Prediction of Homelessness Within Three Months of Discharge Among Inpatients With Schizophrenia
Abstract
OBJECTIVE: The authors' goal was to identify factors that place inpatients with schizophrenia at risk of becoming homeless after hospital discharge. METHODS: Patients with schizophrenia or schizoaffective disorder (N=263) were assessed at discharge from general hospitals in New York City and reassessed three months later to evaluate whether they had become homeless. Sociodemographic and clinical characteristics associated with homelessness were identified using likelihood ratio chi square analysis and logistic regression. RESULTS: Twenty patients (7.6 percent) reported an episode of homelessness during the follow-up period. Patients who had a drug use disorder at hospital discharge were significantly more likely to report becoming homeless than those without a drug use disorder. Patients with a total score above 40 on the Brief Psychiatric Rating Scale (BPRS) at hospital discharge were more likely to report becoming homeless than patients with lower scores, as were those with Global Assessment Scores less than 43. Twelve of 30 patients with a drug use disorder, a BPRS score above 40, and a GAS score less than 43 at hospital discharge reported becoming homeless. CONCLUSIONS: The combination of a drug use disorder, persistent psychiatric symptoms, and impaired global functioning at the time of hospital discharge poses a substantial short-term risk of homelessness among patients with schizophrenia. Patients who fit this profile may be candidates for community-based programs that are specifically aimed at preventing homelessness among patients with severe mental illness.
Homelessness among patients with severe mental illness remains one of the most challenging problems faced by providers of psychiatric services. The risk of becoming homeless for persons with schizophrenia and related disorders is more than ten times greater than the risk for the general population (1,2). Those who become homeless are commonly exposed to severe psychological stress, as well as a range of serious physical health hazards including extremes in temperature (3), violence (4), nutrition-related health problems (5), and potentially life-threatening infectious disease (6,7).
Several models of care have been developed to help prevent or reduce homelessness among patients with severe mental illness (8,9,10,11). One particularly promising model, critical time intervention, involves frequent community contacts with a case worker during the period after discharge from institutional care (12). The case worker attempts to strengthen the patient's ties to the mental health and social services systems, shore up family support, and provide emotional and practical support. In a recent randomized controlled trial, patients who received critical time intervention averaged 67 percent fewer homeless nights after discharge from a homeless shelter than patients who received usual care (8).
The first weeks after discharge from a hospital or other institution are widely believed to be a period of increased risk of homelessness for patients with severe mental disorders (13). The environment may place new demands on the patient when the symptoms that contributed to the patient's institutional placement have not fully resolved. Clinicians who work in institutional settings are routinely confronted with the difficult task of trying to select patients at high risk of becoming homeless so that special efforts can be made to provide stable housing and strong linkages to community support services.
Most research on individual risk factors of homelessness in psychiatrically ill populations have been cross-sectional studies that compare the characteristics of homeless and domiciled patients (14,15,16,17). These studies have implicated elevated clinical symptoms (14,16), substance abuse (14,15,16), medication noncompliance (14,15,16), and contact with the criminal justice system (17) as possible risk factors for homelessness. However, such cross-sectional research does not permit a clear separation of cause from effect. Elevated psychiatric symptoms among homeless subjects, for example, may be a direct cause of housing loss or a secondary consequence of the extreme stress of homelessness. A prospective longitudinal design is needed to help clarify the role of individual characteristics in the etiology of homelessness among patients with severe mental illness and to help identify patients at high risk of becoming homeless.
A recently published prospective longitudinal study supported the role of current substance abuse as a mediating factor in homelessness among severely ill psychiatric patients (9). In this study, homeless adults with severe mental illness and a substance use disorder were followed for 18 months after they enrolled in a program that provided integrated dual diagnosis services in combination with supportive housing. Although none of the clinical factors that were evaluated at program intake predicted subsequent housing status, a lack of progress toward recovery from substance abuse at the intermediate assessment points predicted failure to achieve stable housing at the final follow-up point.
In the study reported here, we examined associations between individual patient characteristics assessed at the time of hospital discharge and the occurrence of homelessness over a three-month period in a broadly representative group of inpatients with schizophrenia or schizoaffective disorder. We examined sociodemographic characteristics, symptom level, global functioning, substance use, previous homelessness, medication noncompliance, and legal history as predictors of homelessness.
