Risk Behaviors for Sexually Transmitted Infections Among Men With Mental Disorders
Abstract
OBJECTIVE: Risk behaviors for sexually transmitted infections among men with mental disorders who were using outpatient psychiatric services and among men who had never been treated for a mental disorder were compared. METHODS: Ninety-two men with major mental disorders, including schizophrenia, bipolar disorder, and mood disorders, were individually matched for age and ethnicity with 92 men who had never been treated for mental illness. All subjects completed a semistructured interview about specific risk behaviors for sexually transmitted infections that they may have engaged in during the preceding year. RESULTS: The 49 patients with mental disorders who had been sexually active in the preceding year were significantly more likely than the 78 sexually active comparison subjects to have known their sexual partner for less than one day and to report having been pressured into unwanted sexual intercourse. A strong but not significant trend was found for sexually active patients to have had sex with a male partner and sex with a drug user. Overall, the patients with mental disorders answered ten questions measuring AIDS knowledge questions significantly less well than the comparison subjects. CONCLUSIONS: The results underscore the priority for developing programs for preventing risk behaviors for sexually transmitted infections among men with mental disorders.
A clinically important minority of patients with mental disorders engage in behaviors that put them at risk of contracting sexually transmitted infections. Their behaviors include having multiple sexual partners (1,2,3,4,5,6), having sexual intercourse with partners with whom they are unfamiliar (4,7,8,9), engaging in male homosexual anal intercourse (2,5,6), and failing to use condoms or using them inconsistently (1,2,3,4,5,6,8).
Some of the factors postulated to contribute to patients' vulnerability to engage in these risk behaviors include deficits in their knowledge about how such diseases, particularly AIDS, are transmitted and prevented (4,8,10,11) and a susceptibility to coercion into unwanted sexual activity (1,4). Other factors may include limited impulse control related to having a mental disorder, difficulties in establishing stable social and sexual relationships, and comorbid alcohol and drug abuse (7,12), as well as varying degrees of impaired autonomy during the course of illness (13,14).
The prevalence of HIV seropositivity among persons with mental illness underscores the likelihood that this population is at high risk. In outpatient settings, prevalence estimates vary between two and six percent of voluntarily tested patients in Wisconsin (1,4) and 19 percent of men in a large homeless shelter in New York City (15). In one study, a third of the patients had been treated for sexually transmitted infections other than AIDS (1).
However, with few exceptions (6), most of the studies have been done in North American settings. Furthermore, there is a dearth of controlled studies. Two studies of female psychiatric patients showed that they sustained greater risks for sexually transmitted infections, including AIDS, than persons in a control group (16,17). As far as we are aware, no controlled or comparison studies about risk behaviors of men with mental disorders have been reported, which limits our understanding of the priorities for developing preventive intervention programs for male patients. With this particular limitation in mind, we interviewed men with mental disorders who were using outpatient services to determine the prevalence of risk behaviors for sexually transmitted infections including AIDS as well as their knowledge about AIDS. We compared these findings with those from a matched group of men who had never been treated for a mental disorder.
Methods
The psychiatric patients attended a public community mental health center (CMHC) in Auckland, New Zealand, that served an inner-city population of approximately 90,000. The clinic predominantly treated patients with chronic disorders of schizophrenia, bipolar disorder, and other mood disorders. Between July 1993 and June 1995, CMHC staff were asked to refer all patients between the ages of 18 and 51 years for consideration for inclusion into the study. Patients with a primary diagnosis of substance abuse, including alcohol abuse, or mental retardation were excluded. Individual caseloads were regularly reviewed to ensure that eligible patients were identified.
Informed consent was obtained from patients after a full explanation of the study was provided in accordance with the requirements of the ethics committee, including stressing that patients could refuse to participate or could withdraw at any time without their care being affected in any way. Ninety-two of the 139 patients who were referred for consideration agreed to participate, for a participation rate of 66 percent. Thirty-eight patients refused to participate, and another nine were not approached because it was judged that they could not provide truly valid consent.
The sample included 64 Europeans, 25 Polynesians or Maoris, and three other patients of Indian, Turkish, and Filipino origin. Each patient was matched with another individual for ethnicity and age to within two years. The comparison group were men who reported that they had never seen a psychiatrist or a psychologist and had never been treated for a mental disorder. They were selected from the waiting rooms of publicly funded medical and surgical outpatient clinics. They included 51 patients from a dermatology clinic, 23 from a surgery clinic, nine from a urology clinic, eight from a dental clinic, and one from a neurology clinic. Publicly funded clinics were chosen to try to obtain comparison subjects from a similar socioeconomic group as the psychiatric patients.
