Factors Associated With Involuntary Return to a Psychiatric Emergency Service Within 12 Months
Abstract
OBJECTIVE: This study examined patient characteristics and other factors that contributed to the involuntary return of patients to a psychiatric emergency service within 12 months of an initial evaluation in the service. The findings were used to consider whether the pressure to limit duration of hospital stays under managed care contributed to the patients' return to the emergency service. METHODS: Structured observations of evaluations of 417 patients admitted to the psychiatric emergency service were completed at seven county general hospitals in California. Twelve months after the initial evaluation, mental health and criminal justice records were reviewed for evidence of the patients' return for emergency psychiatric evaluation at any of the seven hospitals. Factors associated with patients' return to the psychiatric emergency service were evaluated using multivariate modeling. RESULTS: Of the 417 patients initially evaluated, 121, or 29 percent, were involuntarily returned to the psychiatric emergency service within 12 months. The likelihood of involuntary return was increased by a psychotic diagnosis and indications of dangerousness at the initial evaluation. Having insurance also increased the likelihood of involuntary return. CONCLUSIONS: The patient's initial condition in the psychiatric emergency service was found to be the best predictor of involuntary return. Brief hospitalization—an average of six days—after the evaluation did not have a significant prophylactic effect, perhaps because the reduced length of inpatient stay in the managed care environment did not allow adequate resolution of the patient's clinical condition.
In the provision of mental health services, the funds that allow managed care organizations the savings to develop a flexible and responsive service system are primarily accrued from limits on the use of more costly services such as inpatient psychiatric care (1,2,3). Critical decisions about the necessity of psychiatric hospitalization are often made in the psychiatric emergency service in general hospitals, where most civil commitment evaluations are completed. Thus this treatment setting is a critical entry point into the mental health system.
Open 24 hours a day, the psychiatric emergency service is readily available to serve the most needy patients. As many as one-third of the patients admitted to a psychiatric emergency service are likely to return within the year. This proportion represents an increase from about 10 percent in the early 1970s and approximates the percentage of repeat users noted in the mid-1980s (4,5,6,7,8,9,10,11,12,13,14,15,16,17,18). If the use of inpatient psychiatric care is to be restricted under the auspices of managed care, it is crucial to better understand how specific factors associated with the patient's experience at the initial evaluation in the psychiatric emergency service and with interventions after the emergency visit may predict future involuntary returns to the emergency service. This study examined patient characteristics and other factors associated with the involuntary return of patients to a psychiatric emergency service within 12 months of an initial evaluation in the service.
Researchers have begun to identify some of the characteristics of repeat users of the psychiatric emergency service. Demographic findings suggest that frequent users are more likely to be male (5,6,7,8), unmarried (6,7,9,10,11,12), younger (6,7,8,13), nonwhite (7,14), and unemployed (6,7,12,15). Repeat users are also more likely to be unaccompanied or self-referred to the psychiatric emergency service (10,11,12,13,16,17) and to have a psychotic disorder (5,6,7,8,10,15,16,18), a history of previous psychiatric hospitalizations (7,9,13,16), and a history of current or previous psychiatric treatment (10,12,13,15,16). They are also more likely to be perceived as a threat or danger to self or others at the time of the initial evaluation (6,16).
The primary factors found to be helpful in preventing hospital returns were hospitalization after the initial evaluation (9,19,20,21,22) and participation in an aftercare program (9). Despite this growing knowledge base, few studies have considered the possibility that current constraints on the use of inpatient care may prevent us from devoting enough time to the initial psychiatric inpatient care of these needy and troubled patients. In attempting to reduce inpatient costs by restricting hospital admissions or inpatient stays after the initial evaluation, we may fail to adequately treat the patient's condition and, therefore precipitate a later return to the psychiatric emergency service.
This study examined factors contributing to recidivism after evaluation in the psychiatric emergency service. The study moves beyond previous investigations because, in addition to other data, it considers data on patients' clinical characteristics that were collected in observations of patients' initial evaluations. It further takes into account patients' experiences after evaluation in the psychiatric emergency service as predictors of their involuntary return at a future time.
Methods
Sample and process
Data on 482 patients evaluated in the psychiatric emergency services of seven county general hospitals in the San Francisco Bay Area during the period from October 1983 to September 1986 were collected from independent observation of psychiatric evaluations, patient records, and responses to a brief questionnaire completed by staff clinicians in the emergency services. Subjects were chosen consecutively at entry into the psychiatric emergency services. An incoming patient was included in the sample if both an independent observer and a staff clinician were available for the patient's evaluation. Clinical observations were completed at various time intervals spread around the clock and on all days of the week. Thus the sample was random in character.