In line with previous research, we hypothesized that comorbid substance use disorders and more severe psychiatric symptoms at hospital discharge would predict homelessness (8,14,15,16). We anticipated that symptoms that seriously disrupt interpersonal relations, such as paranoia or a tendency toward aggression, would be most likely to jeopardize housing arrangements. Because treatment refusal is common among homeless mentally ill patients (15,17,18), we further expected that involuntary hospitalization and a recent history of medication noncompliance would predict homelessness. Finally, we hypothesized that patients with a recent history of homelessness would be at increased risk of homelessness after hospital discharge.
Methods
Data for this analysis were drawn from the longitudinal patient outcome phase of the Rutgers hospital and community survey. The methods and primary objectives of this survey have been described elsewhere (19). A primary aim was to examine the relationship between psychiatric care in general hospitals and outcomes for Medicaid patients with schizophrenia and related disorders.
Eligibility
Eligible subjects were English-speaking, newly admitted psychiatric inpatients, between ages 18 and 64, who were enrolled in or eligible for Medicaid and who had an admitting clinical diagnosis of schizophrenia or schizoaffective disorder. Subjects were entered in the study if they provided written informed consent and if they met criteria for schizophrenia or schizoaffective disorder according to the Structured Clinical Interview for DSM-III-R (SCID) (20), updated to include DSM-IV criteria, as administered by a trained research assistant. For the sake of brevity, in this report these patients are referred to as having schizophrenia rather than schizophrenia or schizoaffective disorder.
Patients suffering from a severe and highly disabling general medical condition were ineligible for the study. Subjects who had stays longer than 120 days, who were discharged against medical advice, or who were transferred to another inpatient psychiatric facility were also excluded from the study.
Subject recruitment and selection
Subject recruitment occurred in several phases. A total of 1,328 patients who were consecutively admitted to four general hospitals in New York City from October 1994 to April 1996 were prescreened and found to meet the age, payer status, and clinical diagnosis eligibility criteria. Based on medical records and discussions with inpatient staff, we eliminated 4 percent of the screened sample due to severe general medical conditions, 4 percent who lived outside of New York City, and 9 percent who did not speak or understand English.
A total of 1,010 screened patients (76 percent) were therefore assessed as eligible to receive the diagnostic interview. Of this group, 57 percent (N=576) agreed to be interviewed, 31 percent (N=310) refused, and 12 percent (N=124) were not approached because they were discharged before a diagnostic interview could be scheduled. Of the 576 patients who consented to the diagnostic interview, 68 percent (N=394) met DSM-IV criteria for schizophrenia or schizoaffective disorder. Of the patients who met the diagnostic criteria, 71 were excluded from the baseline assessment because they left the hospital against medical advice, were transferred to another inpatient facility, had a length of stay of greater than 120 days, or withdrew their consent. The baseline inpatient assessment was administered to 323 patients and was completed by 316 patients.
The sample of 316 patients and 694 nonselected screened patients did not differ significantly in age, sex, ethnicity, marital status, or recent work history. In addition, a similar proportion of the two groups reported active drug use (42 percent and 38 percent) or active alcohol use (38 percent and 39 percent) before admission. However, in the sample of 316 patients, blacks were overrepresented (58 percent, compared with 42 percent in the nonselected group of screened patients), and whites and Asians were underrepresented (whites, 40 percent, compared with 49 percent in the overall group, and Asians, 2 percent, compared with 9 percent in the overall group). Patients in the selected sample were also significantly more likely than those in the nonselected group of screened patients to report at least one previous psychiatric hospitalization (93 percent, compared with 86 percent).
Of the 316 patients who entered the study, 263 (83 percent) were located for a three-month follow-up reassessment. Patient tracking involved telephone and mail reminders to patients, their clinicians, and other community contacts. The group lost to follow-up did not significantly differ from the follow-up group in age, sex, race, or score on the Brief Psychiatric Rating Scale (BPRS) (21) or Global Assessment Scale (GAS) (22) at the baseline interview.
