Compliance With Depot Antipsychotic Medication by Patients Attending Outpatient Clinics
Abstract
Outpatients with schizophrenia often have problems complying with a regimen of oral antipsychotic medications. Use of depot medications improves compliance, but patients' geographic location and access to transportation may affect compliance with a depot regimen. The authors used retrospective chart review to examine whether patients' geographic location and sociodemographic characteristics and characteristics of their medication use were related to compliance with a depot regimen. The subjects were 75 patients attending an urban clinic and 23 patients attending a rural clinic in New York State. Median rates of compliance were 94.7 percent for the urban patients and 96.4 percent for the rural patients, not a significant difference. The only characteristic associated with a decreased compliance rate was a history of substance abuse.
Antipsychotic medications prescribed to patients with chronic schizophrenia have been shown to reduce relapse rates and rehospitalizations, but these outcomes rely on patients' adherence to medication regimens (1). Long-acting depot antipsychotic medications were developed in the 1960s in an attempt to avoid compliance problems associated with chronic oral therapy. Recent reports have suggested that depot antipsychotic medications are a cost-effective alternative to oral therapy due to the reduction in relapse rates associated with depot regimens (2,3).
Compliance is a clear determinant of the efficacy of depot antipsychotic medications. Patients who receive long-acting decanoate agents are required to come to an outpatient site for administration of their medication. In a study of compliance with psychiatric aftercare, Carrion and associates (4) found that 71 to 86 percent of outpatients kept clinic appointments each month over a 12-month period. Although that study examined psychiatric aftercare in general rather than depot injections specifically, patients' geographic location and access to transportation were found to decrease compliance. The effects on compliance of sociodemographic characteristics such as gender, age, socioeconomic status, length of treatment, marital status, living arrangements, and race remain controversial (5).
Our study was designed to assess compliance rates with depot antipsychotic medications among psychiatric outpatients in state-operated programs in upstate New York. We hypothesized that compliance rates with depot antipsychotic medication in the study population would be greater than those reported in the literature for oral agents. We also hypothesized that lack of access to transportation would decrease compliance. Last, we attempted to determine whether sociodemographic variables were related to compliance.
Methods
We retrospectively reviewed the records of patients who attended the Albany County Outpatient Clinic and Greene County Mental Health Center in New York State for administration of haloperidol decanoate or fluphenazine decanoate during the period from September 1, 1993, to August 30, 1994. Informed consent was not required because the study did not include direct patient assessment or contact. However, the project was approved by the investigational review board of the Capital District Psychiatric Center, which maintains the records for both study sites.
The sample included two groups of patients, one group treated in an urban location and the other in a rural location. The urban setting, Albany County Outpatient Clinic, is located within the Capital District Psychiatric Center, a state psychiatric facility in the city of Albany. Patients receive depot antipsychotic medications at the decanoate clinic, which is held every Wednesday. Patients are encouraged to keep their appointments, but if an appointment is not kept, the medication may be given on a nonclinic day. Patients who consistently miss appointments may be required to have a 24-hour inpatient observation period before receiving their dose.
The rural setting, Greene County Mental Health Center, is a county-run facility located in the Catskill Mountains approximately 25 miles from Albany. Group sessions for administration of decanoate medications are held weekly at a local firehouse; doses are administered by a nurse. If a dose is missed, the patient is contacted by phone or in writing. Patients who miss the group session may come to the mental health center on another day to receive their dose. If the patient is unable to attend the group sessions or come to the mental health center, a nurse may visit the patient for dose administration.
The sample of patient records was obtained from pharmacy records at the Capital District Psychiatric Center. The records of all patients for whom doses of haloperidol decanoate or fluphenazine decanoate were dispensed during the month of August 1993 were included in the sample. All information on patients' demographic characteristics and compliance was obtained from the charts.
Data on the following demographic variables were collected and analyzed for their relationship to compliance: urban or rural residence, gender, age, race, marital status, living arrangement, whether the patient had a case manager, type of transportation used by the patient, employment status, education, and history of substance abuse. If a patient's characteristics changed over the study period, the characteristic that was present for the majority of time during the study period was used in the analysis. Data on diagnosis were not collected; it was understood that all patients receiving the depot medications considered in the study had a diagnosis of schizophrenia or schizoaffective disorder.
