ on any of the remaining variables shown in Table 1.
Table 2 presents MSANS scores of the multiple-family group and the standard-care group at baseline and for the next 12 months. A mixed-design, repeated-measures ANCOVA with one covariate (baseline MSANS scores), three between factors (group by medication type by substance abuse), and one within factor (the four three-month blocks) was performed on the composite MSANS scores. This analysis yielded a significant effect of group treatment (F=6.1, df=1,39, p<.05), indicating that multiple-family group participants had reduced negative symptoms compared with standard-care participants. None of the other main effects or interactions were significant.
To obtain a more detailed look at the negative symptom components, identical analyses were conducted separately on the mean ratings for each of the five symptoms. Because these analyses were based on a single item, they were less reliable than the analysis on the composite measure, and although the results were consistent with the results of the composite measures, they were less robust. Marginally significant effects were observed on the avolition item (F=3.9, df=1,39, p=.05), the flattening item (F=.7, df=1,39, p=.10), the alogia item (F=2.6, df=1,39, p=.11), and the asociality items (F=2.2, df=1,39, p=.14). Inattention was clearly not affected.
Finally, the relationship of negative symptoms to relapse and service utilization was examined. Although no relationship was noted between negative symptoms and outpatient service use or total hospitalization days, the one-year mean score on negative symptoms was significantly associated with occurrence of relapse (r=.47, p<.00l).
Discussion and conclusions
As noted in the introduction, considerable evidence has been found that psychoeducational multiple-family groups are effective in reducing relapse and rehospitalization. Indeed, the inclusion of family education as a best practice in the Schizophrenia PORT Project (36) is an indication of the empirical support for this intervention. On the other hand, little support has been found for the efficacy and effectiveness of psychosocial interventions on the negative symptoms of schizophrenia.
The results of this study indicate that psychoeducational multiple-family groups contribute to the management of negative symptoms in schizophrenia. These results are consistent with those of two other psychosocial intervention studies. The first was by Halford and colleagues (12), which found significant improvement in negative symptoms and quality of life among chronic patients after participation in a non-family-based psychoeducational rehabilitation program. The second study, by McFarlane and associates (8), was of acutely psychotic inpatients from admission to discharge. Compared with patients who participated in a single-family format, those in multiple-family groups experienced a reduction in negative symptoms.
Although the results reported here indicate that the multiple-family group intervention was associated with reductions in negative symptom, no effect was found for either atypical medications or substance abuse status. The failure to find effects due to atypical medications is at variance with several studies that have reported such effects with clozapine (37) and risperidone (38); however, participants in the study reported here were stratified, not randomized, on this variable.
Several aspects of this study warrant comment. First, the results were observed in a large community mental health center that provided services under a capitated managed care contract, an increasingly common outpatient arrangement and financial context. Second, the originators of the treatment did not provide the multiple-family group intervention in our study. In this respect our study is methodologically similar to a recent investigation by Schooler and colleagues (39) and represents an important intermediate step between the development and delivery of a novel intervention and dissemination into routine treatment.
Mechanism of action
Although further research is needed to investigate the mechanisms of action, the observed improvements in negative symptoms may reflect the fact that family psychoeducation serves to broaden and enrich the social environment of consumers and families alike. Such an interpretation is consistent with the observation that negative symptoms are more common in nonstimulating settings and less severe after enrichment of the social environment (40). The interpretation is also congruent with the view that social factors have a central role in the genesis of negative symptoms (41).
Social skills training has been demonstrated to have a significant effect on a cluster of negative symptoms, including poor rapport, social avoidance, poor flow of conversation, and emotional withdrawal (1,42). The socialization component of the multiple-family group intervention provides consumers with repeated exposure to persons who model normal social interactions. As consumers experience increased levels of support within the group, their social engagement skills improve.
In addition, the content of the family guidelines, such as lowered expectations and clear communications, and the problem-solving format of the multiple-family group intervention may also contribute to reductions in negative symptoms. Educating participants about negative symptoms reduces the family's tendency to criticize the consumer, which in turn encourages social engagement. Further, the emphasis on setting realistic limits and clear communications contributes to maintaining a low-key environment with structure and stability. The predictable environment together with the graded-task assignments developed through problem solving could conceivably lead to improved activation and motivation among consumers, by providing more opportunities for success. As participants in standard care received as many outpatient service hours as participants in the multiple-family group intervention, we attribute the difference in results to the difference in the focus of treatment.