Assessments
Within 72 hours of hospital discharge, patients completed a structured assessment that covered several domains, including clinical symptoms, global functioning, substance use disorders, legal history, and sociodemographic characteristics. Patients' clinical symptoms were assessed by a research assistant using the BPRS and the Center for Epidemiological Studies—Depression Scale (CES-D) (23). Global functioning was evaluated using the GAS. DSM-III-R substance use disorders during the past six months were assessed using the Mini-International Neuropsychiatric Interview (24). Previous research has demonstrated a high concordance between the Mini-International Neuropsychiatric Interview and the SCID for these diagnoses (25). Three months after hospital discharge patients were re-interviewed with the same instruments to assess changes over the follow-up period in the various outcome domains as well as housing status.
Homelessness
At the follow-up interview, patients who were not currently homeless were asked if they had been homeless for any period during the three months since they were discharged from the hospital. People who reported that they had been homeless for more than one night were asked a follow-up question to determine the number of days, weeks, or months that they had been homeless. Patients who were homeless at the time of the interview were not asked these two questions.
Homelessness was defined as living on the street or in a park, bus station, abandoned building, or similar setting. It did not include living in jail, a shelter, a rooming house, or other noncongregate living situations. In the following analyses, patients who reported that they were homeless during the follow-up period (N=17) or were homeless at the time of the follow-up interview (N=3) are considered to have become homeless.
Analytic strategy and statistical methods
Our primary goal was to identify patients with schizophrenia at high risk of homelessness during the three months after hospital discharge. We began by stratifying the sample by sociodemographic and clinical characteristics. Specifically, the sample was stratified by age, sex, race, marital status, education, location before admission, employment status, total and subscale BPRS scores (26) at hospital discharge, GAS score at hospital discharge, CES-D score at hospital discharge, legal history, and history of homelessness, substance use disorder, and treatment noncompliance.
A range of cutoff scores was examined for the BPRS, GAS, and CES-D scales, and likelihood ratio chi square analysis was used to select scores that most clearly discriminated patients who became homeless from those who were continuously domiciled. The proportion of patients in each strata who became homeless was then determined, and 95 percent confidence intervals were calculated around these proportions. A logistic regression analysis was conducted to examine the independent association of selected significant predictors of homelessness with becoming homeless at some point during the 12-week period after hospital discharge. Patients' age, sex, and race were entered as covariates into this equation.
Results
General characteristics
Twenty of the 263 study patients (7.6 percent) reported an episode of homelessness during the three-month follow-up period. The mean period of homelessness was 27.8± 26.5 days. At the time of the follow-up interview, three of these 20 patients were homeless, eight patients were living in a shelter, four in a private house or apartment, two in a hospital, and three in congregate living situations such as a rooming house or an adult home. There were no significant differences in the proportion of patients who became homeless and those who did not within the selected sociodemographic categories shown in Table 1.
Clinical characteristics
Table 2 reports the rates of homelessness among patients who scored above or below the cutoff scores for the various clinical measures. Patients with total BPRS scores above 40 at hospital discharge were significantly more likely to become homeless than those with lower scores (14.9 percent, compared with 1.6 percent). Further analysis revealed that patients with scores above 8 on the hostility-suspicion subscale of the BPRS were significantly more likely to become homeless than lower-scoring patients (16.7 percent, compared with 4.7 percent). The hostility-suspicion subscale includes three items—hostility, suspiciousness, and uncooperativeness—and has a theoretical range from 3, not reported, to 21, very severe.
Patients with GAS scores below 43 at hospital discharge were also significantly more likely to become homeless, compared with patients with higher scores (13.4 percent, compared with 2.2 percent). A score of 43 is in the range of serious symptoms or serious impairment in functioning.
Table 3 shows the rates of homelessness among patients by history and various diagnostic characteristics. Patients who met criteria for DSM-III-R alcohol abuse or dependence were no more likely than patients without those disorders to become homeless, but patients with a DSM-III-R drug abuse or dependence disorder were at a significantly higher risk of becoming homeless than patients without a drug use disorder. Nearly one in five patients with a drug use disorder at the time of hospital discharge (18.7 percent) spent at least one homeless night during the three months after hospital discharge.
