Clinical Prediction of Assaultive Behavior Among Male Psychiatric Patients at a Maximum-Security Forensic Facility
Abstract
OBJECTIVE: Patient characteristics associated with the clinical prediction of assaultive behavior in a forensic psychiatric hospital were compared with characteristics associated with actual assaultive behavior. METHODS: Treating psychiatrists at a New York forensic psychiatric hospital were asked to predict which of a sample of 183 recently admitted male patients were likely to show assaultive behavior during a three-month period. The predictions were compared with incident reports of actual assaultive behavior. Several patient characteristics, including race, legal status, age, education, criminal history, psychiatric symptoms rated independently by raters other than the treating psychiatrists, and ward behavior, were examined for their association with predicted and actual assaultive behavior. RESULTS: Clinicians' rate of correct prediction of assaultive behavior was 71 percent, with a diagnostic sensitivity of 54 percent and a diagnostic specificity of 79 percent. Characteristics associated with the prediction of assaultive behavior were race, transfer from a civil facility because of violence or dangerousness, age, education, arrests for violent offenses, childhood physical abuse, hostility, temper (or nurses' assessment of the patient's irritability), and inability to follow ward routine. Characteristics associated with actual assaultive behavior were transfer from a civil hospital, dual diagnosis of schizophrenia and substance abuse or dependence, childhood physical abuse, age, thought disorder, and temper. CONCLUSIONS: Clinicians were significantly more accurate than chance in prospectively predicting which male forensic patients would show assaultive behavior. However, some of the factors associated with clinical prediction, such as race, ability to follow ward routine, and arrest history, were not associated with actual assaultive behavior. In addition, clinicians failed to use dual diagnosis of schizophrenia and substance use disorder as a predictor.
Clinicians' prediction of assaultive behavior among psychiatric inpatients has long been studied. Accuracy is low for long-term predictions partly because of low base rates of assaultive behavior and vague criteria for violence, which has led to high false-positive rates (1,2,3,4). Accuracy is somewhat better for short-term predictions (5,6,7). We are not aware of any reports on the clinical prediction of assaultiveness in forensic settings.
As noted by Apperson and colleagues (5), accuracy of clinical prediction is influenced by many factors, including method of prediction, length of the follow-up period, outcome measure, and composition of the comparison groups. In a study of patients admitted to an inpatient setting due to dangerousness to others, they found that rates of violence were higher for patients predicted to be assaultive (75 percent) than for those who were not (12.5 percent). However, they found no difference in rates of violence between patients who were admitted due to dangerousness to others (56 percent) and those who were not (42 percent). In addition, they found that roughly 80 percent of the violent incidents occurred more than 72 hours after admission. This latter finding is important because some studies have limited their period of prediction to the first three days after admission (6).
Other studies of patient populations in civil hospitals (7,8) have used an ordinal risk assessment scale, which was subsequently dichotomized into high and low risk. These studies found that clinicians' risk assessment was more accurate than chance in predicting violence over a one-week period. One of the studies found a sensitivity of 67 percent and a specificity of 69 percent in risk assessments for a sample of 226 patients (8).
Studies in which predictions are made for a period of only a few days after hospital admission limit the assessment of risk to more acutely psychotic patients. The results of these studies may have less relevance for patients in a forensic facility, because they are usually transferred from other structured milieus where they may have received treatment, and thus they may be less acutely psychotic.
The available literature suggests a variety of factors that differentiate patients who are assaultive from those who are not. They include arrest history (4,9), younger age (4), childhood victimization (10), childhood environment (9), ward behavior (11), and comorbidity of substance abuse and schizophrenia (12). Race has been associated with errors in prediction of assaultive behavior, and hostility-suspiciousness has been associated with accurate prediction of assaultive behavior (8).
We examined whether these variables differentiated patients who were predicted to show assaultive behavior from those who were not and whether these variables differentiated patients who actually became assaultive from those who did not. Other variables relevant to forensic populations, such as legal status, also were examined. The study reported here focused on clinical prediction of inpatient assaultiveness over a 12-week follow-up period. Another major aim of the study was to identify variables that were not explicitly used by clinicians in clinical prediction but were nevertheless associated with it.
Methods
Participants
Participants were male psychiatric inpatients at the Kirby Forensic Psychiatric Center, a maximum-security hospital serving the New York City metropolitan area. This report is based on data collected as part of a larger study for which participating patients gave informed written consent.