The impact of the multiple-family group intervention on negative symptoms might also be related to treatment adherence variables such as attendance and medication compliance. To examine this possibility further, we conducted additional analyses of the relationships between negative symptoms and treatment adherence over time. The analyses on attendance indicated that participants in multiple-family groups attended a mean±SD of 16±11 sessions. The correlation coefficients between attendance and MSANS scores (averaged over three-month intervals) indicated that attendance was associated with reduced negative symptoms. This effect increased over time; significance was attained at the ten- to 12-month interval (r=−.56, df=32, p<.01). Similar analyses of the relationship between medication compliance and negative symptoms showed nonsignificant trends in the expected direction.
Taken together, the data suggest that the mechanism of negative symptom reduction is directly related to the level of participation by consumers in multiple-family groups, presumably through direct exposure to social interactions and practice at social engagement and related skill development.
Clinical significance
The effects observed here are clinically significant because negative symptoms often prevent patients with chronic schizophrenia from being actively involved in psychosocial rehabilitation and complicate the transition to independent living in the community (43). Such symptoms profoundly interfere with the social and vocational functioning so necessary for successful community living and are concurrently correlated with poor community functioning (43). In addition, recent studies have shown that negative symptoms are significantly associated with subjective quality of life (23,24). In the study reported here, negative symptoms were significantly correlated with the occurrence of relapse (r=.47, p<.01).
Although the research literature clearly indicates that control of negative symptoms should be a clinical priority, the quiet nature of these symptoms together with the current emphasis on managing health care costs brings with it the danger of according them second-class priority. Despite their significance, negative symptoms are not the "squeaky wheel" of schizophrenia. Consistent with this view, persons in the sample with high levels of negative symptoms did not receive any more outpatient service hours than did those who had low levels. Indeed, the correlation during the first year of the study between mean MSANS scores and total outpatient staff time was -.03.
Given that recent studies have shown that negative symptoms are significantly associated with subjective quality of life, it is reasonable to expect that multiple-family groups may improve quality of life, particularly in the social and family relations domain.
Acknowledgments
This research was supported by grant R01-MH-52259 from the National Institute of Mental health to the first author. The authors thank Lori Pinter for participation as a multifamily group clinician and supervisor and Bonnie Horen for supervision.
Dr. Dyck, Dr. Short, Dr. Hendryx, Ms. Norell, Dr. Meyers, Mr. McDonnell, and Mr. Voss are affiliated with the Washington Institute for Mental Illness Research and Training, P.O. Box A, Medical Lake, Washington 99022-0045 (e-mail, [email protected]). Dr. Dyck, Dr. Short, Dr. Hendryx, Mr. McDonell, and Mr. Voss are also affiliated with Washington State University in Spokane. Ms. Norell is also affiliated with Eastern State Hospital in Medical Lake, Washington. Dr. Myers and Dr. Patterson are with Spokane Mental Health. Dr. McFarlane is with the Maine Medical Center in Portland.
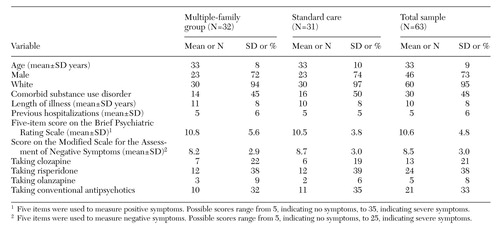 |
Table 1. Baseline characteristics of 63 patients with schizophrenia randomly assigned to a multiple-family group or standard care
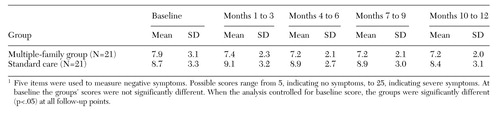 |
Table 2. Mean scores on the Modified Scale for the Assessment of Negative Symptoms at baseline and over a 12-month follow-up of patients with schizophrenia randomly assigned to a multiple-family group or standard care1
1. Goldstein MJ, Rodnick EH, Evans JR, et al: Drug and family therapy in the aftercare treatment of acute schizophrenics. Archives of General Psychiatry 35:1169-1177, 1978Crossref, Medline, Google Scholar
