The Epidemiology of Common Late-Life Mental Disorders in the Community: Themes for the New Century
Abstract
OBJECTIVE: The prevalence and incidence of the major mental disorders of late life that are common in the community and in primary health care are reviewed. METHODS: Community-based studies in English that included older adults were identified through MEDLINE searches and were reviewed. RESULTS: As the population ages, dementia, depression, and other mental conditions of the aged will demand more attention from clinicians and investigators to minimize their effects on disability, the use of health care services, and the quality of life for older adults and caregivers. Up to 15 to 20 percent of older adults have significant depressive symptoms, and it is estimated that as many as 45 percent of persons age 85 years and older have significant cognitive impairment and dementia. Other mental-health-related conditions, such as anxiety disorders, alcohol abuse, and prescription medicine misuse, are also important considerations but have not been as well studied as depression and dementia. Because an increasing proportion of older adults are members of minority groups, clinicians need to increase their awareness of how cultural factors relate to risk for mental disorders in late life. CONCLUSIONS: Attention to three themes may help clinicians and investigators meet the challenge of treating the common mental disorders of later life: the effect of these disorders on functioning, prevention of the consequences of mental disorders, and integration of mental health care and primary health care services.
As the American population ages, dementia, depression, and other mental conditions of the aged will demand more attention to minimize their effects on disability, the use of health care services, and the quality of life for older adults and caregivers. Given the effects of depression, problems of cognitive functioning, and other mental disorders on everyday functioning, understanding the factors associated with preservation of mental health into late life assumes great importance as an issue for public health.
The purpose of this paper is to present estimates of the prevalence and incidence of common mental disorders of late life, focusing on community studies. However, were we to restrict our attention to a list of specific mental disorders, we might lose sight of important phenomena. For example, much disability may be associated with depressive symptoms that do not meet standard criteria for major depression. Similarly, impairment secondary to the misuse of prescription psychotropic medicines by older persons is an important issue that has not been well studied. Our aim, then, is to highlight critical themes in the epidemiology of common mental disorders in late life that are especially pertinent for health service planners and providers as we face the challenges of aging in the new century.
Epidemiological concepts
Prevalence refers to the proportion of the population that meets criteria for a disorder within a specified time. Because duration of illness may be affected by treatment and other factors that influence the course of disease after onset, prevalence rates may be affected by these factors as well.
In contrast, incidence is the rate at which a disorder arises among persons who were previously unaffected. Because incidence studies require that a cohort of individuals who are determined to be free of the disorder are reassessed after a follow-up interval to determine who has developed the disorder, they are generally more difficult to carry out. Thus incidence rates are harder to obtain than prevalence rates. Prevalence estimates are useful in assessing the need for health services, and estimates of incidence are helpful in assessing risk factors, with implications for prevention of disorders. For example, if depression is found to be more prevalent among women than among men, this finding does not mean that women are at increased risk for depression—the duration of depression could be longer among women than among men.
Interventions that diminish the duration of disease or that delay its onset will decrease prevalence rates, but so will rising mortality from the condition. In addition, selection of study samples from among individuals who present to specialized health services may be convenient, but such studies may yield biased estimates of risk because factors not associated with the onset of the disorder may influence presentation to the health services. Because older persons are less likely than younger persons to receive treatment from mental health specialists, the study of samples derived from the community, including primary health care settings, assumes particular importance for understanding mental disorders among older people.
We note that epidemiological studies differ in whether adults age 65 years and older are included in the study sample. Some studies focus on older adults but do not use standardized psychiatric interviews to obtain estimates of prevalence or incidence. Other studies employ standardized interviews but do not include older adults; an example is the National Comorbidity Survey, which did not include adults age 55 and older (1).
This review focuses on community studies identified through MEDLINE that were written in English, that included substantial numbers of persons age 65 years and older, and that employed standardized assessment procedures. Goldberg and Huxley (2) set forth a conceptual framework, including factors associated with vulnerability and resiliency, that emphasizes common mental disorders. We will not cover all the conditions mentioned in the fourth edition of the American Psychiatric Association's Diagnostic and Statistical Manual of Mental Disorder (DSM-IV), but we will focus attention on selected conditions and behaviors that are the most common and potentially preventable causes of disability among community-dwelling elderly persons. For example, we will not discuss schizophrenia, manic-depression, or psychosis, although we realize that they are important conditions in other contexts.
Mood disorders
Estimates of the prevalence of major depression in samples that include older adults range widely, depending on the definition and procedure used for counting a case of depression (3). Table 1 summarizes estimates from several studies using a variety of diagnostic criteria (4,5,6,7,8,9,10,11,12,13,14,15,16). With the exception of studies in Hobart, Tasmania (10), and Gothenberg, Sweden (15), investigations that have used DSM criteria for major depression have found prevalence rates of about 5 percent or less among older people. Estimates derived from use of standardized assessments that rely on DSM criteria suggest that the prevalence of depression declines with age. Using data from psychiatric interviews of adults in the Baltimore Epidemiologic Catchment Area (ECA) study, Romanoski and colleagues (17) showed that major depression declined, while other depression syndromes increased with advancing age.
In comparing studies, estimates are likely to differ because of differences in settings, sampling processes, and methods for ascertaining diagnoses. Estimates based on symptom scales, such as the Center for Epidemiological Studies Depression Scale, are consistent with the clinical impression that the prevalence of depression increases with advancing age. Estimated rates of significant depressive symptoms of about 15 percent among community samples of elderly persons have been reported (see Table 1). Estimated rates of depressive symptoms among physically ill older adults in primary care settings may be substantially higher.
Incidence studies that have been carried out using DSM criteria mirror the same pattern of decline with advancing age as reported from prevalence surveys (18,19). The 13-year follow-up of the participants of the Baltimore ECA sample revealed that the life course distribution of the incidence of DSM major depression appeared to be bimodal, with a primary peak in the fourth decade and a secondary peak in the sixth decade (19). The National Comorbidity Survey also showed an upward shift in onset of major depression among women age 50 to 54 years, the oldest age group studied (1). In Sweden, Hagnell and colleagues (20) reported that rates for new cases of depression were highest in the older age groups and that rates of depression had increased between 1947-1957 and 1957-1972. A study in Stirling County in Canada using 16-year follow-up data reported declining incidence rates of depression with age (21).