Patients are admitted to the forensic facility for several reasons. They may have been found unfit to stand trial and are in need of inpatient psychiatric care to restore their competency. They may have been found not guilty by reason of insanity and are considered dangerously mentally ill. They may have been transferred to the secure facility from a civil hospital due to management difficulties such as violent or dangerous behavior.
Procedure
The records of 411 patients admitted from October 1991 to April 1996 were examined. Patients were approached for participation in the study within two weeks of their admission to the hospital. We successfully recruited 224 of these patients, or 54 percent. They included 199 men and 25 women. Participants and nonparticipants did not differ in age, racial distribution, distribution of index offenses, proportion with a chart diagnosis of schizophrenia, or legal status. Because of the limited number of women in our sample, the analyses reported here are based on data for the men.
At the time a patient was recruited into the study, the patient's treating psychiatrist was interviewed using a standardized instrument and asked to indicate the likelihood that the patient would hit or hurt someone within the first three months of his hospital stay. The treating psychiatrists were interviewed after the patient had been in the hospital for two weeks to allow enough time to observe the patient before making a prediction. Prediction data were available for 183 patients, who constituted the final sample. Among the 183 patients included in the study, 155 patients, or 84.7 percent, were at the forensic facility to resolve competency issues; 16 patients, or 8.7 percent, were there for treatment after a verdict of not guilty by reason of insanity; and 12, or 6.6 percent, were there after an emergency transfer from a civil hospital.
Evaluations
Psychiatric diagnoses, including substance abuse and dependence, were made by a research psychiatrist (not the treating psychiatrist) using the Structured Clinical Interview for DSM-III-R (SCID) (13) for 142 patients or chart review for 41 patients. Rates of schizophrenia, substance abuse, and comorbid substance abuse and schizophrenia did not differ depending on whether diagnoses were obtained from the chart or from the SCID.
A research psychiatrist assessed patients' psychiatric symptoms using the Brief Psychiatric Rating Scale (BPRS) (14). This 18-item scale has five subscales: activation, anergia, anxiety-depression, hostility-suspiciousness, and thought disorder (15). We attempted to make this evaluation weekly. Data were averaged across weeks and were prorated for missing information.
Ward behavior was rated by the ward nurses during the 12-week follow-up, independently of the treating psychiatrists's prospective prediction, using the Nurses' Observation Scale for Inpatient Evaluation (NOSIE) (16). Ratings of patients' temper (or irritability), ability to follow ward routine, and social participation on the ward were derived from the NOSIE ratings. The NOSIE was completed weekly, with scores averaged across weeks and prorated for missing data. In addition, data on patients' medication compliance were obtained by systematic review of nursing records.
Patients' criminal history was obtained from official records. The number of arrests for violent offenses, such as murder, rape, assault, and arson, was distinguished from the number of arrests for nonviolent offenses, such as burglary, misdemeanors, and drug-related crimes. Childhood experiences of victimization were measured using the Conflict Tactics Scales (17), a standardized interview that includes questions on whether during childhood the respondent was hit, was left alone, did not have basic necessities met, or had sex against his or her will. Using the same criteria as Widom's group (18,19,20), we scored the Conflict Tactics Scales for very severe violent abuse, such as childhood physical abuse; sex against one's will, such as childhood sexual abuse; and serious neglect. Finally, data on the family rearing environment, including the presence or absence of a parent with intravenous drug abuse, alcohol abuse, or psychiatric hospitalizations, was obtained from a structured interview.
An assault was defined as a violent incident in which the patient was judged to be the attacker. We should note, however, that it is often difficult to determine who initiates a fight between patients (21,22). For each patient, the number and severity of physically violent incidents over the 12-week follow-up period was recorded using a modification of the Scale for Aggressive and Agitated Behaviors (21), an instrument with high interrater reliability (23).
Data analysis
We conducted two sets of analyses, one on the prediction of assaultive behavior and the other on actual assaultive behavior. In both sets, differences on categorical variables, such as race, diagnosis, patient legal status, and childhood victimization rates were tested using the chi square statistic. Group differences on continuous variables, such as age, education, severity of psychiatric symptoms, ward behavior, and number of arrests, were examined using t tests.
Results
Demographic characteristics
The average age of the study participants was 36.4±10.1 years. The sample consisted of 105 African Americans (57.4 percent), 39 Hispanics (21.3 percent), 35 Caucasians (19.1 percent), and four Asians (2.2 percent).
