Rehab Rounds: Improving Pharmacotherapy in a Psychiatric Hospital
Abstract
Introduction by the column editors: Rehabilitation of persons with severe mental disorders is of necessity a biobehavioral endeavor, with control and stabilization of symptoms the foundation for helping individuals achieve their personal goals through building skills and providing social support. Several recent studies have documented the importance of minimizing symptoms and maximizing cognitive functioning to ready individuals for rehabilitation services (1,2). Because of the key role of pharmacotherapy in the management, reduction, or removal of symptoms as obstacles to the attainment of the individual's rehabilitation goals, it is essential that drug interventions be of high quality. However, recent studies of drug-prescribing practices for severely mentally ill patients have documented the inadequacies of this essential first stage of rehabilitation (3,4).In this month's column, Robert E. Moebius, M.D., and colleagues who worked with him at Camarillo State Hospital describe several quality improvement programs that were instituted at the facility to raise the quality of pharmacotherapy provided by the staff psychiatrists and physicians. Also highlighted are the clinical benefits that can result from the formation of an alliance between a public mental health institution and an academic medical center. The success of this public-academic liaison led to the hospital's receiving an award from the American Psychiatric Association in 1991 for excellence in state-academic collaboration.
The Camarillo State Hospital and Developmental Center in southern California, an institution serving as a tertiary back-up treatment facility for a large catchment area of several million people, developed a public-academic affiliation with the School of Medicine of the University of California, Los Angeles (UCLA), in the late 1960s. Over the years, this relationship provided numerous benefits to both organizations, including expanded opportunities for UCLA researchers to study a population with treatment-refractory mental illness and for clinicians at the hospital to gain experience with innovative biobehavioral treatment methods.
This column focuses on the quality improvement programs instituted at Camarillo State Hospital to raise the level of pharmacotherapy provided by the staff psychiatrists and physicians. These programs included annual psychopharmacology update courses that culminated in an examination and weekly grand rounds that often focused on the challenges posed by patients whose illnesses were refractory to medications. In addition, a psychopharmacology consultation team was made available for reviews and recommendations for patients exhibiting suboptimal clinical progress, and drug utilization reviews were conducted by clinical pharmacists after consensus was reached with the medical staff on problems to target.
The quality improvement programs
Annual psychopharmacologyupdate seminar
For more than two decades, the first author served as chief of professional education at Camarillo State Hospital. In this capacity, he sponsored an annual seminar aimed at updating the psychopharmacology knowledge and skills of the psychiatrist staff as well as the nonpsychiatrist physicians who were often assigned to treat individuals with developmental disorders at this institution. The psychiatric residents searched the current literature and made written and verbal presentations that were available to the entire medical staff. Each resident typically selected one topic area, such as antipsychotics or mood stabilizers, for his or her presentation.
At the end of the seminar series, a comprehensive examination was given to all medical staff. To maintain clinical privileges, all medical staff were expected to demonstrate a reasonable level of proficiency on the test. Clinicians who had poor scores received counseling and peer tutoring until they took the test again and obtained a satisfactory score. Table 1 shows some of the questions from the annual examinations.
Grand rounds in psychopharmacology
Grand rounds complemented the annual psychopharmacology seminar. Over 20 years, the hospital held 772 grand rounds in which notable academic psychiatrists lectured on topics related to drug treatment. Moreover, because of the hospital's academic affiliation with the UCLA School of Medicine, experts in the treatment of patients with severe mental illness who lectured during grand rounds also participated routinely in the discussion of cases at the hospital. These psychopharmacology experts included Philip R. A. May, M.D., Theodore Van Putten, M.D., Stephen R. Marder, M.D., William Wirshing, M.D., and George Simpson, M.D.
Based on the grand rounds, a course was designed to prepare staff psychiatrists to take and pass the national boards in psychiatry and neurology. This endeavor was remarkably successful; 25 physicians passed the boards, and most of them remained on staff at the hospital afterward to share their expertise.
Psychopharmacology consultation team
From 1980 to 1996, an active psychopharmacology consultation team made biweekly rounds on the wards and units at Camarillo State Hospital. As the years passed, an increasing number of referrals came to this team, which comprised UCLA faculty who were conducting clinical research at the hospital, the hospital's chief of professional education, and selected clinical pharmacists and staff psychiatrists.
Because the hospital served a tertiary role in the state system of care, most of the patients had conditions that were refractory to conventional forms, doses, and combinations of medications. Many had both mental retardation and a psychotic disorder, and their very diagnosis defied easy categorization because they could not readily communicate verbally. In these cases, deviant and bizarre behaviors such as pacing, aggression, shouting, and grimacing were identified, and their criteria were operationalized. The criteria were then monitored while one or another medication was introduced to determine the effect on the frequency of the problem behaviors.