Prospective studies reveal an increased risk of major depression among women compared with men, consistent with findings based on prevalence surveys (18,20,22). Other risk factors for depression in late life, based on results of prospective studies, include widowhood (23,24,25,26), physical illness (25,27), educational attainment less than high school (22,28), impaired functional status (29), and heavy alcohol consumption (30). Prevalence estimates from the ECA program were consistent with lower prevalence of major depression among African Americans than among whites (31,32). Incidence of major depression over the course of a one-year follow-up was higher among whites compared with minorities, even adjusting for age, gender, level of educational attainment, employment, marital status, and neighborhood characteristics (22). Careful attention to measurement issues related to depression among older adults may clarify the extent to which reported differences in risk according to ethnicity reflect differences in diagnostic practices (33).
Much of the disability attributed to depression may be associated with depressive symptoms that do not meet criteria for major depression (34). Several studies that employed a measure of depression that did not meet the standard DSM criteria for major depression are listed in Table 1. Inspection of the estimates for minor depression reveals that a significant additional number of older adults would be identified as having a depressive disorder, consistent with studies finding that patients with minor depression tend to be older and more physically ill.
Age may be one crucial variable that influences presentation, expression, and recognition of depression, which may also reflect differences in etiology of depressive symptoms. Based on the 13-year follow-up of older adults in the Baltimore ECA sample, persons with depressive symptoms without sadness (hopelessness, worthlessness, thoughts of death, wanting to die, or suicide) were at increased risk for functional impairment, cognitive impairment, psychological distress, and death over the next 13-year interval (7). In another prospective cohort study that used performance measures of functioning, older adults with depressive symptoms were found to be at increased risk for functional decline over a four-year follow-up period (35).
Depressive symptoms in older persons are an important risk factor for development of cognitive impairment as well as functional decline (36,37). A common pathophysiologic process, such as vascular lesions, may be a final common pathway for development of depression and dementia. More studies of the phenomenology of depression and of the relationship between depression and anxiety, cognitive functioning, and physical illness would help clarify how depression presents among older adults.
Suicidal behavior
Suicide rates increase with advancing age and appear to be rising among recent cohorts of older persons. Because national statistics generally do not include subtle forms of suicide, such as cases of nursing home residents who stop eating, estimated rates are probably conservative.
Depression is the psychiatric condition most often linked to suicide among older adults. In a study that used psychological autopsy to investigate all suicides within a geographical region, Conwell and coworkers (38) found that with increasing age, depression was more likely to be unaccompanied by other psychiatric conditions such as substance abuse. Although thoughts of death may be developmentally expected in older adults, suicidal thoughts are not. Based on data from a stratified sample of older primary care patients, Callahan and colleagues (39) estimated the prevalence of suicidal ideation to be between .7 and 1.2 percent. Unfortunately, no demographic or clinical variables distinguished depressed suicidal patients from depressed nonsuicidal patients.
Skoog and associates (40) interviewed 494 adults age 85 years and older living in Gothenberg, Sweden, and found a one-month prevalence of any suicidal thoughts of 9.6 percent among men and 18.7 percent among women. In the Gothenberg study, suicidal ideation was strongly associated with depression. Only 6.2 percent of the participants who did not meet criteria for depression or anxiety endorsed any suicidal thoughts, while almost half of the persons who met criteria for depression did.
Older adults use more lethal methods in attempting suicide than do younger persons. Older men, especially older white men, appear to have the highest rates of completed suicide. Because suicide among older adults appears to be strongly related to depressive symptoms, efforts to address increasing suicide rates will require innovation to deliver effective treatment for depression to older adults. Several studies that are testing interventions based in primary care settings are under way.
Anxiety and mixed anxiety-depression
In his 1965 book, The Clinical Psychiatry of Late Life, Post (41) observed that depression in older people was likely to remain unrecognized when presenting as "an exacerbation of anxious, hypochondriacal, phobic, or obsessional propensities." Symptoms of anxiety occurring alone or with depression are important but understudied phenomena. Phobic anxiety disorders were among the most common mental disturbances in late life in the ECA study (32). Community-based prevalence estimates have suggested that about 5 percent of adults age 65 years and older meet criteria for an anxiety disorder (42,43).
However, worry or nervous tension, rather than specific anxiety syndromes such as panic disorder, may be more important for older people. Prevalence studies of panic disorder and obsessive-compulsive disorder in older samples revealed low rates of less than .5 percent (6,12,42,43,44). The prevalence of generalized anxiety disorder among older adults is higher, ranging from 1.1 percent (44) to 17.3 percent (15). Anxiety symptoms that do not meet criteria for specific syndromes are reported for up to 17 percent of elderly men and 21 percent of elderly women (45).
Incidence studies paint a different picture, with findings of a very low rate of development of new cases of DSM-IV anxiety disorders among older persons in the community. For example, in a study in Lundby, Sweden, the estimated incidence of any anxiety disorder (panic disorder with and without agoraphobia, general anxiety disorder, and anxiety disorder not otherwise specified) was 0 in persons age 65 years and older (46). In the 13-year follow-up of the Baltimore ECA study, no new cases of panic disorder, with or without agoraphobia, occurred among persons who began the follow-up interval age 65 years and older (47). Incidence rates for obsessive-compulsive disorder, estimated from the one-year follow-up of the five ECA sites, declined with age among men, but a slight upturn in incidence was noted among older women (18). In the 13-year follow-up of the Baltimore ECA study, the incidence rate for obsessive-compulsive disorder among women age 65 years and older was .94 per 1,000 person-years of follow-up and was 0 among the older men, again revealing a pattern of increasing incidence with age for women (48).