A total of 106 patients, or 58 percent, had a diagnosis of schizophrenia, and 105 patients, or 57 percent, had a diagnosis of substance abuse or dependence. Fifty-seven patients, or 31 percent, had both a diagnosis of schizophrenia and a substance abuse or dependence disorder. Other diagnoses included affective disorders for 30 patients, delusional disorder for 16 patients, paranoid personality disorder for 23 patients, schizoid personality disorder for 12 patients, and antisocial personality disorder for 20 patients.
The study sample differs from other forensic populations described in the literature, which have had lower proportions of minority patients (24,25,26,27) and a lower prevalence of substance use disorders (24,28). In the study sample, the rate of medication compliance was quite high: 104 patients, or 71 percent, took all of their neuroleptic medication during the 12-week study period. (Data on medication compliance were missing for 37 patients.)
Accuracy of clinical prediction
Treating psychiatrists were significantly more accurate than chance in predicting which patients would be assaultive during the first three months of hospitalization (χ2=22.2, df=1, p<.001). The clinicians predicted that 66 patients, or 36 percent, would become assaultive; 60 patients, or 33 percent of the sample—although not necessarily the same individuals identified by the clinicians—actually did become assaultive (see Table 1). The overall rate of correct classification was 71 percent. The diagnostic sensitivity (29), which is the ratio of the number of true positives to the sum of true positives and false positives, was 54 percent. The diagnostic specificity (29), which is the ratio of the number of true negatives to the sum of true negatives and false negatives, was 79 percent.
Factors associated with clinical prediction
For this analysis, we grouped patients according to whether they were or were not predicted to be assaultive. Statistically significant results are shown in Table 2. African Americans were overrepresented and Caucasians were underrepresented in the group predicted to be assaultive. The groups also differed in legal status. Patients transferred from a civil hospital were overrepresented among patients predicted to be assaultive, and patients found not guilty by reason of insanity were underrepresented. A diagnosis of schizophrenia alone, a dual diagnosis of schizophrenia and substance abuse or dependence, and a substance-related diagnosis alone were not related to clinical prediction.
Patients predicted to be assaultive were younger, had lower levels of education, and had higher scores on the BPRS hostility-suspiciousness subscale, compared with those who were not predicted to be assaultive. In interpreting these findings, it is important to note that the BPRS ratings were made by a research psychiatrist, whereas the prediction was made independently by the treating psychiatrist. Patients predicted to be assaultive had more violent arrests and tended to have more nonviolent arrests than patients who were not predicted to be assaultive. Moreover, patients predicted to be assaultive were rated by ward nurses as having higher scores on temper and showing greater difficulty in following ward routine. However, the groups did not differ in social participation on the ward.
Patients predicted to be assaultive had higher rates of self-reported childhood physical abuse compared with those who were not predicted to be assaultive, but they did not report higher rates of childhood sexual abuse or neglect or increased deviance in the family rearing environment. The two groups did not differ in medication compliance or rates of comorbid substance abuse.
Factors associated with assaultive behavior
Statistically significant comparisons between patients who actually becane assaultive and those who did not are shown in Table 3. This table also includes marginally significant findings (p<.10) for variables found to distinguish the two groups. No differences in racial distribution were found between the group who became assaultive and the group who did not. Fifty-five percent of the assaultive patients were African American, compared with 57 percent of the total sample and 67 percent of the patients who were predicted to be assaultive.
Patients who had been transferred from civil hospitals were overrepresented among the assaultive patients, and patients found not guilty by reason of insanity were underrepresented. Patients who became assaultive and those who did not were similar in their number of arrests for violent offenses and for nonviolent offenses. However, there was a weak correlation between the number of assaults and both arrests for violent offenses (r=.21, p<.011) and arrests for nonviolent offenses (r=.22, p<.006).
Patients who were assaultive in the hospital were younger and tended to have less education than patients who did not become assaultive. Furthermore, assaultive patients showed more temper on the ward, but did not differ in social participation or ability to follow ward routine. Assaultive patients also showed higher levels of thought disorder on the BPRS but did not differ from patients who did not become assaultive in scores on the other BPRS subscales, although the difference for hostility-suspiciousness approached significance (p<.08).