The interview schedule was semistructured and was modified from existing schedules (9,10,18). It covered information on specific heterosexual and homosexual risk behaviors for sexually transmitted infections, a history of treatment for sexually transmitted infections, current physical symptoms, and a test of cognitive functioning (19). Knowledge questions required responses of yes, no, or don't know. Findings about patients' family planning outcomes have been reported elsewhere (20).
Two female research nurses, formerly senior psychiatric nurses, interviewed the psychiatric patients in private, and three female research nurses interviewed the comparison subjects. The nurses were employed part time for this purpose and had been given formal training on risk assessment and prevention of sexually transmitted infections.
The data were analyzed using SAS (21). Percentages for responses to each question were calculated; the denominator varied according to the number responding to each question. Chi square tests were used to compare differences between groups when cell sizes were sufficient; otherwise Fisher's exact test (two tailed) was used in the two-by-two analyses.
Results
Samples
The mean±SD age of the patients was 35.6±8.2 years, and that of the comparison subjects was 35.3±8.2 years. The mean±SD duration of mental disorder was 12.9±8.8 years. Additional psychiatric and medical information for the patient group is provided in Table 1. The most common psychiatric diagnoses, which were obtained by retrospective chart review and by consultation with the CMHC staff, were schizophrenia or schizoaffective disorders. Twelve patients (14 percent) were classified as having both an additional alcohol and drug abuse problem, five patients (6 percent) had an additional alcohol abuse problem only, and three (4 percent) had an additional drug abuse problem only.
The patients with mental disorders were compared with the comparison subjects on visits to a general practitioner or sexually transmitted infection clinic and on socioeconomic factors, including social welfare assistance, current employment, marital status, and education. Twenty-three patients with mental disorders (25 percent) had been to a sexually transmitted infection clinic at any time in the past, compared with 20 of the comparison subjects (22 percent), but the difference was not statistically significant. Sixty-one psychiatric patients (66 percent) and 78 comparison subjects (85 percent) had visited a general practitioner in the past year (χ2=6.70, df=1, p<.01).
Significantly more psychiatric patients than comparison subjects were receiving social welfare assistance (85 percent compared with 23 percent; χ2=70.3, df=1, p<.001), and fewer patients than comparison subjects were currently employed (29 percent compared with 75 percent; χ2=38.42, df=1, p<.001). Significantly fewer patients than comparison subjects were in a married or common-law relationship (13 percent compared with 66 percent; χ2=54.52, df=1, p<.001). The mean age at which patients completed schooling was 16.2 years, compared with 16.4 years for the comparison subjects. Only 14 patients had attended a technical college or university compared with 31 of the comparison subjects.
Within the previous year, 45 patients with mental disorders (49 percent) had heterosexual intercourse, and another four (4.3 percent) had homosexual contact. In contrast, 77 comparison subjects (84 percent) had engaged in heterosexual intercourse in the past year, and another subject had homosexual contact. The patients were significantly less likely than the comparison subjects to have been sexually active over the past year (χ2=21.38, df=1, p<.001).
As shown in Table 2, the 49 patients who were sexually active were significantly more likely than the 78 sexually active comparison subjects to have known their sexual partner for less than one day and to report having been pressured into unwanted sexual intercourse during the preceding year. A strong but not significant trend was found for patients with mental disorders to be more likely to have had sex with a male partner and to have had sex with a suspected or known intravenous drug user during the preceding year.
Furthermore, 11 patients, three of whom had shared needles, had injected themselves with drugs at some point in the past, including two patients within the past year. The three comparison subjects who had injected themselves with drugs had all done so more than a year ago. Three-quarters (76 percent) of the sexually active patients reported at least one of the risk factors listed in Table 2, compared with 49 percent of the comparison subjects (χ2=9.64, df=1, p=.001).
One homosexual psychiatric patient who said he was HIV positive had receptive anal intercourse during the past year, although he reported using condoms on every occasion of intercourse. Another homosexual patient reported having had sex with a male whom he knew had AIDS but denied engaging in anal intercourse. He also had not been tested for the AIDS virus. Two other patients, one of whom had 12 male partners in the past year, denied having anal intercourse.