Low rates of anxiety disorders among older people should not be interpreted to mean that anxiety disorders and symptoms are not significant in this age group. Anxiety disorders, especially their co-occurrence with depressive symptoms, have clinically relevant implications. For example, physicians may focus on anxiety symptoms and may fail to consider depression with the result that patients with both anxiety and depressive symptoms are more likely to receive a benzodiazepine than to receive treatment for depression (49,50). A recent National Institute of Mental Health workshop on anxiety in late life called for additional work on understanding this critical area of comorbidity and the influence of age on the presentation and course of anxiety.
Alzheimer's disease and other dementia syndromes
Alzheimer's disease and other dementia syndromes are among the most devastating of all illnesses. Although early dementia may be difficult to distinguish from normal aging, diagnostic criteria have undergone considerable refinement in the past decade. Prevalence rates of Alzheimer's disease vary widely. Studies by Pfeffer and colleagues (51), Evans and associates (52), and Skoog and others (53) have estimated that approximately half of older adults age 85 years and older are demented; other studies have produced estimates of less than 10 percent (27).
Although the risk of Alzheimer's disease may plateau at the oldest ages, advancing age has been the characteristic most clearly related to this disorder. Based on an analysis of more than 45 prevalence studies carried out between 1945 and 1985, Jorm and colleagues (54) developed the following rule of thumb: the prevalence of dementia doubles with every five years of age, reaching 11 percent at age 80 to 84 years, 21 percent at age 85 to 89 years, and 39 percent at age 90 to 94 years. Incidence studies have revealed a similar age-related pattern of increased incidence (55,56,57,58).
The prevalence of Alzheimer's disease may be higher among women, but this difference may reflect the longer survival of women compared with men. Studies of the incidence of Alzheimer's disease do not show marked differences in incidence rates between women and men (59). Estimates of the prevalence of dementia and Alzheimer's disease among U.S. minority groups reveal substantial disease burden on the African-American and Hispanic communities, with rates of Alzheimer's disease several times higher than among whites (60,61). There is a pressing need for more studies of Alzheimer's disease and other mental disorders of late life among the growing populations of older persons among African Americans, Hispanics, and other minority groups in the U.S.
In addition to advancing age, several other personal characteristics have been explored as risk factors for onset of Alzheimer's disease and other dementias, including family history of dementia, Parkinson's disease, or Down's syndrome; head trauma; hypothyroidism; and depression. Recent years have seen the realization that the apolipoprotein E (APOE) genotype may be one of the most influential characteristics associated with risk of Alzheimer's disease. Several studies have now established the relationship between APOE and both sporadic and familial forms of Alzheimer's disease (62) and possibly vascular dementia as well (63,64,65,66,67). However, the association between APOE and Alzheimer's disease may be attenuated among African Americans (61,68,69) and Nigerians (70).
Vascular factors have long been thought to influence mental health in late life. The realization that most dementia appeared to be related to neuropathologic changes described by Alzheimer in 1906 largely discredited the notion of "atherosclerotic dementia." However, recent evidence has rekindled interest in the role of vascular factors in dementia (71), including Alzheimer's disease (72,73,74). Vascular dementia—that is, dementia thought to be the result of strokes or cerebrovascular disease—may be more common than previously appreciated (75).
Environmental influences on the development of Alzheimer's disease must be important because some subjects with the high-risk APOE genotype do not develop dementia, twins have remained discordant for Alzheimer's disease for many years, and APOE may wane in importance as a risk factor among the very old (76). The significance of genotype should not deter a search for the environmental influences that may interact with genotype in determining the onset of Alzheimer's disease. Estrogen, nonsteroidal anti-inflammatory drugs, and other substances may be protective, and a number of trials are under way or planned to determine whether any of these substances will delay the onset of Alzheimer's disease. Despite gains in understanding the role of genotype in development of this disorder, there is still a compelling need to understand the potentially modifiable environmental and personal factors related to the development of cognitive impairment.
Use of alcohol
Alcohol consumption is common among older adults. Ten to 20 percent report daily use of alcohol (77). In a survey of residents of a retirement community, almost half reported some alcohol consumption, and 15 percent reported consumption of one to six drinks each week (78). Among 5,065 adults age 60 years and older screened in primary care practices in Wisconsin, 10.5 percent of the men and 3.9 percent of the women reported problem alcohol use (79).
However, the proportion of older persons who meet criteria for alcohol abuse or dependence appears to be much smaller. In the ECA study, for example, the one-month prevalence of alcohol abuse or dependence was 1.93 percent for men and .4 percent for women age 65 years and older (32). Grant and colleagues (80) reported similar figures from the National Health Interview Survey—2.77 percent for men and .37 percent for women age 65 years and older. Incidence rates for alcohol abuse or dependence appear to show an upturn with age, but only among men (18).
Alcohol consumption has been associated with cognitive impairment. In one study, patients age 40 to 50 years who reported use of alcohol for five years or more were more impaired on several measures of cognitive functioning, but this study was cross-sectional in design (81). Men with a history of heavy drinking, in contrast to men without such a history, recalled fewer words at a follow-up interview three years later, but appeared to lack insight into any impairment (82). Deficits associated with alcohol consumption were found to generalize to multiple domains such as verbal and nonverbal ability, memory, and perceptual motor skill (83). Chronic alcohol exposure was associated with memory loss even among older alcoholics who do not have Korsakoff's syndrome (84).
In a meta-analysis of case-control studies, findings on the relationship of alcohol consumption and dementia were essentially negative (85). However, if case-control studies fail to show alcohol consumption as an environmental risk factor for Alzheimer's disease, it may be because the population under study is heterogeneous in genetic susceptibility. Nonetheless, it is premature to rule out any risk factor or to draw causal inferences from cross-sectional studies.