None of the other clinical factors examined were associated with a significantly increased risk of becoming homeless. The combination of a substance use disorder, a BPRS score above 40, and a GAS score below 43 was associated with particularly high risk of becoming homeless. Forty percent of patients with these characteristics (12 of 30 patients) spent at least one night without housing during the three-month follow-up period.
Predictors of homelessness
A logistic regression analysis in which patients' age, sex, and race were controlled showed that BPRS score at hospital discharge was significantly associated with the patients' subsequently reporting a period of homelessness. In this analysis, a 1-point increase in BPRS score increased the estimated relative risk of becoming homeless by 6.5 percent (odds ratio [OR]=1.07, 95 percent confidence interval [CI]=1.02 to 1.11). For each 1-point decrease in GAS score at hospital discharge, the estimated relative risk of becoming homeless increased by 5.9 percent (OR=1.06, CI=1.01 to 1.10) when the analysis controlled for demographic factors. A diagnosis of a substance use disorder was associated with an approximate sixfold increase in the risk of becoming homeless (OR=6.1, CI=2.0 to 18.4) after the analysis adjusted for patients' age, sex, and race.
In a separate model that also controlled for these three demographic factors, substance use disorder (OR= 6.7, CI=2.2 to 20.8) remained strongly associated with becoming homeless. However, baseline BPRS and GAS scores were no longer significantly related to becoming homeless.
Discussion and conclusions
We found that the risk of becoming homeless following hospital discharge was significantly increased for patients with schizophrenia who had a comorbid drug use disorder, elevated psychiatric symptoms, or poor global functioning at the time of hospital discharge. The combination of these three characteristics placed individuals at an especially high risk of becoming homeless. Twelve of 30 such patients spent at least one night without housing during the three-month follow-up period. These 12 patients accounted for a majority of the patients who reported becoming homeless during the follow-up period. A high level of clinical attention should be given to the possibility of future homelessness among multiply impaired inpatients with schizophrenia who have comorbid drug use and continue to have marked symptoms and functional impairment at the time of hospital discharge.
The strong association between comorbid drug use disorders and subsequent homelessness supports and extends earlier longitudinal research (8) and cross-sectional (14,16) research. Abuse of illicit drugs may exacerbate the symptoms of schizophrenia (27,28), which in turn threatens the stability of housing arrangements. In the treatment of patients with schizophrenia complicated by substance use, discharge planning should proceed with careful attention to the attendant risks of homelessness. Unfortunately, these are the very patients who may be at greatest risk of receiving the least adequate discharge planning (13).
Inpatient staff who determine that a patient is at high risk in the near-term of becoming homeless should try to connect the patient to supportive outpatient services that help smooth the transition to community living. The previously mentioned critical time intervention model (8) approaches this problem by helping patients develop relationships with community providers, who in turn offer ongoing care and support (29). The critical time intervention is intensive but extends only to a maximum of nine months from the time the individual leaves the institution. Case workers individually tailor their services around four areas thought to be critical for housing stabilization: containment of substance abuse, maintenance of medication compliance, appropriate money management, and prevention of housing-related crises (30). The current findings suggest that symptom control may be another important focus of care to help prevent homelessness in this patient population.
Although several investigators have reported a cross-sectional association between alcoholism and homelessness in psychiatrically ill populations (15,16,18), we did not find that a history of alcohol use disorders increased the risk of homelessness. It is possible that the relatively small size of the homeless sample and the high base rate of alcohol use disorders explain the lack of association in this study.
The finding that patients with higher psychiatric symptom scores are at risk of subsequent homelessness suggests that psychiatric symptoms play an etiologic role in the loss of housing by patients with schizophrenia. Although the BPRS hostility-suspicion symptom cluster was most closely linked to homelessness, the logistic regression analysis showed that this cluster did not improve prediction of homelessness beyond the total BPRS score. A structured assessment of psychiatric symptoms near the time of planned hospital discharge may help inpatient staff determine which patients are at greatest risk of losing their housing after discharge. For high-risk patients, particular attention should be given to selecting appropriate housing arrangements and outpatient services.
The association we found between high BPRS scores and short-term homelessness may also weigh in clinical decisions about pharmacologic management. In the treatment of schizophrenia, there is evidence that the atypical antipsychotics olanzapine (31), risperidone (32), and clozapine (33) are superior to conventional antipsychotics in lowering BPRS scores. More specifically, patients treated with risperidone have been found to be more likely than those treated with perphenazine to achieve a substantial reduction in score on the hostility-suspicion subscale of the BPRS (32).