The two groups did not differ in the distribution of diagnoses of schizophrenia or substance abuse or dependence, variables related to the family rearing environment, or history of childhood sexual abuse or neglect. However, comorbid substance abuse or dependence was more prevalent among assaultive patients than among patients who did not become assaultive, as was childhood physical abuse.
Discussion
Treating psychiatrists were significantly more accurate than chance in prospectively predicting which patients would become assaultive during the first 12 weeks after hospital admission. Seventy-one percent of the patients were correctly identified. The diagnostic sensitivity (correct prediction of assaultiveness) was 54 percent, and the diagnostic specificity (correct prediction of nonassaultiveness) was 79 percent.
Given the low base rate of physical assaults among psychiatric inpatients, clinicians in previous studies have often had a high rate of false-positive predictions. In those studies, clinicians did not appear to anchor their prediction on the base rate of violence in their population. The treating psychiatrists at the maximum-security forensic hospital where this study was conducted appeared to be more aware of the base rate of assaultive behavior. They predicted that 36 percent of the male patients in this sample would become assaultive during the first three months of hospitalization, whereas 33 percent actually did. This awareness may have accounted for the low rate of false-positive predictions of 16 percent. The rate of false-negative predictions was only 13 percent.
Our results are consistent with other studies in civil settings (6) in showing that clinical prediction of assaultiveness is more accurate than chance. This study extends this finding to the forensic setting.
A strength of the study was that it addressed many concerns raised by previous work (5). For example, the study based prediction of assaultive behavior on the treating psychiatrist's judgment rather than on patients' admission status. In addition, the follow-up period was longer than that in many of the studies that were conducted in civil hospitals. The study had clear outcome measures and clearly identified comparison groups. We were able to compare factors related to prediction of assaultive behavior as well as to actual assaultive behavior.
The patients who actually became assaultive were younger, tended to be less educated, and were more likely to be transferred from a civil hospital. However, they did not differ from the group of patients who did not become assaultive in racial distribution, ability to follow ward routine, or criminal history.
Predictions may have been influenced by patients' arrest histories, given clinicians' knowledge of that history. Arrest history has been shown in other studies to be the best predictor of violent behavior (9). In the study reported here, the failure of arrest history to differentiate those who were actually assaultive from those who were not was not surprising, given that the sample varied little in arrest history—92 percent of subjects had at least one arrest for a violent offense. However, the number of arrests was correlated with the number of inpatient assaults.
The reason for the impact of race on the prediction was less clear, although a similar finding had been obtained in the assessment of risk of violence among civil psychiatric patients (8). The influence of patients' level of hostility, rated independently of the clinician, might be understandable. However, the difference in hostility between assaultive patients and those who did not become assaultive only approached statistical significance.
In an earlier paper, we described an association between inpatient violence and a poor childhood rearing environment (9). In the study reported here, we failed to see such an association, which was likely due to the low variability in family environment in this sample.
Conclusions
The accuracy of treating psychiatrists was well above chance in predicting which patients would be assaultive, and the correct prediction rate was consistent with other studies in the literature. However, there is clearly room for improvement in such predictions. We found some discrepancies between the variables associated with prediction and those associated with actual assaultive behavior. These discrepancies may be useful teaching points for clinicians. For instance, despite consistent evidence to the contrary (4,8), clinicians overpredicted assaultive behavior for psychiatric patients who were members of racial minorities.
In addition, in forensic psychiatric facilities, arrest history does not predict assaultive behavior, perhaps because an arrest history is so prevalent in this population. However, in civil hospital settings where rates of criminal offenses are lower, it is a useful predictor. Inability to follow ward routine differentiated patients predicted to be assaultive from those who were not. This variable did not, however, differentiate patients who actually became assaultive from those who did not. Thus the ability of patients to follow ward routine may not be a particularly useful predictor of assaultive behavior in a forensic setting.
Finally, clinicians did not appear to take into account the role of a dual diagnosis of schizophrenia and substance abuse or dependence in making their predictions. Nonetheless, rates of assaultive behavior were higher among patients with a dual diagnosis, compared with patients who did not have a dual diagnosis. This latter finding is consistent with the existing literature (12,30). It should be noted that patients did not have access to alcohol or drugs in the hospital. The association between dual diagnosis and assaultiveness in the hospital is likely to be mediated by another variable such as impulsivity.