In longitudinal studies, Hebert and associates (86) found no excess risk of alcohol use for new cases of Alzheimer's disease in East Boston. However, Saunders and colleagues (30) did find a relationship in a Liverpool sample. They reported that men with a history of heavy drinking were five times as likely to be rated as demented and four times as likely to be diagnosed as depressed. Although the study included a three-year follow-up, the results were based on retrospective review of alcohol consumption earlier in life. Similarly, although a history of depression was not found in early life among the alcohol users, this finding could reflect failure to recall episodes of depression. The relationship between chronicity, duration, frequency, timing, and quantity of alcohol consumption early in life and cognitive impairment in late life is not clear and remains an area for future investigation.
Misuse of prescription medicines
The misuse of prescription medicines and its effect on the mental status of older adults is a poorly studied but possibly important source of preventable delirium and depression. Misuse of prescription medications by older persons may also be linked to clinicians' difficulties in diagnosing depression and other disorders in this population.
Community surveys have revealed that the prevalence and duration of the use of psychoactive medicines increases with advancing age and with the number of reported health problems despite the potential for adverse reactions and polypharmacy among the elderly. Data from the National Survey of Psychotherapeutic Medicine Use suggested that long-term users of medicines tended to be older (71 percent were age 50 years and older) and were more likely to report use of general medical services (87). Another survey found that 25 percent of community-dwelling older adults took psychotherapeutic medicines regularly (88). Older adults were more likely than younger adults to have attempted suicide using prescription medicines, especially benzodiazepines and analgesics (89).
Although older adults are frequent consumers of psychoactive medicines, to what extent can this use be characterized as inappropriate? The concepts of prescription medicine "misuse" and "nonmedical use" are central to understanding possible effects on adults in later life. Nonmedical use is a form of misuse that is defined by the World Health Organization as "use of a prescription drug, whether obtained by prescription or otherwise, other than in the manner or for the time period prescribed, or by a person for whom the drug was not prescribed" (90).
Several indicators of misuse that have been gleaned from the literature are summarized in the accompanying box. By these criteria, significant proportions of community-dwelling older adults appear to misuse psychoactive medicines. A survey of 559 older adults in New Zealand estimated that 7 percent of the sample were taking two or more psychoactive medicines (91). Kail (92) found that in most studies, women outnumbered men in the use of psychoactive medicines by about two to one, but the extent to which this ratio reflects the greater prevalence and incidence of psychiatric disorders, especially depression, among women is unclear. Studies of the use of psychoactive medicines from the ECA study have found that use is associated with female gender (93,94), use of health services (93), use of illicit substances (95), functional impairment (94), and increased age (93,96).
Community surveys typically have limitations in measurement of psychiatric disorders, in ability to relate medicine use to symptoms, in accounting for characteristics that may influence the use of medicines, and in consideration of the consequences of medicine use. In addition to psychoactive medicines such as benzodiazepines, medications prescribed for medical conditions may result in mental status changes to which concomitant alcohol use may contribute. The complex interplay of mental disorders, medical conditions, and the use of powerful psychoactive substances by older persons presents a significant challenge for the health care services.
Indicators of possible misuse of prescription medicines
Use of a medicine prescribed for another person
Use for which the medicine was not intended
Simultaneous use of alcohol
Use of drugs from the same classification or with similar pharmacologic effects
Use in the context of potential adverse interactions with drugs or nutrients
Use when the indication is no longer present
Premature discontinuation
Inappropriate dose
Feeling of dependence
Use resulting in adverse consequences attributable to the medicine
Looking toward the 21st century
To meet the challenge of treating mental disorders in the aging population, we consider three themes for the future: a focus on function, prevention of the consequences of mental disorders, and integration of mental health care and primary health care services.
An important backdrop for these themes is the increasing proportion of older adults who are members of minority groups. Early on in the new century, older African Americans and Hispanic Americans will outnumber older whites in the United States. This demographic shift will have widespread implications for assessment and treatment of mental disorders among the aged. We need to improve our understanding of how cultural factors relate to risk factors, presentation to primary care physicians, and acceptability of treatment for older persons with mental disorders.
The first theme—a focus on function—requires that the full spectrum of depressive symptoms and comorbidity be examined in relation to function and quality of life. In other words, the field must move from a preoccupation with counting "cases" to more fundamental questions of how a "case" is to be defined. Future investigations will have to examine a range of symptoms and dimensional approaches to understand risk and how disorders might be prevented.
This rigor is not merely an academic exercise. An older patient may seek care for mental distress, often with accompanying physical illness and typically in the primary care setting, but may not meet standard criteria for a psychiatric disorder. How then is a psychiatric disorder to be defined in primary care? Development of new types of classification of mental disorders and new approaches to treatment may be necessary (97). The focus should be on enhancing functioning and quality of life and on how appropriate mental health care can be made available to previously underserved persons.
A second theme concerns ways to promote well-being and prevent the adverse consequences of the mental disorders of late life. Studies in which pharmacotherapy is used to slow the progression of Alzheimer's disease are already under way. A multisite investigation is examining the effects of training in memory, reasoning, and other abilities on prevention of functional decline in older adults at risk. Control of cardiovascular risk factors may diminish the impact of vascular dementia. Conditions that exacerbate cognitive impairment, such as the immoderate use of alcohol or the prescription of offending medicines, may be preventable. Understanding and addressing the psychological aspects of physical illnesses might result in prevention of disability from depression and may make the difference between dependence and independence.
A third theme is the organization of health care services to meet these challenges. Despite suggestions that persons with mental disorders in the U.S. bypass the general medical sector and seek care directly from a specialist in mental health care, data from the ECA studies indicate that persons with incident mental disorders tend to first seek care from a general physician (98). Elderly persons with mental disorders may be especially unlikely to bypass the general medical sector.
The ECA data suggest that compared with persons age 45 to 64, adults age 65 years and older were .39 times as likely (95 percent CI=.23 to .64) to have reported a visit with a professional in the mental health sector and .24 times as likely (CI=.06 to .91) to report a visit in the mental health sector that bypassed the general medical sector altogether (98). The general medical sector may be even more important as a venue for mental health care for African Americans than for whites (99). Rabins (100) reformulated estimates derived from prevalence studies of the Baltimore ECA study and concluded that unmet need for mental health services increases with age, with up to 63 percent of adults age 65 years and older having an unmet need for mental health care.