Several factors that we hypothesized would predict homelessness did not reach the level of statistical significance. They included a history of noncompliance with antipsychotic medications, homelessness before the index hospitalization, and a history of contact with the criminal justice system. However, for each variable, a nonsignificant trend toward an increased risk of homelessness was noted. In general, the risk of becoming homeless tended to be more strongly tied to aspects of the patient's clinical status at hospital discharge than to aspects of the patient's clinical history. An important exception to this tendency was the association between drug use disorders during the six months before hospital admission and the risk of homelessness after hospital discharge.
The current findings are constrained by several important limitations. First, we relied exclusively on patient reports to determine housing status. Problems with patient recall and conscious factual distortions may have introduced inaccuracies in our measurements. Second, only short-term follow-up data were available. A longer follow-up period might have yielded a larger number of patients who became homeless and a different risk profile.
Third, we did not collect information on the reasons that patients became homeless or the processes that link the identified risk factors to loss of housing. Fourth, the sample was limited by patients' refusal to participate, attrition, and exclusion of certain patient groups, such as those who left the hospital against medical advice. The combined effect of these factors may have reduced the observed rate of homelessness below what would have been found with more representative sampling and more complete follow-up. Finally, the subjects were drawn from four urban hospitals, and the results may not generalize to inpatients treated in suburban or rural settings.
It is unreasonable to think that the problems faced by homeless individuals with schizophrenia can be solved by the mental health system alone. Attention clearly must be paid to the broader housing and social welfare issues that affect all homeless individuals. However, mental health professionals do have opportunities to identify patients at high risk of becoming homeless and to coordinate aggressive preventive measures. Among inpatients with schizophrenia, the combination of a current drug use disorder, persisting clinical symptoms, and poor functioning at the time of hospital discharge appears to pose just such a risk.
Acknowledgments
This research was supported by a grant from the Robert Wood Johnson Foundation and grant MH-43450 from the National Institute of Mental Health.
The authors are affiliated with the Institute for Health, Health Care Policy, and Aging Research at Rutgers University in New Brunswick, New Jersey. Dr. Olfson is also associate professor in the department of psychiatry at Columbia University College of Physicians and Surgeons at the New York State Psychiatric Institute, 1051 Riverside Drive, New York, New York 10032 (e-mail, [email protected] ).
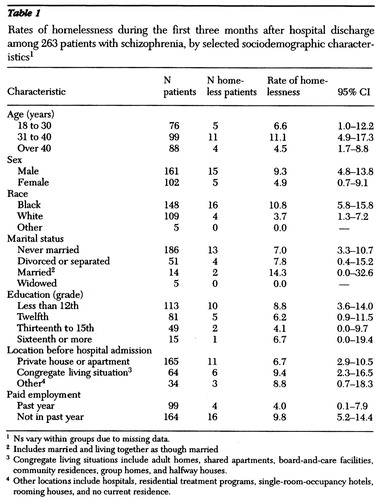 |
Table 1. Rates of homelessness during the first three months after hospital discharge among 263 patients with schizophrenia, by selected sociodemographic characteristics1
1 Ns vary within groups due to missing data.
2 Includes married and living together as though married
3 Congregate living situations include adult homes, shared apartments, board-and-care facilities, community residences, group homes, and halfway houses.
4 Other locations include hospitals, residential treatment programs, single-room-occupancy hotels, rooming houses, and no current residence.
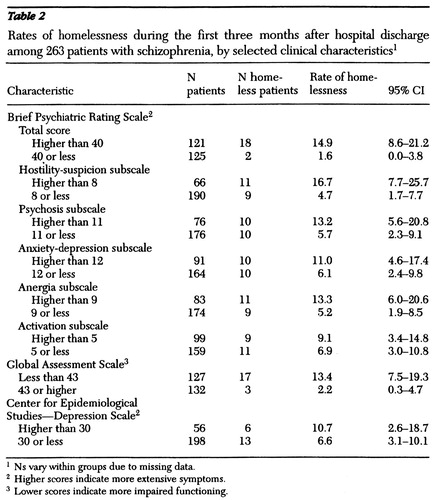 |
Table 2. Rates of homelessness during the first three months after hospital discharge among 263 patients with schizophrenia, by selected clinical characteristics1