The study findings suggest that some variables associated with clinical prediction may be misleading in identifying patients who actually become assaultive. If clinical methods of prediction are to be used in the process of assessing risk for violence among forensic patients, they should be supplemented with other data specific to them, such as data on thought disorder, history of comorbidity of schizophrenia and substance use disorder, and history of childhood victimization, much as predictions of violence among civil psychiatric patients have been supplemented (31).
Acknowledgments
This work was supported by grant MH-45060 from the National Institute of Mental Health to Dr. Convit.
Dr. Hoptman, Dr. Yates, Dr. Patalinjug, and Dr. Convit are affiliated with the Nathan Kline Institute for Psychiatric Research in Orangeburg, New York, and the department of psychiatry at New York University School of Medicine in New York City. Dr. Wack is with the Kirby Forensic Psychiatric Center in Wards Island, New York, and with the department of psychiatry at New York University School of Medicine. Address correspondence to Dr. Convit at Millhauser Laboratories, HN-314, New York University School of Medicine, 550 First Avenue, New York, New York 10016 (e-mail, [email protected]).
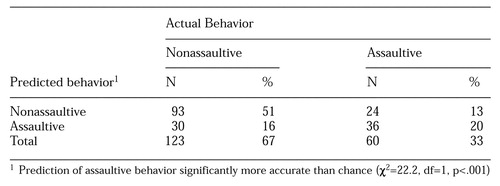 |
Table 1. Accuracy of clinicians'prediction of assaultive behaviour among 183 male patients within three months of admission to a forensic psychiatric hospital
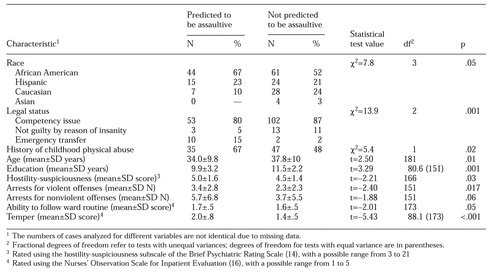 |
Table 2. Characteristics of patients whom clinicians predicted would be assaultive within three months of admission to a forensic psychiatric hospital and of those predicted not to be assaultive
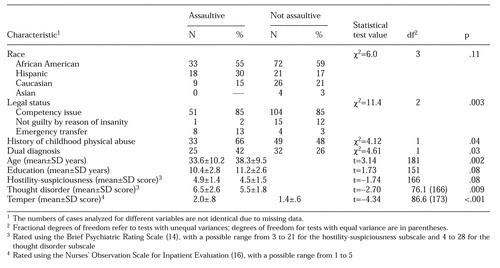 |
Table 3. Characteristics of patients who were and were not assaultive within three months of admission to a forensic psychiatric hospital
1. Cocozza J, Steadman H: The failure of psychiatric predictions of dangerousness: clear and convincing evidence. Rutgers Law Review 29:1074-1101, 1976Google Scholar
2. Kozol HL, Boucher RJ, Garofalo RF: The diagnosis and treatment of dangerousness. Crime and Delinquency 18:371-372, 1972Crossref, Google Scholar
3. Convit A, Jaeger J, Lin SP, et al: Prediction of violence in psychiatric inpatients, in Biologic Contributions to Crime Causation. Edited by Moffitt TE, Mednick SA. Boston, Nijhoff, 1988Google Scholar
4. Monahan J: Predicting Violent Behavior: An Assessment of Clinical Techniques. Beverly Hills, Calif, Sage, 1981Google Scholar
5. Apperson LJ, Mulvey EP, Lidz CW: Short-term clinical prediction of assaultive behavior: artifacts of research methods. American Journal of Psychiatry 150:1374-1379, 1993Link, Google Scholar
6. McNeil DE, Binder RL: Predictive validity of judgments of dangerousness in emergency civil commitment. American Journal of Psychiatry 144:197-200, 1987Link, Google Scholar
7. McNeil DE, Binder RL: Clinical assessment of the risk of violence among psychiatric inpatients. American Journal of Psychiatry 148:1317-1321, 1991Link, Google Scholar
8. McNeil DE, Binder RL: Correlates of accuracy in the assessment of psychiatric inpatients' risk of violence. American Journal of Psychiatry 152:901-906, 1995Link, Google Scholar
9. Convit A, Jaeger J, Lin SP, et al: Predicting assaultiveness in psychiatric inpatients: a pilot study. Hospital and Community Psychiatry 39:429-434, 1988Abstract, Google Scholar
10. Widom C: The cycle of violence. Science 244:160-166, 1989Crossref, Medline, Google Scholar
11. Krakowski M, Czobor P: Violence in psychiatric patients: the role of psychosis, frontal lobe impairment, and ward treatment. Comprehensive Psychiatry 38:230-236, 1997Crossref, Medline, Google Scholar