The mental health professionals who collected data for the study were experienced in assessing patients with severe mental illness. They were trained to use structured instruments to record their observations and the results of chart reviews and to complete structured process notes. During the study period, observers had access to staff members' in-person and telephone conversations with and about patients and to all patients' records.
Evaluating clinicians were primarily psychiatrists or other physicians (for 50 percent of the patients) but also included registered nurses (for 16.4 percent of patients), master's-level psychologists and social workers (6.8 percent), licensed psychiatric technicians (6.2 percent), other trainees (4.3 percent), doctoral-level psychologists (2.5 percent), and persons with other credentials (7.4 percent). Most nonpsychiatrists had a psychiatrist available for consultation. The evaluators had a mean±SD of 10.5±10 years of clinical experience (median, seven years), 6±5.4 years of experience in psychiatric admissions (median, five years), and 5.5±4.8 years of experience in the psychiatric emergency service (median, five years). Actual time for initial evaluations ranged from 15 minutes to ten hours, with a mean±SD of 1.42±1.22 hours and a median of one hour.
Twelve months after the initial evaluation, patients' mental health and criminal justice records were reviewed by the research staff, often the same individuals who had done the initial observations, for evidence of involuntary return to a psychiatric emergency service at these seven county general hospitals. Information was gathered on insurance coverage and conformity to medication and referral recommendations that were made at the initial evaluation. Vital statistics and criminal justice records were also checked for evidence of death or incarceration during the follow-up period.
Sixty-five of the patients were excluded from the analysis. Twenty-four had either died or were incarcerated in prison or jail during the follow-up period, and 41 had returned to a psychiatric emergency service voluntarily. The final sample consisted of 417 patients.
Measures
Whether a patient was involuntarily returned to a psychiatric emergency service in the San Francisco Bay Area in the 12-month period following the initial evaluation was the criterion variable for the study. The predictor variables were patients' demographic characteristics and clinical history, admission criteria from the initial evaluation, and measures of patients' status after the initial evaluation.
Demographic characteristics included age, gender, and ethnicity. Clinical history included the number of psychiatric hospitalizations before the evaluation in the psychiatric emergency service. These variables have often been cited in the literature as significant factors contributing to recidivism.
Because involuntary return to the psychiatric emergency service was the criterion variable, the analysis included four admission criteria from the initial psychiatric evaluation that had been used by clinicians in making decisions about retaining patients in a controlled hospital setting. The first variable was whether the emergency service clinician assigned the patient a diagnosis of a psychotic disorder.
The second was whether the psychiatric disorder was viewed as treatable by the clinician; this variable was measured using the Treatability Scale (23). This scale is made up of nine items coded either 0 or 1. Items include whether the record or the assessment indicates that the patient will comply with medication schedules, can be involved in psychotherapy, or can be consistent about a decision to seek treatment. Item codes are summed, and their mean constitutes the treatability score, assuming information is available on at least five of the items. Thus scores on the Treatability Scale can range from 0 to 1, with higher scores indicating a higher likelihood that the patient is treatable.
The third variable was the patient's ability to benefit from hospitalization, as measured by the Benefit From Hospitalization Scale (23). This scale is made up of three items coded either 0 or 1. The first item is whether the person's chart included a recommendation suggesting that future hospitalization might be necessary or useful. The second item is whether the record indicates that referrals made for treatment of this patient in this condition did not work out. The third item is whether the evaluation or the record indicates that the patient's condition at the time of the assessment requires stabilization, observation, or continued evaluation in a hospital setting. The items are summed and divided by three. Thus possible scores on the scale range from 0 to 1, with higher scores indicating less ability to benefit from hospitalization.
The fourth variable was the patient's likelihood of causing harm to self or to others or of being gravely disabled at the time of the initial evaluation; this variable was measured using the Three Ratings of Involuntary Admissibility (TRIAD) Scale (24,25,26). TRIAD consists of 88 items that can be combined to yield 155 patterns of behavior and circumstances relevant to the clinical prediction of violence and suicide and the assessment of grave disability. Observers gather information for the items during the assessment but are blind to the pattern scoring, which is done by computer. Possible scores on the TRIAD scale range from 0 to 11, with higher scores indicating increased dangerousness.