2. Falloon IRH, Boyd JL, McGill CW, et al: Family management in the prevention of morbidity of schizophrenia: clinical outcome of a two-year longitudinal study. Archives of General Psychiatry 42:887-896, 1985Crossref, Medline, Google Scholar
3. Hogarty GE, Anderson CM, Reiss DJ, et al: Family psychoeducation, social skills training, and maintenance chemotherapy in the aftercare treatment of schizophrenia: II. two-year effects of a controlled study on relapse and adjustment. Archives of General Psychiatry 48:340-347, 1991Crossref, Medline, Google Scholar
4. Leff J, Kuipers L, Berkowitz R, et al: A controlled trial of social intervention in the families of schizophrenic patients: two year follow-up. British Journal of Psychiatry 146:594-600, 1985Crossref, Medline, Google Scholar
5. Tarrier N, Barrowclough C, Vaughn C, et al: Community management of schizophrenia: a two-year follow-up of a behavioral intervention with families. British Journal of Psychiatry 154:625-628, 1989Crossref, Medline, Google Scholar
6. Leff J, Berkowitz R, Shavit N, et al: A trial of family v a relatives group for schizophrenia. British Journal of Psychiatry 154:58-66, 1989Crossref, Medline, Google Scholar
7. McFarlane WR, Link B, Dushay R, et al: Psychoeducational multiple family groups: four-year relapse outcome in schizophrenia. Family Processes 34:127-144, 1995Crossref, Medline, Google Scholar
8. McFarlane WR, Lukens E, Dushay R, et al: Multiple family group and psychoeducation in the treatment of schizophrenia. Archives of General Psychiatry 52:679-687, 1995Crossref, Medline, Google Scholar
9. Goldstein MJ: Psychoeducation family programs in the United States, in Handbook of Mental Health Economics and Health Policy, Vol 1: Schizophrenia. Edited by Moscarelli M, Rupp A, Sartorius N. New York, Wiley, 1996Google Scholar
10. Gingerich SL, Bellack AS: Research-based family interventions for the treatment of schizophrenia. Research on Social Work Practice 6:122-126, 1996Crossref, Google Scholar
11. Grace J, Bellus SB, Raulin ML, et al: Long-term impact of clozapine and psychosocial treatment on psychiatric symptoms and cognitive functioning. Psychiatric Services 47:41-45, 1996Link, Google Scholar
12. Halford WK, Harrison C, Kalyansundaram, et al: Preliminary results from a psychoeducational program to rehabilitate chronic patients. Psychiatric Services 46:1189-1191, 1995Link, Google Scholar
13. Inch R, Crossley M, Keegan D, et al: Use of the Brief Psychiatric Rating Scale to measure success in a psychosocial day program. Psychiatric Services 48:1195-1197, 1997Link, Google Scholar
14. Andreasen NE, Arndt S, Alliger R, et al: Symptoms of schizophrenia: methods, meanings, mechanisms. Archives of General Psychiatry 52:341-351, 1995Crossref, Medline, Google Scholar
15. Arndt S, Andreasen NC, Flaum M, et al: A longitudinal study of symptom dimensions in schizophrenia. Archives of General Psychiatry 52:352-360, 1995Crossref, Medline, Google Scholar
16. Pogue-Geile MF, Harrow M: Negative symptoms in schizophrenia: their longitudinal course and prognostic importance. Schizophrenia Bulletin 11:427-439, 1985Crossref, Medline, Google Scholar
17. Andreasen NC: Modified Scale for the Assessment of Negative Symptoms. Rockville, Md, National Institute of Mental Health, 1984Google Scholar
18. Glynn SM, Randolph ET, Eth S, et al: Schizophrenic symptoms, work adjustment, and behavioral family therapy. Rehabilitation Psychology 37:323-339, 1992Crossref, Google Scholar
19. Hamilton NG, Ponzoha CA, Cutler DL, et al: Social networks and negative versus positive symptoms of schizophrenia. Schizophrenia Bulletin 15:625-633, 1989Crossref, Medline, Google Scholar
20. Lysaker P, Bell M: Negative symptoms and vocational impairment in schizophrenia: repeated measurements of work performance over six months. Acta Psychiatrica Scandinavica 91:205-208, 1995Crossref, Medline, Google Scholar
21. Pogue-Geile MF, Harrow M: Negative and positive symptoms in schizophrenia and depression: a follow-up. Schizophrenia Bulletin 10:371-387, 1984Crossref, Medline, Google Scholar