A major challenge in the next century will be to create a health care system that integrates primary health care and mental health care for older persons. Powerful disincentives mitigate against providing mental health services within primary care, not the least of which is the managed care environment that may discourage cooperation between sectors. To increase the effectiveness of treatment for older adults with mental disorders, mental health clinicians may need to make additional efforts to maintain rapport with staff in the primary care practices that serve these patients. Creating a bridge of mutual understanding across specialties, with advocacy for integration of mental health into a general medical framework, will be a key element in enhancing the overall health and functioning of older persons in the next century.
Acknowledgment
Dr. Gallo's work was supported by the Brookdale Foundation National Fellowship in Geriatrics.
Dr. Gallo is affiliated with the department of family practice and community medicine and the department of psychiatry in the School of Medicine of the University of Pennsylvania, 3400 Spruce Street, 2 Gates, Philadelphia, Pennsylvania 19104 (e-mail, [email protected]). At the time this work was done, he was affiliated with the department of mental hygiene in the School of Hygiene and Public Health at Johns Hopkins University in Baltimore. Dr. Lebowitz is with the adult and geriatric treatment and preventive interventions research branch of the National Institute of Mental Health in Rockville, Maryland. This paper is part of a special section on meeting the mental health needs of the growing population of elderly persons.
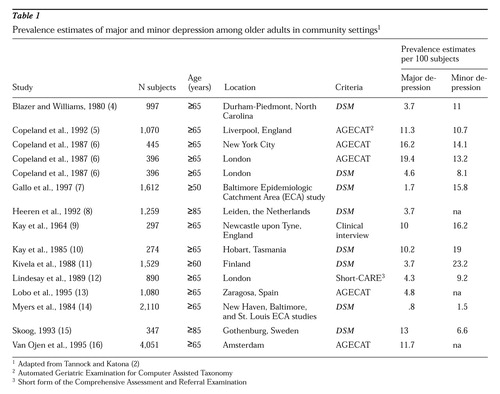 |
Table 1.
Prevalence estimates of major and minor depression among older adults in community settings1
1. Kessler RC, McGonagle KA, Swartz M, et al: Sex and depression in the National Comorbidity Survey: I. lifetime prevalence, chronicity, and recurrence. Journal of Affective Disorders 29:85-96, 1993Crossref, Medline, Google Scholar
2. Goldberg D, Huxley P: Common Mental Disorders: A Bio-Social Model. New York, Tavistock/Routledge, 1992Google Scholar
3. Tannock C, Katona C: Minor depression in the aged: concepts, prevalence, and optimal management. Drugs and Aging 6:278-292, 1995Crossref, Medline, Google Scholar
4. Blazer D, Williams CD: Epidemiology of dysphoria and depression in an elderly population. American Journal of Psychiatry 137:439-444, 1980Link, Google Scholar
5. Copeland JRM, Davidson IA, Dewey ME, et al: Alzheimer's disease, other dementias, depression, and pseudodementia prevalence, incidence, and three-year outcome in Liverpool. British Journal of Psychiatry 161:230-239, 1992Crossref, Medline, Google Scholar
6. Copeland JRM, Gurland BJ, Dewey ME, et al: Is there more depression and neurosis in New York? A comparative community study of the elderly in New York and London using the computer diagnosis AGECAT. British Journal of Psychiatry 151:466-473, 1987Crossref, Medline, Google Scholar
7. Gallo JJ, Rabins PV, Lyketsos CG, et al: Depression without sadness: functional outcomes of nondysphoric depression in later life. Journal of the American Geriatrics Society 45:570-578, 1997Crossref, Medline, Google Scholar
8. Heeren TJ, van Hemert AM, Lagaay AM, et al: The general population prevalence of nonorganic psychiatric disorders in subjects aged 85 years and over. Psychological Medicine 22:733-738, 1992Crossref, Medline, Google Scholar
9. Kay DWK, Beamish R, Roth M: Old age mental disorders in Newcastle-upon-Tyne: I. a study of prevalence. British Journal of Psychiatry 110:146-158, 1964Crossref, Medline, Google Scholar
10. Kay DWK, Henderson AS, Scott R, et al: Dementia and depression among the elderly living in the Hobart community: the effect of the diagnostic criteria on the prevalence rates. Psychological Medicine 15:771-788, 1985Crossref, Medline, Google Scholar
11. Kivela SL, Pahkala K, Eronen P: Depressive symptoms and signs that differentiate major and atypical depression from dysthymic disorder in elderly Finns. International Journal of Geriatric Psychiatry 4:79-85, 1988Crossref, Google Scholar
12. Lindesay J, Briggs SK, Murphy E: The Guys/Age Concern Survey: prevalence rates of cognitive impairment, depression, and anxiety on an urban elderly community. British Journal of Psychiatry 155:317-329, 1989Crossref, Medline, Google Scholar
13. Lobo A, Saz P, Marcos G, et al: The prevalence of dementia and depression in the elderly community in a Southern European population. Archives of General Psychiatry 52:497-506, 1995Crossref, Medline, Google Scholar
14. Myers JK, Weissman MM, Tischler GL, et al: Six-month prevalence of psychiatric disorders in three communities. Archives of General Psychiatry 41:959-967, 1984Crossref, Medline, Google Scholar
15. Skoog I: The prevalence of psychotic, depressive, and anxiety syndromes in demented and non-demented 85-year-olds. International Journal of Geriatric Psychiatry 8:247-253, 1993Crossref, Google Scholar
16. Van Ojen R, Hooijer C, Bezemer D, et al: Late-life depressive disorder in the community: I. the relationship between MMSE score and depression in subjects with and without psychiatric history. British Journal of Psychiatry 166:311-315, 1995Crossref, Medline, Google Scholar
