Anxiety Disorders Among Abstinent Alcohol-Dependent Patients
Abstract
The Spielberger State-Trait Anxiety Index (STAI) and screening questions for anxiety disorders from the Structured Clinical Interview for DSM-IV Disorders were used to assess 146 alcohol-dependent patients on admission for inpatient treatment and just before discharge, after about three to four weeks of abstinence. Eighty-four patients (58 percent) reported excessive anxiety on admission, and 32 patients (22 percent) met DSM-IV criteria for specific anxiety disorders. After three to four weeks of abstinence, both state and trait STAI scores declined significantly, and only 15 patients (10 percent) met criteria for specific anxiety disorders. Anxiety levels on admission were significantly related to severity of alcohol dependence and recent life events but not to severity of withdrawal symptoms.
Anxiety is common among patients with alcohol dependence (1). Between 22 percent and 69 percent of alcohol-dependent patients have comorbid anxiety disorders (2,3). Although anxiety disorders may be a pre-existing condition in some cases, factors related to alcohol use, such as increased stressful life events and alcohol withdrawal symptoms, could also contribute to patients' reports of anxiety.
Patients for whom anxiety disorders play a causative role in alcoholism must be differentiated from those for whom the anxiety is secondary to alcohol abuse. The former are likely to benefit from treatment of the anxiety disorder in addition to detoxification and rehabilitation.
The high rates of anxiety found among patients with alcohol dependence may be inflated because many studies are performed shortly after abstinence is achieved, when anxiety may be related to intoxication or withdrawal (4). Also, interpretation of the results is complicated by other methodological problems, including the use of different diagnostic criteria, inaccuracies in using symptom checklists, unreliable reporting of relationships between alcohol use and anxiety symptoms, effects of abuse of other substances, alcohol-related severe life problems, and small sample sizes. Nevertheless, anxiety disorders appear to be more common than expected by chance alone. In particular, patients with alcohol dependence report higher-than-normal rates of panic disorder, social phobia, and perhaps generalized anxiety disorder (4).
This study attempted to address some of the methodological problems of previous work and aimed at determining the prevalence of anxiety disorders in a sample of alcohol-dependent patients on admission to inpatient treatment and after a period of abstinence. Other objectives were to examine the relationships between anxiety symptoms and the severity of alcohol dependence and stressful life events and to investigate changes in anxiety scores between admission and the third or fourth week of abstinence.
Methods
Patients in the study were consecutive admissions over ten months (July 31, 1995, to May 27, 1996) to the alcohol rehabilitation unit at Stikland Hospital in Cape Town, South Africa. Patients included in the study were voluntarily admitted to the hospital and were free of major physical illnesses. They met DSM-IV criteria for alcohol dependence (5) and showed no overt cognitive impairment. Patients with more than nine years of education underwent a four-week rehabilitation program, while the rest underwent a three-week program. All subjects provided written informed consent. The study was approved by the ethics committee of the University of Stellenbosch.
Early in their hospital admission, subjects were given a comprehensive clinical assessment by the first author, including a semistructured interview, the first seven screening questions for anxiety disorder from the Structured Clinical Interview for DSM-IV Disorders (SCID) (6), and the Withdrawal Syndrome Scale (7). The four-week group also completed the Severity of Alcohol Dependence Questionnaire (SADQ) (8). All subjects completed the Spielberger State-Trait Anxiety Index (STAI) (9), Holmes and Rahe's life event scale, and the Social Readjustment rating Scale (SRRS) (10).
The STAI comprises two separate scales for measuring state and trait anxiety. Scores on the STAI range from 20 to 80, with higher scores representing higher levels of anxiety. The STAI scales were administered again during week 4 to 33 men and 14 women.
Because the three-week patients were discharged on day 19 after admission, they were excluded from the repeat analyses. For repeat analyses, raw scores were used, and for all other analyses, percentile ranks were used to standardize scores for age and gender. A particular percentile rank represents the percentage of the population expected to have a score equal to or less than the percentile rank. In describing the proportion of subjects with very high levels of anxiety, a cutoff of 95 was arbitrarily chosen.