22. Nuechterlein KH, Edell WS, Norris M, et al: Attentional vulnerability indicators, thought disorder, and negative symptoms. Schizophrenia Bulletin 12:408-426, 1986Crossref, Medline, Google Scholar
23. Browne S, Roe M, Lane A, et al: Quality of life in schizophrenia: relationship to sociodemographic factors, symptomatology, and tardive dyskinesia. Acta Psychiatrica Scandinavica 94:118-124, 1996Crossref, Medline, Google Scholar
24. Packer S, Husted J, Cohen S, et al: Psychopathology and quality of life in schizophrenia. Journal of Psychiatry and Neuroscience 22:231-234, 1997Medline, Google Scholar
25. Fenton WS, McGlashan TH: Natural history of schizophrenia subtypes: II. positive and negative symptoms and long-term course. Archives of General Psychiatry 48:978-986, 1991Crossref, Medline, Google Scholar
26. Knight RA, Roff JD: Affectivity in schizophrenia, in Controversies in Schizophrenia: Changes and Constancies. Edited by Alpert M. New York, Guilford, 1985Google Scholar
27. Pogue-Geile MF, Harrow M: Negative symptoms in schizophrenia: longitudinal characteristics and etiological hypotheses, in Positive and Negative Symptoms of Psychosis. Edited by Harvey PD, Walker EF. Hillsdale, NJ, Erlbaum, 1987Google Scholar
28. Halford WK, Hayes R: Psychological rehabilitation of chronic schizophrenic patients: recent findings on social skills training and family psychoeducation. Clinical Psychology Review 23:23-44, 1991Crossref, Google Scholar
29. Crow TJ: The two-syndrome concept: origins and current status. Schizophrenia Bulletin 11:471-485, 1985Crossref, Medline, Google Scholar
30. Morrison RL, Bellack AS, Wixted JT, et al: Positive and negative symptoms in schizophrenia: a cluster-analytic approach. Journal of Nervous and Mental Disease 178:377-384, 1990Crossref, Medline, Google Scholar
31. Anthony WA, Liberman RP: The practice of psychiatric rehabilitation: historical, conceptual, and research base. Schizophrenia Bulletin 12:542-559, 1986Crossref, Medline, Google Scholar
32. Lyndemayer JP, Kay SR, Friedman C: Negative and positive schizophrenic syndromes after the acute phase: a prospective follow-up. Comprehensive Psychiatry 27:276-286, 1986Crossref, Medline, Google Scholar
33. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC, American Psychiatric Association, 1994Google Scholar
34. Anderson CM, Hogarty G, Reiss DJ: Family treatment of adult schizophrenic patients: a psycho-educational approach. Schizophrenia Bulletin 6:490-505, 1980Crossref, Medline, Google Scholar
35. Overall JE, Gorham DR: The Brief Psychiatric Rating Scale. Psychological Reports 10:799-812, 1962Crossref, Google Scholar
36. Lehman AF, Steinwachs DM: Translating research into practice: the Schizophrenia Patient Outcomes Research Team (PORT) treatment recommendations. Schizophrenia Bulletin 24:1-10, 1998Crossref, Medline, Google Scholar
37. Breier A, Buchanan R, Kirpatrick B, et al: Effects of clozapine on positive and negative symptoms in outpatients with schizophrenia. American Journal of Psychiatry 151:20-26, 1994Link, Google Scholar
38. Möller H, Müller H, Borison R, et al: A path-analytical approach to differentiate between direct and indirect drug effects on negative symptoms in schizophrenic patients: a re-evaluation of the North American risperidone study. European Archives of Psychiatry and Clinical Neuroscience 245:45-49, 1995Crossref, Medline, Google Scholar
39. Schooler N, Keith SJ, Severe JB, et al: Relapse and rehospitalization during maintenance treatment of schizophrenia. Archives of General Psychiatry 54:453-463, 1997Crossref, Medline, Google Scholar
40. Wing JK: Psychosocial factors influencing the onset and course of schizophrenia, in Psychoses of Uncertain Aetiology. Edited by Wing JK, Wing L. Cambridge, England, Cambridge University Press, 1982Google Scholar
41. Wing JK, Brown GW: Institutionalism and Schizophrenia. Cambridge, England, Cambridge University Press, 1970Google Scholar
42. Dobson DJG, McDougall G, Blusheikin J, et al: Effects of social skills training and social milieu treatment on symptoms of schizophrenia. Psychiatric Services 46:376-380, 1995Link, Google Scholar
43. Pogue-Geile MF, Zubin J: Negative symptomatology and schizophrenia: a conceptual and empirical review. International Journal of Mental Health 16:3-45, 1988Google Scholar