Many clinical problems were complicated by socioenvironmental contingencies of reinforcement and ward events and stimuli that triggered or maintained the abnormal behavior. To address these multifaceted issues, members of the psychopharmacology consultation team formed a biobehavioral treatment and rehabilitation team that made weekly rounds, reviewed the cases of difficult-to-treat patients, and assisted staff on the various units to construct joint behavior therapy and psychopharmacology treatment protocols. Protocols were developed for problems such as polydipsia, aggression, and borderline personality disorder (5).
Drug use evaluations
Drug use evaluations have been used in a variety of settings to identify opportunities to improve the use of drugs and to resolve problems associated with their use. Evaluations are also conducted to ensure that medications are used appropriately, safely, and effectively (6,7). The decision to formally evaluate a particular drug is often made because the agent causes adverse reactions or interacts adversely with other drugs, is more expensive than other drugs that can be used to treat the same disorder, or is used at a disproportionately high volume in a particular population.
The pharmacy department of a hospital or institution typically takes responsibility for conducting a drug use evaluation. The reviews are organized by particular audit criteria for sampling the use of the drug in a population. Audit criteria may include indications for the drug among the individuals in the population, precautions or eligibility determined through clinical or laboratory testing, adverse reactions, and therapeutic responses.
At Camarillo drug use evaluations began in earnest in 1990 when a review of all patients on benztropine was conducted. That evaluation resulted in a series of educational seminars designed to limit the prophylactic and indefinite use of this agent for patients receiving neuroleptics.
In 1991 a comprehensive review of treatment for seizures was done. Carbamazepine was found to be the most widely used antiseizure drug. Its untoward interactions with erythromycin were identified and discussed in educational sessions for the hospital's cadre of physicians. Another drug use evaluation yielded evidence of excessive use of phenobarbital as an antiseizure agent. This finding led to a concerted educational effort to reduce or terminate the prescribing of phenobarbital when it appeared therapeutically reasonable, resulting in improved cognitive functioning in affected patients.
In a drug use evaluation of lithium conducted in 1987, all patients in the hospital were surveyed for use of that agent. At that time, lithium had been the institution's most problematic drug in terms of side effects. Staff education on lithium's toxic interactions with other agents such as nonsteroidal anti-inflammatory drugs and angiotensin-converting enzyme inhibitors was accomplished, and the importance of periodically monitoring patients' renal and thyroid function was established. The drug use evaluation monitoring form for lithium included the safety checklist shown in Table 2.
A drug use evaluation of clozapine that began with the hospital's initial use of this drug resulted in close monitoring and no deaths from agranulocytosis, although some deaths did occur in other hospitals in the California state hospital system. The clozapine monitoring process identified frequent problems with clozapine-induced constipation and resulted in formulation of treatment guidelines for chronic constipation that were adopted by other institutions throughout the state.
Educational efforts derived from the findings of the drug use evaluations were included in the annual psychopharmacology updates, examinations, and grand rounds. In addition, a psychopharmacology advisory committee issued monthly pharmacy bulletins that conveyed information from the drug use evaluations as well as concise and practical information about new drugs that were being introduced into the hospital's formulary.
Benefits of systematic quality improvement
The drug use evaluations, as well as the annual psychopharmacology updates, examinations, consultation teams, and grand rounds contributed to a significant decline in adverse drug effects reported at the hospital over a ten-year period. The psychopharmacology update and examination was emulated by other state hospitals in California and was endorsed in 1996 by the National Board of Psychiatric Pharmacy. The psychopharmacology consultation team at Camarillo State Hospital was selected to draft the initial statewide guidelines for psychotropic drugs, which preceded by 15 years the treatment guidelines published by the American Psychiatric Association and other organizations. Over the succeeding years, these guidelines delineated methods for the use of clozapine, carbamazepine, and valproate that were promulgated throughout the state.
The Camarillo psychopharmacology program evolved into a statewide psychopharmacology advisory committee that has purview over a variety of issues that require problem solving. These issues include drug abuse at one of the state prisons, antiandrogen protocols at the state's forensic hospitals, treatment algorithms and guidelines for the use of typical versus atypical antipsychotic drugs, and the use of sildenafil citrate (Viagra) in state institutions.
Afterword by the column editors: It is no accident that the standards and methods for improving the quality of pharmacotherapy described here had their origin at Camarillo State Hospital and Developmental Center. Camarillo was the jewel in the crown of state hospitals. During the 1950s and 1960s the definitive study of neuroleptic drug therapy for schizophrenia was carried out by Philip May (8) at Camarillo. Subsequently, pioneering research and the development of biobehavioral treatments for schizophrenia were conducted at the Camarillo-UCLA Clinical Research Unit and disseminated throughout the hospital, the state, and the nation (9). Close and reciprocal working relationships between researchers and clinicians were a "given" at Camarillo; thus, the "town-gown" conflicts that have plagued other research units in state facilities were simply nonexistent at Camarillo.