1 Ns vary within groups due to missing data.
2 Higher scores indicate more extensive symptoms.
3 Lower scores indicate more impaired functioning.
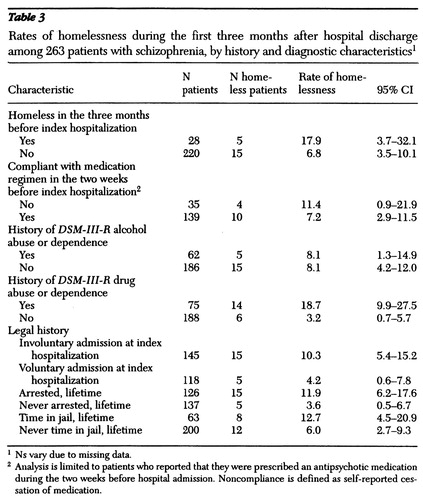 |
Table 3. Rates of homelessness during the first three months after hospital discharge among 263 patients with schizophrenia, by history and diagnostic characteristics1
1 Ns vary due to missing data.
2 Analysis is limited to patients who reported that they were prescribed an antipsychotic medication during the two weeks before hospital admission. Noncompliance is defined as self-reported cessation of medication.
1. Susser E, Moore R, Link B: Risk factors for homelessness. Epidemiologic Reviews 15:546-556, 1993Medline, Google Scholar
2. Susser ES, Lin SP, Conover S: Risk factors for homelessness among patients admitted to a state mental hospital. American Journal of Psychiatry 148:1659-1664, 1991Link, Google Scholar
3. Cohen NL, Putnam JF, Sullivan AM: The mentally ill homeless: isolation and adaptation. Hospital and Community Psychiatry 35:922-924, 1984Abstract, Google Scholar
4. Padgett DK, Struening EL, Andrews H, et al: Predictors of emergency room use by homeless adults in New York City: the influence of predisposing, enabling, and need factors. Social Science and Medicine 41:547-556, 1995Crossref, Medline, Google Scholar
5. Luder E, Boey E, Buchalter B, et al: Assessment of the nutritional status of urban homeless males. Public Health Reports 104:451-457, 1989Medline, Google Scholar
6. Geldberg L, Panarites CJ, Morgenstern H, et al: Tuberculosis skin testing among homeless adults. Journal of General Internal Medicine 12:25-33, 1997Crossref, Medline, Google Scholar
7. Susser E, Miller M, Valencia E, et al: Injection drug use and risk of HIV transmission among homeless men with mental illness. American Journal of Psychiatry 153:794-798, 1996Link, Google Scholar
8. Susser E, Valencia E, Conover S, et al: Preventing recurrent homelessness among mentally ill men: a "critical time" intervention after discharge from a shelter. American Journal of Public Health 87:256-262, 1997Crossref, Medline, Google Scholar
9. Bebout RR, Drake RE, Xie H, et al: Housing status among formerly homeless dually diagnosed adults. Psychiatric Services 48:936-941, 1997Link, Google Scholar
10. Dixon LB, Krauss N, Kernan E, et al: Modifying the PACT model to serve homeless persons with severe mental illness. Psychiatric Services 46:684-688, 1995Link, Google Scholar
11. Leda C, Rosenheck R: Mental health status and community adjustment after treatment in a residential treatment program for homeless veterans. American Journal of Psychiatry 149:1219-1224, 1992Link, Google Scholar
12. Caton CL, Wyatt RJ, Grunberg J, et al: An evaluation of a mental health program for homeless men. American Journal of Psychiatry 147:286-289, 1990Link, Google Scholar
13. Caton CLM: Mental health service use among homeless and never-homeless men with schizophrenia. Psychiatric Services 46:1139-1143, 1995Link, Google Scholar
14. Opler LA, Caton CLM, Shrout P, et al: Symptom profiles and homelessness in schizophrenia. Journal of Nervous and Mental Disease 182:174-178, 1994Crossref, Medline, Google Scholar
15. Drake RE, Wallach MA, Hoffman JS: Housing instability and homelessness among aftercare patients of an urban state hospital. Hospital and Community Psychiatry 40:46-51, 1989Abstract, Google Scholar
16. Caton CLM, Shrout PE, Dominguez B, et al: Risk factors for homelessness among women with schizophrenia. American Journal of Public Health 85:1153-1156, 1995Crossref, Medline, Google Scholar