Patients who responded positively to the screening tests for an anxiety disorder were further examined and diagnosed based on DSM-IV criteria. A final diagnosis was made by the ward physician after they had been observed on the unit during their stay.
Prevalence rates and 95 percent confidence intervals for the prevalence rates of anxiety disorders were computed. Because of skewed data, nonparametric tests were used. The significance of differences between scores at admission and discharge was determined using the Wilcoxon signed-rank test. The Spearman rank-order correlation coefficient was used for correlations between numeric variables. For categorical variables, a Yates'-corrected chi square test with one degree of freedom was performed. The McNemar chi test for matched pairs was performed for dependent categories.
Results
During the ten months, 164 patients were admitted. Eighteen patients were excluded from the study—three were readmissions, six were discharged within the first few days, and nine had prominent cognitive impairment. Another 20 did not complete the program but were included because they remained in the ward long enough for a diagnosis to be made. Thus the final sample comprised 146 patients. Of these, 119 (82 percent) were men, 62 (42 percent) were married, and 70 (48 percent) were employed. Twenty-five (17 percent) sporadically abused other substances. The three-week group comprised 67 men and 12 women, and the four-week group comprised 52 men and 15 women.
The mean±SD age of the patients was 38.5±8.49 years. The mean±SD age when patients reported that they first drank was 17.4±4.21 years. The mean±SD duration of excessive drinking was 9.2±7.07 years. The median time of last alcohol intake before admission was 21 hours.
Thirteen patients were receiving antidepressant or anxiolytic medication on admission, but none of these patients were diagnosed at admission as having an anxiety disorder. In six cases the medication was discontinued. No significant differences between patients in the three- and four-week programs were found in age, age of onset of alcohol abuse, duration of alcohol abuse, anxiety scores, withdrawal symptoms, and significant life events.
On admission, the STAI state scale was administered to 100 patients and the trait scale to 98 patients. The scores revealed that 42 percent and 52 percent, respectively, had percentile rank scores greater than 95 on admission. The mean±SD STAI state and trait scores were 52.9±13.58 and 53.5±12.13, respectively.
Correlations were performed between STAI state and trait scores and SADQ total score; scores on the SADQ physical, affective, relief, and consumption subsections; WSS score; and SRRS score. STAI state scores were significantly correlated with total scores on the SADQ (r=.48, p<.001), as well as with scores on several of its subsections, including physical (r=.35, p<.01), affective (r=.54, p<.001), and relief (r=.38, p<.005). The STAI trait score was correlated with total score on the SADQ (r=0.43, p<.005), as well as with the score on its affective subsection (r=.59, p<.001), and with SRRS score (r=.40, p<.005).
Based on results of the SCID screening on admission, 84 patients (58 percent) reported excessive anxiety, 26 (18 percent) reported panic symptoms, 29 (20 percent) reported symptoms of agoraphobia, 44 (31 percent) reported social anxiety, 42 (29 percent) reported a specific phobia, six (4 percent) reported obsessions, and 12 (8 percent) reported compulsions. Table 1 shows specific DSM-IV diagnoses of anxiety disorders among the 146 patients in the study at admission and before discharge, about three to four weeks later. A significant decline was noted in the proportion of subjects diagnosed as having an anxiety disorder (χ2=8.47, df=1, p<.005). The STAI was readministered to 41 patients before discharge; scores declined significantly (state, Z=4.78; trait, Z=3.98; p<.001). The proportion with percentile rank scores greater than 95 for the STAI state and trait scales declined to 11 percent and 21 percent, respectively.
Because anxiety disorders may be more common in females with alcohol dependence than in males with the disorder, we analyzed results for men and women patients separately. The prevalence of anxiety disorder diagnoses on admission or discharge did not differ significantly by gender. Furthermore, no significant gender differences were found on admission on scores on the Withdrawal Syndrome Scale, the SSRS, and the STAI state and trait scales. At four weeks, women showed significantly higher percentile rank values than men on the STAI state scale (Z=2.09, p=.03) and trait scale (Z=2.72, p=.006).