17. Romanoski AJ, Folstein MF, Nestadt G, et al: The epidemiology of psychiatrist-ascertained depression and DSM-III depressive disorders: results from the Eastern Baltimore Mental Health Survey Clinical Reappraisal. Psychological Medicine 22:629-655, 1992Crossref, Medline, Google Scholar
18. Eaton WW, Kramer M, Anthony JC, et al: The incidence of specific DIS/DSM-III mental disorders: data from the NIMH Epidemiologic Catchment Area program. Acta Psychiatrica Scandinavica 79:163-178, 1989Crossref, Medline, Google Scholar
19. Eaton WW, Anthony JC, Gallo JJ, et al: Natural history of Diagnostic Interview Schedule/DSM-IV major depression: the Baltimore Epidemiologic Catchment Area follow-up. Archives of General Psychiatry 54:993-999, 1997Crossref, Medline, Google Scholar
20. Hagnell O, Lanke J, Rorsman B, et al: Are we entering an age of melancholy? Depressive illnesses in a prospective epidemiological study over 25 years: the Lundby study, Sweden. Psychological Medicine 12:279-289, 1982Crossref, Medline, Google Scholar
21. Murphy JM, Olivier DC, Monson RR, et al: Incidence of depression and anxiety: the Stirling County study. American Journal of Public Health 78:534-540, 1988Crossref, Medline, Google Scholar
22. Gallo JJ, Royall DR, Anthony JC: Risk factors for the onset of major depression in middle age and late life. Social Psychiatry and Psychiatric Epidemiology 28:101-108, 1993Crossref, Medline, Google Scholar
23. Bruce ML, Kim K, Leaf PJ, et al: Depressive episodes and dysphoria resulting from conjugal bereavement in a prospective community sample. American Journal of Psychiatry 147:608-611, 1990Link, Google Scholar
24. Zisook S, Shuchter SR: Depression through the first year after the death of a spouse. American Journal of Psychiatry 148:1346-1352, 1991Link, Google Scholar
25. Harlow SD, Goldberg EL, Comstock GW: A longitudinal study of risk factors for depressive symptomatology in elderly widowed and married women. American Journal of Epidemiology 134:526-538, 1991Crossref, Medline, Google Scholar
26. Mendes de Leon CF, Kasl SV, Jacobs S: A prospective study of widowhood and changes in symptoms of depression in a community sample of the elderly. Psychological Medicine 24:613-624, 1994Crossref, Medline, Google Scholar
27. Bachman DL, Wolf PA, Linn R: Prevalence of dementia and probable senile dementia of the Alzheimer type in the Framingham study. Neurology 42:115-119, 1992Crossref, Medline, Google Scholar
28. Wallace J, O'Hara MW: Increases in depressive symptomatology in the rural elderly: results from a cross-sectional and longitudinal study. Journal of Abnormal Psychology 101:398-404, 1992Crossref, Medline, Google Scholar
29. Bruce ML, Hoff RA: Social and physical health risk factors for first-onset major depressive disorder in a community sample. Social Psychiatry and Psychiatric Epidemiology 29:165-171, 1994Medline, Google Scholar
30. Saunders PA, Copeland JRM, Dewey ME, et al: Heavy drinking as a risk factor for depression and dementia in elderly men: findings from the Liverpool Longitudinal Community Study. British Journal of Psychiatry 159:213-216, 1991Crossref, Medline, Google Scholar
31. Somervell PD, Leaf PJ, Weissman MM, et al: The prevalence of major depression in black and white adults in five United States communities. American Journal of Epidemiology 130:725-735, 1989Crossref, Medline, Google Scholar
32. Robins LN, Regier DA: Psychiatric Disorders in America: The Epidemiologic Catchment Area Study. New York, Free Press, 1991Google Scholar
33. Gallo JJ, Cooper-Patrick L, Lesikar S: Depressive symptoms of whites and African Americans aged 60 years and older. Journal of Gerontology (Series B, Psychological Sciences and Social Sciences) 53:277-286, 1998Google Scholar
34. Horwath E, Johnson J, Klerman GL, et al: Depressive symptoms as relative and attributable risk factors for first-onset major depression. Archives of General Psychiatry 49:817-823, 1992Crossref, Medline, Google Scholar
35. Pennix WJH, Guralnik JM, Ferrucci L, et al: Depressive symptoms and physical decline in community-dwelling older persons. JAMA 279:1720-1726, 1998Crossref, Medline, Google Scholar
36. Devanand DP, Sano M, Tang MX, et al: Depressed mood and the incidence of Alzheimer's disease in the elderly living in the community. Archives of General Psychiatry 53:175-182, 1996Crossref, Medline, Google Scholar
37. Bassuk SS, Berkman LF, Wypij D: Depressive symptomatology and incident cognitive decline in an elderly community sample. Archives of General Psychiatry 55:1073-1081, 1998Crossref, Medline, Google Scholar
38. Conwell Y, Duberstein PR, Cox C, et al: Relationships of age and axis I diagnoses in victims of completed suicide: a psychological autopsy study. American Journal of Psychiatry 153:1001-1008, 1996Link, Google Scholar
39. Callahan CM, Hendrie HC, Nienaber NA, et al: Suicidal ideation among older primary care patients. Journal of the American Geriatrics Society 44:1205-1209, 1996Crossref, Medline, Google Scholar
40. Skoog I, Aevarsson O, Beskow J: Suicidal feelings in a population sample of 85-year-olds. American Journal of Psychiatry 153:1015-1020, 1996Link, Google Scholar
41. Post F: The Clinical Psychiatry of Late Life. New York, Pergamon, 1965Google Scholar
42. Regier DA, Boyd JH, Rae DS, et al: One-month prevalence of mental disorders in the U.S. based on the five Epidemiologic Catchment Area sites. Archives of General Psychiatry 45:977-986, 1988Crossref, Medline, Google Scholar
43. Bland RC, Newman SC, Orn H: Prevalence of psychiatric disorders in the elderly in Edmonton. Acta Psychiatrica Scandinavica Suppl 338:57-63, 1988Crossref, Medline, Google Scholar