Besides the active public-academic liaison, what other factors can explain the development of the quality improvement programs at Camarillo? Perhaps the most important consideration is the strong mandate for quality assurance from top management. For more than two decades, the executive and medical directors at Camarillo were champions for change and opponents of the status quo. The hospital leadership did more than pay lip service to quality assurance; they insisted on it through policies, procedures, promotions, job descriptions, performance standards, newsletters, positive reinforcement, and "management by walking around."
It is a sad commentary on the Machiavellian power politics of state bureaucracies that Camarillo State Hospital and Developmental Center was closed in 1997, despite having the best clinical programs and community placement statistics by far of any state hospital in California. The protests of professional and consumer stakeholders and advocates notwithstanding, a decision was made in the state capital to eliminate the only facility that had the dual functions of serving mentally ill and developmentally disabled patients, an organizational anomaly that worked extremely well at the clinical level but created awkwardness in shared governance for managers in the state headquarters.
Dr. Moebius is a consultant in psychiatry to the California Department of Developmental Services and is in private practice in Ventura County, California. Dr. Jones is a clinical pharmacist with the California Department of Developmental Services. Dr. Liberman is professor of psychiatry at the University of California, Los Angeles, School of Medicine and director of its Center for Research on Treatment and Rehabilitation of Psychosis. During the period described in this column, Dr. Moebius was chief of professional education at Camarillo (Calif.) State Hospital and Developmental Center. Dr. Jones was a senior clinical pharmacist, editor of the pharmacy bulletin, and organizer of the psychotropic drug audits at Camarillo State Hospital and Developmental Center. Dr. Liberman was director of the Camarillo-UCLA clinical research unit. Address correspondence to Dr. Liberman at 528 Lake Sherwood Drive, Thousand Oaks, California 91361 (e-mail, [email protected]). Dr. Liberman and Alex Kopelowicz, M.D., are editors of this column.
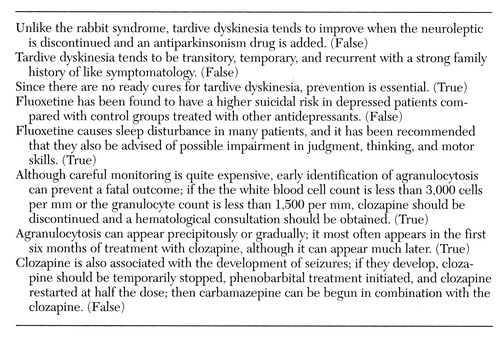 |
Table 1. Questions (and answers) from an annual psychopharmacology examination at Camarillo (Calif.) State Hospital and Developmental Center
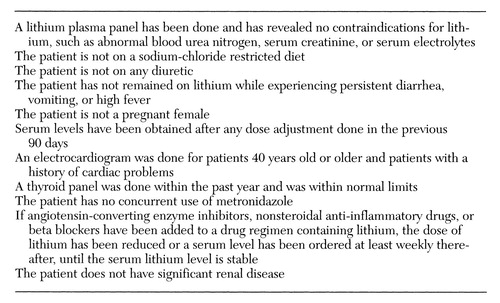 |
Table 2. Safety criteria for lithium from a drug use evaluation monitoring form used at Camarillo (Calif.) State Hospital and Developmental Center
1. Green MF: What are the functional consequences of neurocognitive deficits in schizophrenia? American Journal of Psychiatry 153:321-330, 1996Google Scholar
2. Anthony WA, Rogers ES, Cohen M, et al: Relationship between psychiatric symptomatology, work skills, and future vocational performance. Psychiatric Services 46:353- 358, 1995Link, Google Scholar
3. Young AS, Sullivan G, Burnam MA, et al: Measuring the quality of outpatient treatment for schizophrenia. Archives of General Psychiatry 55:611-617, 1998Crossref, Medline, Google Scholar
4. Lehman AF, Steinwachs DM: Translating research into practice: the Schizophrenia Patient Outcomes Research Team treatment recommendations. Schizophrenia Bulletin 24:1-10, 1998Crossref, Medline, Google Scholar
5. Kern RS, Kuehnel TG, Teuber J, et al: Multimodal cognitive-behavioral therapy for borderline personality disorder with self-injurious behavior. Psychiatric Services 48:1131-1133, 1997Link, Google Scholar
6. Brodie DC, Smith WE: Constructing a conceptual model of drug utilization review. Hospitals 50:143-150, 1976Medline, Google Scholar
7. Sass CM: Drug usage evaluation. Journal of Pharmacy Practice 7:74-78, 1994Crossref, Google Scholar
8. May PRA: Treatment of Schizophrenia. New York, Science House, 1968Google Scholar
9. Corrigan PY, Liberman RP (eds): Behavior Therapy in Psychiatric Hospitals. New York, Springer, 1994Google Scholar