17. Appleby L, Desai P: Documenting the relationship between homelessness and psychiatric hospitalization. Hospital and Community Psychiatry 36:732-737, 1985Abstract, Google Scholar
18. Drake RE, Wallach MA, Teague GB, et al: Housing instability and homelessness among rural schizophrenic patients. American Journal of Psychiatry 148:330-336, 1991Link, Google Scholar
19. Boyer CA, Olfson M, Kellermann SL, et al: Studying inpatient treatment practice in schizophrenia: an integrated methodology. Psychiatric Quarterly 66:293-320, 1995Crossref, Medline, Google Scholar
20. Spitzer RL, Williams JBW, Gibbon M: Structured Clinical Interview for DSM-III-R: Patient Education (SCID-P, Version 1.0). Washington, DC, American Psychiatric Association, 1990Google Scholar
21. Overall JE, Gorham DP: Brief Psychiatric Rating Scale. Psychological Reports 10:799-807, 1962Crossref, Google Scholar
22. Endicott J, Spitzer RL, Fleiss JL, et al: The Global Assessment Scale. Archives of General Psychiatry 33:766-771, 1976Crossref, Medline, Google Scholar
23. Radloff LS: The CES-D scale: a self-report depression scale for research in the general population. Applied Psychological Measurement 1:385-401, 1977Crossref, Google Scholar
24. Sheehan D, Janavs J, Knapp E, et al: Mini-International Neuropsychiatric Interview, Clinical Rated, Version 4.0, Tampa, University of South Florida College of Medicine, 1992Google Scholar
25. Sheehan DV, Lecrubier Y, Janavs J, et al: Reliability and validity of the Mini-International Neuropsychiatric Interview (MINI) according to the SCID-P. Presented at the New Clinical Drug Evaluation annual meeting, Orlando, Fla, May 31, 1995Google Scholar
26. Guy W: ECDEU Assessment Manual for Psychopharmacology, rev ed. Washington, DC, US Department of Health, Education, and Welfare, 1976Google Scholar
27. Haywood TW, Kravits HM, Grossman LS, et al: Predicting the "revolving door" phenomenon among patients with schizophrenic, schizoaffective, and affective disorders. American Journal of Psychiatry 152:856-861, 1995Link, Google Scholar
28. Negroid J, Knoop WP, Douglas DE, et al: Cannabis affects the severity of schizophrenic symptoms: results of a clinical survey. Psychological Medicine 16:515-520, 1986Crossref, Medline, Google Scholar
29. Valenica E, Susser E, McQuistion H: Critical time points in the clinical care of homeless mentally ill individuals, in Practicing Psychiatry in the Community: A Manual. Edited by Vaccaro JV, Clarke GH Jr. Washington, DC, American Psychiatric Press, 1996Google Scholar
30. Jones K, Colson P, Valencia E, et al: A preliminary cost-effectiveness analysis of an intervention to reduce homelessness among the mentally ill. Psychiatric Quarterly 65:243-256, 1994Crossref, Medline, Google Scholar
31. Tollefson GD, Beasley CM, Street JS, et al: Olanzapine versus haloperidol in the treatment of schizophrenia and schizoaffective and schizophreniform disorders: results of an international collaborative trial. American Journal of Psychiatry 154:457-465, 1997Link, Google Scholar
32. Hoyberg OJ, Fensbo C, Remvig J, et al: Risperidone versus perphenazine in the treatment of chronic schizophrenic patients with acute exacerbations. Acta Psychiatrica Scandinavica 88:395-402, 1993Crossref, Medline, Google Scholar
33. Hagger C, Buckley P, Kenny JT, et al: Improvement in cognitive functions and psychiatric symptoms in treatment-refractory schizophrenic patients receiving clozapine. Biological Psychiatry 34:702-712, 1993Crossref, Medline, Google Scholar