Table 3 shows the percentages of patients with mental disorders and comparison subjects who gave correct responses to ten questions about AIDS. For seven of the ten questions, the patients with mental disorders scored significantly lower than the comparison subjects. The patients scored significantly fewer mean correct answers than the comparison subjects.
Patients with mental disorders and comparison subjects were asked whether they had ever had a sexually transmitted infection. Only one patient reported being HIV positive. Eighteen patients said that they had had gonorrhea, compared with eight comparison subjects (χ2=5, df=1, p=.025). Five patients reported having had syphilis, compared with none of the comparison subjects (p=.027, Fisher's exact test, two tailed). Eight persons in each group reported having had chlamydia. Five patients reported genital herpes, compared with 12 comparison subjects, but the difference was not significant. When asked about current symptoms, two patients reported discharge from the penis, pain passing water, and itching in the genital region, indications of current infection. None of the comparison subjects reported such symptoms.
Twenty-six of the 92 patients with mental disorders (28 percent) said that they had talked to a doctor or nurse about AIDS. Of the 35 patients who were sexually active within the past year and had a least one risk factor for a sexually transmitted infection, 13 (37 percent) had at some time talked to a doctor or nurse about AIDS.
Discussion and conclusions
These findings should be considered in the light of several possible limitations. First, social desirability may have biased some responses. Second, information on patients' diagnoses was limited to clinicians' reports and information from the medical records. Third, the interrater reliability of the interviewers was not established. Fourth, the participants were not matched for sexual orientation.
Fifth, although an attempt was made to select a comparison group of a socioeconomic status similar to that of the patients with mental disorders, patients were significantly more likely than the comparison subjects to receive social welfare assistance and less likely to be currently employed. They were also less likely to be married or in a common-law relationship. Therefore, differences between groups in risk behaviors may reflect the effects of differences in socioeconomic or marital status independent of the presence or absence of mental illness. Finally, the sample sizes were small, and the results are not necessarily generalizable to other settings or cultures.
Significantly fewer of the patients with mental disorders than comparison subjects had been sexually active in the year preceding the interview, which might have been predicted (3) and perhaps reflected an effect of neuroleptics on sexual desire (22). However, sexually active patients were significantly more likely to report at least one risk behavior for sexually transmitted infections during the past year, indicating the importance for psychiatrists or other mental health professionals of taking an appropriate sexual history. Identification of risk is a necessary prerequisite for providing preventive counseling and referral for testing for sexually transmitted infections. The importance of incorporating educational material in counseling is also indicated by the patients' relatively poor performance on tests of AIDS knowledge.
Sexually active patients were significantly more likely than sexually active comparison subjects to report two risk behaviors during the previous year—having known a sexual partner for less than one day and having been pressured into unwanted sexual intercourse. Nearly a third of the sexually active patients reported having engaged in sexual intercourse with a partner known for less than a day, which, consistent with earlier findings (7,9), perhaps reflects a susceptibility to coercion or difficulty in establishing or maintaining enduring sexual relationships or in postponing gratification.
Eleven percent of the sexually active patients reported being pressured into unwanted sexual intercourse during the preceding year. Physical and sexual assault of men with mental disorders is prevalent (23,24). Impairment in autonomy, including impaired cognitive and evaluative understanding and judgment, may contribute to patients' vulnerability to coercion into sexual risk behaviors (14,25). However, in contrast to earlier studies (1,2,3,4,5,6), patients were no more likely to have multiple sexual partners or trade sex for money or drugs than comparison subjects.
We also found a strong but not significant trend for sexually active psychiatric patients to have had sex with a male partner and to have had sex with a person known to be a drug user. However, the numbers were quite small, and only one man reported engaging in homosexual anal intercourse during the past year. The percentage of men with mental disorders engaging in homosexual behavior was little different from percentages reported in earlier studies (2,5,26). Only three patients reported sharing dirty needles when injecting themselves with intravenous drugs at some point in the past.
Our results support a priority for developing intervention programs for preventing sexually transmitted infections for men with mental disorders. Although few model programs exist for addressing risk, some evidence has been found that the sexual risk-taking behaviors of patients can be modified (12,27). However, evidence also suggests that mental health professionals, including psychiatrists, sometimes fail to identify patients at risk for sexually transmitted infections, including AIDS, and fail to appropriately counsel patients (6,28). Although further controlled or comparison studies of patients' risk behaviors are needed, the important challenge of developing effective prevention programs for sexually transmitted infections remains.