44. Copeland JRM, Dewey ME, Wood N, et al: Range of mental illness among the elderly in the community: prevalence in Liverpool using the GMS-AGECAT package. British Journal of Psychiatry 150:815-823, 1987Crossref, Medline, Google Scholar
45. Himmelfarb S, Murrell SA: The prevalence and correlates of anxiety symptoms in older adults. Journal of Psychology 116:159-167, 1984Crossref, Medline, Google Scholar
46. Grasbeck A, Hagnell O, Otterbeck L, et al: Anxiety in the Lundby study: re-evaluation according to DSM-III-R, incidence, and risk. Neuropsychobiology 27:1-8, 1993Crossref, Medline, Google Scholar
47. Eaton WW, Anthony JC, Romanoski A, et al: Onset and recovery from panic disorder in the Baltimore ECA follow-up. British Journal of Psychiatry 173:501-507, 1998Crossref, Medline, Google Scholar
48. Nestadt G, Bienvenu OJ, Cai G, et al: Incidence of obsessive-compulsive disorder in adults. Journal of Nervous and Mental Disease 186:401-406, 1998Crossref, Medline, Google Scholar
49. Tollefson GD, Souetre E, Thomander L, et al: Comorbid anxious signs and symptoms in major depression: impact on functional work capacity and comparative treatment outcomes. International Clinical Psychopharmacology 8:281-293, 1993Crossref, Medline, Google Scholar
50. Lindesay J: Phobic disorders in the elderly. British Journal of Psychiatry 159:531-541, 1991Crossref, Medline, Google Scholar
51. Pfeffer RI, Afifi AA, Chance JM: Prevalence of Alzheimer's disease in a retirement community. American Journal of Epidemiology 125:420-436, 1987Crossref, Medline, Google Scholar
52. Evans DA, Funkenstein HH, Albert MS, et al: Prevalence of Alzheimer's disease in a community population of older persons: higher than previously reported. JAMA 262:2551-2556, 1989Crossref, Medline, Google Scholar
53. Skoog I, Nilsson L, Palmertz B, et al: A population-based study of dementia in 85-year-olds. New England Journal of Medicine 328:153-158, 1993Crossref, Medline, Google Scholar
54. Jorm AF, Korten AE, Henderson AS: The prevalence of dementia: a quantitative integration of the literature. Acta Psychiatrica Scandinavica 76:465-479, 1987Crossref, Medline, Google Scholar
55. Aevarsson O, Skoog I: A population-based study on the incidence of dementia disorders between 85 and 88 years of age. Journal of the American Geriatrics Society 44:1455-1460, 1996Crossref, Medline, Google Scholar
56. Hebert LE, Scherr PA, Beckett, LA, et al: Age specific incidence of Alzheimer's disease. JAMA 273:1354-1359, 1995Crossref, Medline, Google Scholar
57. Johansson B, Zarit SH: Prevalence and incidence of dementia in the oldest-old: a longitudinal study of a population-based sample of 84-90 year-olds in Sweden. International Journal of Geriatric Psychiatry 10:359-366, 1995Crossref, Google Scholar
58. Paykel ES, Brayne C, Huppert FA, et al: Incidence of dementia in a population older than 75 years in the United Kingdom. Archives of General Psychiatry 51:325-332, 1994Crossref, Medline, Google Scholar
59. Lebowitz BD, Pearson JL, Cohen GD: Older Americans and their illnesses, in Clinical Geriatric Psychopharmacology. Edited by Salzman C. Baltimore, Williams & Wilkins, 1998Google Scholar
60. Hendrie HC, Osuntokun BO, Hall KS, et al: Prevalence of Alzheimer's disease and dementia in two communities: Nigerian Africans and African Americans. American Journal of Psychiatry 152:1485-1492, 1995Link, Google Scholar
61. Teng MX, Stern Y, Marder K, et al: The APOE-epsilon-4 allele and the risk of Alzheimer's disease among African Americans, whites, and Hispanics. JAMA 279:751-755, 1998Crossref, Medline, Google Scholar
62. Farrer LA, Cupples LA, Haines JL, et al: Effects of age, sex, and ethnicity on the association between apolipoprotein E genotype and Alzheimer's disease: a meta-analysis. JAMA 278:1349-1356, 1997Crossref, Medline, Google Scholar
63. Wieringa GE, Burlinson S, Rafferty JA, et al: Apolipoprotein E genotypes and serum lipid levels in Alzheimer's disease and multi-infarct dementia. International Journal of Geriatric Psychiatry 12:359-362, 1997Crossref, Medline, Google Scholar
64. Frisoni GB, Bianchetti A, Govoni S, et al: Association of apolipoprotein E E4 with vascular dementia. JAMA 271:1317, 1994Crossref, Medline, Google Scholar
65. Kawamata J, Tanaka S, Shimohama S, et al: Apolipoprotein E polymorphism in Japanese patients with Alzheimer's disease or vascular dementia. Journal of Neurology, Neurosurgery and Psychiatry 57:1414-1416, 1994Crossref, Medline, Google Scholar
66. Roses AD, Saunder AM, Alberts MA, et al: Apolipoprotein E E4 alleles and risk of dementia. JAMA 273:374-375, 1995Crossref, Medline, Google Scholar
67. Katzman R, Zhang MY, Chen PJ, et al: Effects of apolipoprotein E on dementia and aging in the Shanghai Survey of Dementia. Neurology 49:779-785, 1997Crossref, Medline, Google Scholar
68. Maestre G, Ottman R, Stern Y, et al: Apolipoprotein E and Alzheimer's disease: ethnic variation in genotype risks. Annals of Neurology 37:254-259, 1995Crossref, Medline, Google Scholar
69. Mayeux R, Stern Y, Ottman R, et al: The apolipoprotein epsilon 4 allele in patients with Alzheimer's disease. Annals of Neurology 34:752-754, 1993Crossref, Medline, Google Scholar
70. Osuntokun BO, Sahota A, Ogunniyi AO, et al: Lack of an association between apolipoprotein E epsilon 4 and Alzheimer's disease in elderly Nigerians. Annals of Neurology 38:463-465, 1995Crossref, Medline, Google Scholar