Compliance with depot medications was determined retrospectively for the 12-month period from September 1, 1993, through August 31, 1994. Compliance was calculated by dividing the number of kept appointments for dose administration by the number of scheduled appointments. A kept appointment was defined as receipt of a dose within four days of the scheduled dose. Failure to keep a dose appointment was not considered such if the medication was discontinued by the physician, if the patient was hospitalized, or if the patient had relocated and had been reestablished at another clinic.
Patients were assigned to the rural or urban group based on address and zip code. Patients residing within the Albany city limits were assigned to the urban group, and those residing outside the city were assigned to the rural group. Because all patients in the sample were outpatients and could obtain medication from sources outside the study facilities, information on medications other than antipsychotics was not collected.
Data were statistically analyzed using the computer program Sigmastat (Jandel Scientific). Compliance is reported as a median proportion with 25 to 75 percent quartile ranges. The proportions of kept dose appointments to scheduled appointments for the urban and rural groups were compared using a Mann-Whitney ranked-sum test. The two groups' demographic characteristics were compared using Student's t test for continuous data and the chi square test for dichotomous data. To determine if any characteristic was related to improved compliance, mean proportions between categories for each characteristic were compared using the Mann-Whitney ranked-sum test. For characteristics with continuous data, Pearson product-moment correlation was used. Significance was determined at p<.05.
Results
A total of 104 outpatients received either depot fluphenazine or depot haloperidol during the month of August 1993. Six patients were excluded from the sample because their charts could not be obtained or because their depot medication had been discontinued during the study period, leaving a final sample of 98 patients (11 at the Greene County site and 87 at the Albany County site). All patients attending the Greene County clinic plus 12 patients attending the Albany County clinic constituted the rural group, 23 patients. Seventy-five patients, all attending the Albany County clinic, constituted the urban group. There were no differences in demographic variables between the two groups.
The overall proportion of kept appointments to scheduled appointments was .96. The urban and rural groups did not differ in the proportion of kept dose appointments.
Table 1 shows the patients' clinical characteristics. In the total patient sample, more patients were receiving fluphenazine decanoate than haloperidol decanoate (87 percent versus 13 percent). Dose requirements varied widely and were converted to daily oral chlorpromazine equivalents. The doses ranged from 80 to 2,850 chlorpromazine equivalents a day, with a mean of 676 chlorpromazine equivalents a day. The patients' duration of illness ranged from three to 35 years, with a mean of 18.7 years. The mean duration of depot therapy was six years, with a range from less than one to 23 years.
The only patient characteristics that were associated with compliance were history of substance abuse and duration of illness. Patients with a history of substance abuse had poorer compliance (p=.027). Longer duration of illness was correlated with improved compliance (r=.24, p<.02).
Discussion and conclusions
The primary objective of this study was to determine the rate of compliance with depot antipsychotic medication in an outpatient population of patients with schizophrenia or schizoaffective disorder and to determine which factors were related to compliance. This study found an overall compliance rate of 96 percent, which is well above rates reported for newer oral antipsychotic agents (6). Because depot antipsychotic medications have to be administered by a health care provider, a more effective determination of compliance is possible. If a patient misses an appointment, follow-up by a health care provider can bring the patient back into treatment before a relapse occurs.
The compliance rate found in this study is also higher than that reported in previous studies with depot antipsychotic medications (4,7). This difference may be attributed to the relationship that exists between patients and health care workers at the sites of this study. For example, follow-up on missed appointments was very thorough at both sites. Attempts were made to contact patients by telephone or by mail. If these attempts were unsuccessful, a worker went to the patient's residence. In the long run, providing this follow-up care may be cost-effective if it helps the patient avoid a relapse resulting from noncompliance.
Our definition of compliance may not have been as restrictive as that found in previous studies. It is difficult to impose a strict definition of compliance in a study of depot agents, because the outcome of missing a depot dose by one day may not be comparable to that of missing an oral dose for a day. We believe that the definition we used—the proportion of scheduled depot dose appointments that were kept within four days—was practical for this type of study.
In agreement with previous literature, our study did not identify many characteristics that could predict improved compliance (5,8). Although we did not find that access to public transportation had any association with compliance, our method of data collection may not have adequately addressed this issue. Many charts stated that public transportation was accessible to the patient but did not state whether patients in fact used public transportation. More accurate information could have been obtained if patients had been asked directly.