Discussion and conclusions
As in the study by Brown and associates (1), our results indicate that for most patients with alcohol dependence, anxiety symptoms are temporary and are related to intoxication and withdrawal. However, symptoms may be more persistent among females. Our results further suggest that factors other than withdrawal may contribute to anxiety symptoms. Anxiety scores on admission showed significant correlations with severity of alcohol dependence and significant life events but not with severity of alcohol withdrawal symptoms.
Symptoms resolved for most patients meeting DSM-IV criteria for specific anxiety disorders at admission, supporting the view that previous estimates of these disorders may be inflated (4). Even STAI trait anxiety scores declined significantly after three to four weeks, as was also the case in the study by Brown and colleagues (1). Clearly, diagnostic schedules and symptom rating scales for assessing anxiety during the acute abstinence phase need to be used with caution.
Several limiting factors in this study should be noted. Some patients with comorbid anxiety disorders may have been referred to psychiatric facilities other than the alcohol rehabilitation unit. Patients with avoidant behavior may not have sought admission. The high anxiety scores on admission could be due partly to patients' removal from familiar surroundings. Finally, a reduction in stressful events during hospitalization could have influenced the results.
In conclusion, the diagnosis of anxiety disorders among alcohol-dependent individuals should be delayed for at least a few weeks after abstinence. Treatment interventions for anxiety disorders should be reserved for patients with persistent symptoms, as they may be at particular risk for relapse (1).
Acknowledgment
This work was supported by the unit for anxiety and stress disorders of the Medical Research Council of South Africa.
The authors are affiliated with the department of psychiatry at the University of Stellenbosch in Cape Province, South Africa. Dr. Roberts is research medical officer, Dr. Emsley is head of the department, Dr. Pienaar is principal psychiatrist, and Dr. Stein is director of research. Send correspondence to Dr. Emsley at P.O. Box 19063, Tygerberg 7505, South Africa (e-mail, [email protected]).
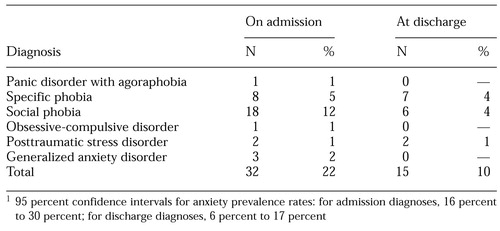 |
Table 1. DSM-IV diagnoses of anxiety disorders among 146 patients with alcohol dependence on admission to an impatient alcohol rehabilitation unit and before discharge three or four weeks later1
1. Brown SA, Irwin M, Schuckit MA: Changes in anxiety among abstinent male alcoholics. Journal of Studies on Alcohol 52:55-61, 1991Crossref, Medline, Google Scholar
2. Weiss KJ, Rosenberg DJ: Prevalence of anxiety disorder among alcoholics. Journal of Clinical Psychiatry 46:3-5, 1985Medline, Google Scholar
3. Mullaney JA, Trippett CJ: Alcohol dependence and phobias: clinical description and relevance. British Journal of Psychiatry 135:565-573, 1994Crossref, Google Scholar
4. Schuckit MA, Hesselbrock VH: Alcohol dependence and anxiety disorders: what is the relationship? American Journal of Psychiatry 151:1723-1733, 1994Google Scholar
5. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC, American Psychiatric Association, 1994.Google Scholar
6. First MB, Spitzer RL, Gibbon M, et al: Structured Clinical Interview for DSM-IV Disorders. New York, New York State Psychiatric Institute, Biometrics Research Department, 1994Google Scholar
7. Bech P, Rasmussen S, Dahl A, et al: The Withdrawal Syndrome Scale for alcohol and related psychoactive drugs. Nordic Journal of Psychiatry 43:291-294, 1989Crossref, Google Scholar
8. Stockwell T, Murphy D, Hodgson R: The Severity of Alcohol Dependence Questionnaire: its use and reliability. British Journal of Addiction 78:145-155, 1983Crossref, Medline, Google Scholar
9. Spielberger CD: Manual for the State-Trait Anxiety Inventory (STAI). Palo Alto, Calif, Consulting Psychologists Press, 1983Google Scholar
10. Holmes TH, Rahe RH: The Social Readjustment Rating Scale. Journal of Psychosomatic Research 11:213-218, 1971Crossref, Google Scholar