Acknowledgments
The authors thank Helen Roberts, M.D., for helpful suggestions; Alistair Stewart for statistical advice; and research nurses Norma Moerland, Christine Van Den Berg, Ruth Patton, Angela Cook, and Colleen Preston. The study was funded by the Auckland Medical Research Foundation.
When this work was done Dr. Coverdale was associate professor in the department of psychiatry and behavioral science of the Faculty of Medicine and Health Science at the University of Auckland in New Zealand, where Ms. Turbott is a research assistant. Dr. Coverdale is currently affiliated with the department of psychiatry and behavioral sciences at Baylor College of Medicine, 1 Baylor Plaza, Houston, Texas 77030.
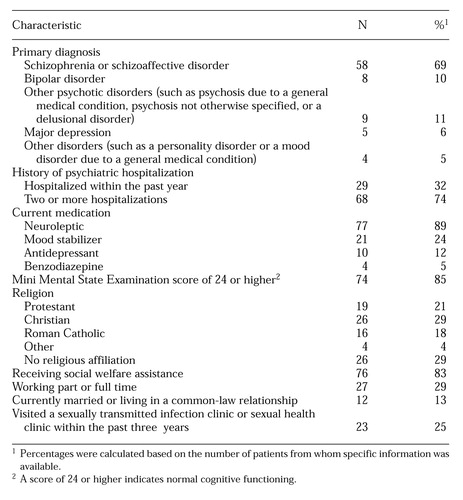 |
Table 1. Psychiatric and medical information for 92 men with mental disorders who were subsequently interviewed about their risk for sexually transmitted infections
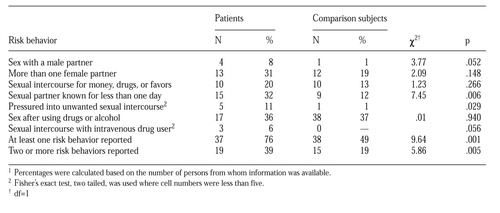 |
Table 2. Self-reported risk behaviors fo sexually transmitted infections of 49 sexually active male patients with male patients with mental disorders and 78 sexually active comparison subjects1
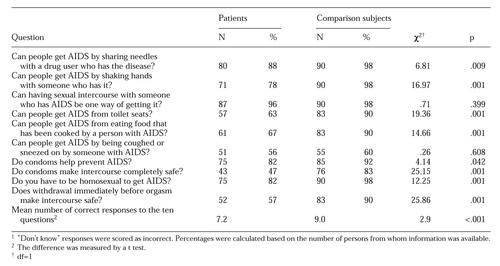 |
Table 3. Patients with mental disorders and comparison subjects who correctly answered questions about AIDS1
1. Kelly JA, Murphy DA, Bahr R, et al: AIDS/HIV risk behavior among the chronic mentally ill. American Journal of Psychiatry 149:886-889, 1991Google Scholar
2. Cournos F, McKinnon K, Meyer-Bahlberg H, et al: HIV risk activity among persons with severe mental illness: preliminary findings. Hospital and Community Psychiatry 44:1104-1106, 1993Abstract, Google Scholar
3. Cournos F, Guido JR, Coomaraswamy S, et al: Sexual activity and risk of HIV infection among patients with schizophrenia. American Journal of Psychiatry 151:228-232, 1994Link, Google Scholar
4. Kalichman SC, Kelly JA, Johnson JR, et al: Factors associated with risk for HIV infection among chronic mentally ill adults. American Journal of Psychiatry 151:221-227, 1994Link, Google Scholar
5. Kelly JA, Murphy DA, Sikkema KJ, et al: Predictors of high and low levels of HIV risk behavior among adults with chronic mental illness. Psychiatric Services 46:813-818, 1995Link, Google Scholar
6. Thompson SC, Checkley GE, Hocking JS: HIV risk behaviour and HIV testing of psychiatric patients in Melbourne. Australian and New Zealand Journal of Psychiatry 31:566-576, 1997Crossref, Medline, Google Scholar
7. Carmen E, Brady SM: AIDS risk and prevention for the chronic mentally ill. Hospital and Community Psychiatry 41:652-657, 1990Abstract, Google Scholar
8. Chuang HT, Atkinson M: AIDS knowledge and high-risk behavior in the chronic mentally ill. Canadian Journal of Psychiatry 41:269-272, 1996Crossref, Medline, Google Scholar
9. Volavka J, Convit A, O'Donnell J: Assessment of risk behaviors for HIV infection among psychiatric inpatients. Hospital and Community Psychiatry 43:482-485, 1992Abstract, Google Scholar
10. Aruffo J, Coverdale JH, Chacko RC, et al: Knowledge about AIDS among women psychiatric outpatients. Hospital and Community Psychiatry 41:326-328, 1990Abstract, Google Scholar
11. Steiner J, Lussier R, Rosenblatt W: Knowledge about and risk factors for AIDS in a day hospital population. Hospital and Community Psychiatry 43:734-735, 1992Abstract, Google Scholar