12. Steadman HJ, Mulvey EP, Monahan J, et al: Violence by people discharged from acute psychiatric inpatient facilities and by others in the same neighborhoods. Archives of General Psychiatry 55:393-401, 1998Crossref, Medline, Google Scholar
13. Spitzer RL, Williams JBW, Gibbon M, et al: Structured Clinical Interview for DSM-III-R, Patient Edition (SCID-P, Version 1.0). Washington, DC, American Psychiatric Press, 1990Google Scholar
14. Overall JE, Gorham DR: The Brief Psychiatric Rating Scale. Psychological Reports 10:799-812, 1962Crossref, Google Scholar
15. Guy W: ECDEU Assessment Manual for Psychopharmacology. Rockville, Md, National Institute of Mental Health, 1976Google Scholar
16. Honigfield G, Klett CJ: The Nurses' Observation Scale for Inpatient Evaluation: a new scale for measuring improvement in chronic schizophrenia. Journal of Clinical Psychology 21:65-71, 1965Crossref, Medline, Google Scholar
17. Straus MA: Measuring intrafamily conflict and violence: the Conflict Tactics (CT) Scales. Journal of Marriage and the Family 41:75-86, 1979Crossref, Google Scholar
18. Widom CS, Morris S: Accuracy of adult recollections of childhood victimization: II. childhood sexual abuse. Psychological Assessment 9:34-46, 1997Crossref, Google Scholar
19. Widom CS, Shepard RL: Accuracy of adult recollections of childhood victimization: I. childhood physical abuse. Psychological Assessment 8:412-421, 1996Crossref, Google Scholar
20. Widom CS: Crime and childhood sexual abuse. Society 33:47-53, 1996Crossref, Google Scholar
21. Brizer D, Convit A, Krakowski M, et al: Reporting violence: a comparison of routine ward reports with a new rating scale. Hospital and Community Psychiatry 38:769-770, 1987Abstract, Google Scholar
22. Yudofsky SC, Silver JM, Jackson W: The Overt Aggression Scale for the objective rating of verbal and physical aggression. American Journal of Psychiatry 143:35-39, 1986Link, Google Scholar
23. Convit A, Isay D, Gadioma R, et al: Underreporting of physical assaults in schizophrenic inpatients. Journal of Nervous and Mental Disease 176:507-509, 1988Crossref, Medline, Google Scholar
24. Carmel H, Hunter M: Staff injuries from inpatient violence. Hospital and Community Psychiatry 40:41-46, 1989Abstract, Google Scholar
25. Hutton HE, Miner MH, Langfeldt VC: The utility of the Magargee-Bohn typology in a forensic psychiatric hospital. Journal of Personality Assessment 60:572-587, 1993Crossref, Medline, Google Scholar
26. Klinge V, Dorsey J: Correlates of the Woodcock-Johnson Reading Comprehension Test and Kaufman Brief Intelligence Test in a forensic psychiatric population. Journal of Clinical Psychology 49:593-598, 1993Crossref, Medline, Google Scholar
27. Hill CD, Rogers R, Bickford ME: Predicting aggressive and socially disruptive behavior in a maximum-security forensic psychiatric hospital. Journal of Forensic Sciences 41:56-59, 1996Medline, Google Scholar
28. Rice ME, Harris GT: Violent recidivism: assessing predictive validity. Journal of Consulting and Clinical Psychology 63:737-748, 1995Crossref, Medline, Google Scholar
29. Feinstein AR: Clinical epidemiology, in The Architecture of Clinical Research. Edited by Feinstein AR. Philadelphia, Saunders, 1985Google Scholar
30. Swanson J, Holzer C III, Ganju V, et al: Violence and psychiatric disorder in the community: evidence from the Epidemiologic Catchment Area survey. Hospital and Community Psychiatry 41:761-770, 1990Abstract, Google Scholar
31. Gardner W, Lidz CW, Mulvey EP, et al: Clinical versus actuarial predictions of violence of patients with mental illnesses. Journal of Consulting and Clinical Psychology 64:602-609, 1996Crossref, Medline, Google Scholar