Substance abuse was associated with reduced compliance in this study and in previous studies (9,10). Patients' substance abuse may need to be adequately addressed before successful treatment of schizophrenia can be accomplished. Although longer duration of illness was positively correlated with compliance, the clinical significance of this association is questionable.
Patients receiving depot antipsychotic medications appear to have improved compliance compared with patients receiving oral therapy. The excellent compliance rates found in this study may strengthen the conclusions reported in studies of the cost-effectiveness of depot antipsychotics (2). These findings should provide additional support for a regimen that is clearly underused in this country. It is unclear if any patient characteristics, other than substance abuse, can predict compliance with a depot regimen. Therefore, substance abuse by patients should be actively addressed before initiating long-term treatment with antipsychotic medications.
Dr. Heyscue is assistant professor of clinical pharmacy at Massachusetts College of Pharmacy and Allied Health Sciences in Boston. Dr. Levin is associate professor of pharmacy at Albany College of Pharmacy. He is also medical staff associate at Capital District Psychiatric Center in Albany, where Dr. Merrick is director of pharmacy. Address correspondence to Dr. Levin at the Albany College of Pharmacy, 106 New Scotland Avenue, Albany, New York 11208 (e-mail, [email protected]). An earlier version of this paper was presented as a poster at the annual meeting of the American College of Clinical Pharmacy held August 4-7, 1996, in Nashville and at the midyear clinical meeting of the American Society of Health Systems held December 3-7, 1996, in New Orleans.
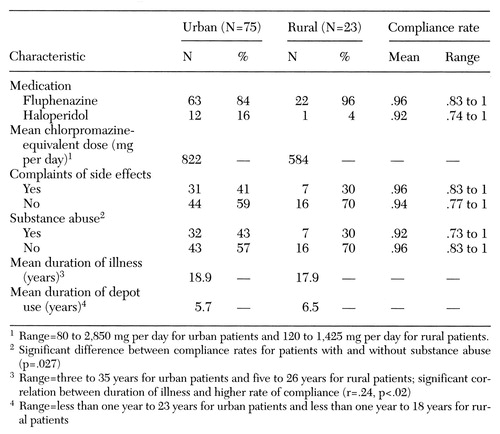 |
Table 1. Clinical characteristics and mean rates of compliance with appointments for administration of depot antipsychotic medications among 98 outpatients with schizophrenia at an urban and a rural treatment site
1. Bartko G, Maylath E, Herczeg L: Comparative study of schizophrenic patients relapsed on and off medication. Psychiatry Research 22:221-227, 1987Crossref, Medline, Google Scholar
2. Glazer W, Ereshefsky L: A pharmacoeconomic model of outpatient antipsychotic therapy in "revolving door" schizophrenic patients. Journal of Clinical Psychiatry 57:337-345, 1996Medline, Google Scholar
3. Weiden P, Olfson M: Cost of relapse in schizophrenia. Schizophrenia Bulletin 21:419-429, 1995Crossref, Medline, Google Scholar
4. Carrion P, Swann A, Kellert-Cecil H, et al: Compliance with clinic attendance by outpatients with schizophrenia. Hospital and Community Psychiatry 44:764-767, 1993Abstract, Google Scholar
5. Pan PC, Tantam D: Clinical characteristics, health beliefs, and compliance with maintenance treatment: a comparison between regular and irregular attenders at a depot clinic. Acta Psychiatrica Scandinavica 79:564-570, 1989Crossref, Medline, Google Scholar
6. Hirsch SR, Puri BK: Clozapine progress in treating refractory schizophrenia. British Medical Journal 306:1427-1428, 1993Crossref, Medline, Google Scholar
7. Tunnicliffe S, Harrison G, Standen PJ: Factors affecting compliance with depot injection treatment in the community. Social Psychiatry and Psychiatric Epidemiology 27:230-233, 1992Crossref, Medline, Google Scholar
8. Buchanan A: A two-year prospective study of treatment compliance in patients with schizophrenia. Psychological Medicine 22:787-797, 1992Crossref, Medline, Google Scholar
9. Kent S, Yellowlees P: Psychiatric and social reasons for frequent rehospitalization. Hospital and Community Psychiatry 45:347-350, 1994Abstract, Google Scholar
10. DeQuardo JR, Carpenter CP, Tandon R: Patterns of substance abuse in schizophrenia: nature and significance. Journal of Psychiatric Research 20:267-275, 1994Crossref, Google Scholar