71. Devasenapathy A, Hachinski V: Vascular cognitive impairment: a new approach, in Advances in Old Age Psychiatry: Chromosomes to Community Care. Edited by Holmes C, Howard R. Bristol, Penn, Wrightson, 1997Google Scholar
72. Steingart A, Hachinski VC, Lau C, et al: Cognitive and neurologic findings in demented patients with diffuse white matter lucencies on computed tomographic scan (leuko-araiosis). Archives of Neurology 44:36-39, 1987Crossref, Medline, Google Scholar
73. Hofman A, Ott A, Breteler MMB, et al: Atherosclerosis, apolipoprotein E, and prevalence of dementia and Alzheimer's disease in the Rotterdam study. Lancet 349:151-154, 1997Crossref, Medline, Google Scholar
74. Snowdon DA, Greiner LH, Mortimer JA, et al: Brain infarction and the clinical expression of Alzheimer disease: the nun study. JAMA 277:813-817, 1997Crossref, Medline, Google Scholar
75. Skoog I: Risk factors for vascular dementia: a review. Dementia 5:137-144, 1994Medline, Google Scholar
76. Skoog I, Hesse C, Aevarsson O, et al: A population study of apoE genotype at the age of 85: relation to dementia, cerebrovascular disease, and mortality. Journal of Neurology, Neurosurgery, and Psychiatry 64:37-43, 1998Crossref, Medline, Google Scholar
77. Beresford T, Gomberg E: Alcohol and Aging. New York, Oxford University Press, 1995Google Scholar
78. Adams WL: Alcohol use in retirement communities. Journal of the American Geriatrics Society 44:1082-1085, 1996Crossref, Medline, Google Scholar
79. Adams WL, Barry KL, Fleming MF: Screening for problem drinking in older primary care patients. JAMA 276:1964-1967, 1996Crossref, Medline, Google Scholar
80. Grant BF, Harford TC, Chou P, et al: Prevalence of DSM-III-R alcohol abuse and dependence: United States, 1988. Alcohol and Health Research World 15:91-96, 1991Google Scholar
81. DeFranco C, Tarbox AR, McLaughlin EJ: Cognitive deficits as a function of alcohol abuse. American Journal of Drug and Alcohol Abuse 11:279-293, 1985Crossref, Medline, Google Scholar
82. Colsher PL, Wallace RB: Elderly men with histories of heavy drinking: correlates and consequences. Journal of Studies on Alcohol 51:528-535, 1990Crossref, Medline, Google Scholar
83. Tivis R, Beatty WW, Nixon SJ, et al: Patterns of cognitive impairment among alcoholics: are there subtypes? Alcoholism: Clinical and Experimental Research 39:496-500, 1995Google Scholar
84. Brandt J, Butters N, Ryan C, et al: Cognitive loss and recovery in long-term alcoholics. Archives of General Psychiatry 40:435-442, 1983Crossref, Medline, Google Scholar
85. Graves AB, van Dujin CM, Chandra V, et al: Alcohol and tobacco consumption as risk factors for Alzheimer's disease: a collaborative re-analysis of case-control studies. International Journal of Epidemiology 20:48-57, 1991Crossref, Google Scholar
86. Hebert LE, Scherr PA, Beckett LA, et al: Relation of smoking and alcohol consumption to incident Alzheimer's disease. American Journal of Epidemiology 135:347-355, 1992Crossref, Medline, Google Scholar
87. Mellinger GD, Balter MB, Uhlenhuth EH: Prevalence and correlates of the long-term regular use of anxiolytics. JAMA 251:375-379, 1984Crossref, Medline, Google Scholar
88. Ostrom JR, Hammarlund ER, Christensen DB, et al: Medication usage in an elderly population. Medical Care 23:157-164, 1985Crossref, Medline, Google Scholar
89. Draper B: Suicidal behavior in the elderly. International Journal of Geriatric Psychiatry 9:655-661, 1994Crossref, Google Scholar
90. Lexicon of Alcohol and Drug Terms. Geneva, World Health Organization, 1994Google Scholar
91. Campbell AJ, McCosh L, Reinken J: Drugs taken by a population based sample of subjects 65 years and over in New Zealand. New Zealand Medical Journal 96:378-380, 1983Medline, Google Scholar
92. Kail B: Drugs, gender, and ethnicity: is the older woman at risk? Journal of Drug Issues 29:171-189, 1989Google Scholar
93. Cottler LB, Robins LN: The prevalence and characteristics of psychoactive medication use by a general population survey. Psychopharmacology Bulletin 19:746-751, 1983Google Scholar
94. Hall MM: Epidemiological examination of the relationship between psychotherapeutic medicine use and disability in the elderly. Unpublished doctoral dissertation. Baltimore, Johns Hopkins University School of Hygiene and Public Health, 1993Google Scholar
95. Trinkoff AM, Anthony JC, Munoz A: Predictors of the initiation of psychotherapeutic medicine use. American Journal of Public Health 80:61-65, 1990Crossref, Medline, Google Scholar
96. Escobar JI, Anthony JC, Canino G, et al: Use of neuroleptics, antidepressants, and lithium by US community populations. Psychopharmacology Bulletin 23:196-200, 1987Medline, Google Scholar
97. Klinkman MS, Okkes I: Mental health problems in primary care: a research agenda. Journal of Family Practice 47:379-384, 1998Medline, Google Scholar
98. Gallo JJ, Marino S, Ford D, et al: Filters on the pathway to mental health care: II. sociodemographic factors. Psychological Medicine 25:1149-1160, 1995Crossref, Medline, Google Scholar
99. Cooper-Patrick L, Gallo JJ, Powe NR, et al: Mental health service utilization by African-Americans and whites: the Baltimore Epidemiologic Catchment Area follow-up. Medical Care, in pressGoogle Scholar
100. Rabins PV: Barriers to diagnosis and treatment of depression in elderly patients. American Journal of Geriatric Psychiatry 4(suppl 1):S79-S83, 1996Google Scholar