12. Kalichman SC, Sikkema KJ, Kelly JA, et al: Use of a brief behavioral skills intervention program to prevent HIV infection among chronic mentally ill adults. Psychiatric Services 46:275-277, 1995Link, Google Scholar
13. McCullough LB, Coverdale JH, Bayer T, et al: Ethically justified guidelines for family planning interventions to prevent pregnancy in female patients with chronic mental illness. American Journal of Obstetrics and Gynecology 167:19-25, 1992Crossref, Medline, Google Scholar
14. Coverdale JH: HIV risk behavior in the chronically mentally ill. International Review of Psychiatry 8:149-156, 1996Crossref, Google Scholar
15. Susser E, Valencia E, Conover S: Prevalence of HIV infection among psychiatric patients in a New York City men's shelter. American Journal of Public Health 83:568-570, 1993Crossref, Medline, Google Scholar
16. Miller LJ, Finnerty M: Sexuality, pregnancy, and childrearing among women with schizophrenia-spectrum disorders. Psychiatric Services 47:502-506, 1996Link, Google Scholar
17. Coverdale JH, Turbott SH, Roberts H: Family planning needs and STD risk behaviours of female psychiatric outpatients. British Journal of Psychiatry 171:69-72, 1997Crossref, Medline, Google Scholar
18. McKinnon K, Cournos F, Meyer-Bahlburg H, et al: Reliability of sexual risk behavior interviews with psychiatric patients. American Journal of Psychiatry 150:972-974, 1993Link, Google Scholar
19. Folstein MF, Folstein SE, McHugh PR: "Mini-Mental State": a practical guide for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research 12:189-198, 1975Crossref, Medline, Google Scholar
20. Coverdale JH, Turbott SH: Family planning outcomes of male chronically ill psychiatric outpatients. Psychiatric Services 48:1199-1200, 1997Link, Google Scholar
21. SAS/STAT User's Guide, Release 6.03 Edition. Cary, NC, SAS Institute, 1988Google Scholar
22. Sullivan G, Lukoff D: Sexual side effects of antipsychotic medication: evaluation and interventions. Hospital and Community Psychiatry 41:1238-1241, 1990Abstract, Google Scholar
23. Jacobson A, Richardson B: Assault experiences of 100 psychiatric inpatients: evidence of the need for routine inquiry. American Journal of Psychiatry 144:908-913, 1987Link, Google Scholar
24. Jacobson A: Physical and sexual assault histories among psychiatric outpatients. American Journal of Psychiatry 146:755-758, 1989Link, Google Scholar
25. Coverdale JH, Bayer T, McCullough LB, et al: Sexually transmitted disease prevention services for female chronically mentally ill patients. Community Mental Health Journal 31:303-315, 1995Crossref, Medline, Google Scholar
26. Lyketsos GC, Sakka P, Mailis A: The sexual adjustment of chronic schizophrenics: a preliminary study. British Journal of Psychiatry 143:376-382, 1983Crossref, Medline, Google Scholar
27. Kelly JA, McAuliffe TL, Sikkema KJ, et al: Reduction in risk behaviors among adults with severe mental illness who learned to advocate for HIV prevention. Psychiatric Services 48:1283-1288, 1997Link, Google Scholar
28. Coverdale JH, Falloon I, Turbott SH: Sexually transmitted disease and family planning counseling of psychiatric patients in New Zealand. Australian and New Zealand Journal of Psychiatry 31:285-290, 1997Crossref, Medline, Google Scholar