Four measures of patients' status after the evaluation were also included. They were the number of days the patient spent in a psychiatric hospital after the initial evaluation and discharge, whether the patient had medical or health insurance, whether the patient complied with medication, and whether the patient complied with referral recommendations that resulted from the initial evaluation.
Analyses
Data on patients' demographic characteristics are reported. Univariate analyses were used to determine which variables predicted whether patients were involuntarily returned to the psychiatric emergency service within 12 months. Group differences were evaluated using t tests and chi square tests. A logistic regression model was used to demonstrate the relative importance of indicators of patients' involuntary return to the psychiatric emergency service.
Results
Patients' characteristics
The demographic characteristics of the 417 patients in the final sample suggested that the study subjects were a marginal group at high risk for involvement with the mental health and health care systems and with social services and law enforcement agencies. The typical client was male (58 percent), 36.3 years of age, and not black (82 percent) and had a history of 4.6 previous psychiatric hospitalizations before the initial evaluation.
At the end of the initial evaluation, the sample's mean±SD Global Assessment Scale score was 37.1±13.32, indicating that most patients had serious difficulty in their daily functioning. Most of the patients in the sample had a diagnosis of a psychotic disorder (275 patients, or 66 percent). Of those with a psychotic diagnosis, 153 had a schizophrenic condition (56 percent), 61 had an affective disorder (22 percent), and 61 had another type of psychotic condition, for example, alcohol-related psychosis (22 percent). Although clinicians did not have enough time to make an accurate substance abuse diagnosis during the initial evaluation in the psychiatric emergency service, 138 patients, or 33 percent, had a condition that was complicated by substance abuse at the time of their evaluation. This complication was significantly more likely to be present among patients with a nonpsychotic diagnosis (49 percent versus 27 percent of patients with a psychotic disorder; χ2 =18.68, df=1, p<.001).
As a result of the initial evaluation, 66 percent of the patients were retained in an inpatient facility. These patients remained hospitalized for an average of six days.
Univariate comparisons
During the 12-month period after the initial evaluation, 121 of the 417 patients (29 percent) were involuntarily returned to a psychiatric emergency service in the San Francisco Bay Area.
Involuntary returnees and nonreturnees did not differ in age, gender, race, involvement with substance abuse, or the number of previous psychiatric hospitalizations before the initial evaluation in the psychiatric emergency service. Compared with nonreturnees, returnees spent more days in the hospital after the evaluation in the psychiatric emergency service (mean±SD=5.8±9.9, compared with 3.3±6.7 for nonreturnees; t= 2.53, df=166, p=.01).
At the initial evaluation the returnees were more likely than nonreturnees to be more seriously impaired on three of the four admission criteria. They were more likely than nonreturnees to have a psychotic disorder (85 percent, compared with 67 percent of nonreturnees; χ2 =14.22, df=1, p<.001), to be rated as more dangerous (TRIAD mean±SD=3.55±2.3, compared with 2.98±2.2 for nonreturnees; t=2.4, df=415, p=.02), and to be deemed less treatable (Treatability Scale mean±SD =.36±.23, compared with .42±.24; t=2.29, df=415, p=.02). However, returnees were not perceived as more likely to benefit from hospitalization than nonreturnees.
On the postevaluation status indicators likely to affect future readmission, the returnees were more likely to have been insured than nonreturnees (72 percent versus 59 percent; χ2 =6.31, df=1, p=.012). The returnees were also more likely to comply with their referrals for treatment than were nonreturnees, although the difference did not reach significance (25 percent versus 18 percent). The two groups did not differ significantly on reported medication compliance.
Multivariate analysis
As shown in Table 1, the primary predictors of patients' involuntary return to the psychiatric emergency service were a diagnosis of a psychotic disorder and the seriousness of their presentation during the initial evaluation, as indicated by their score on the TRIAD measure of dangerousness. Patients with a psychotic diagnosis were 238 percent more likely to experience an involuntary return to the psychiatric emergency service within 12 months, compared with patients without a psychotic diagnosis. For each clinically significant increase in the TRIAD dangerousness score (a 3-point increase), patients were 33 percent more likely to experience an involuntary return to the psychiatric emergency service within 12 months. This 3-point difference is clinically meaningful in that it is associated with the clinician's view that the patient is dangerous enough to be involuntarily admitted to an inpatient facility under the three dangerousness criteria—danger to self, danger to others, or grave disability. Patients with insurance were 176 percent more likely to have an involuntary return to the psychiatric emergency service within 12 months, compared with patients without insurance.
Discussion
Our findings indicate that the likelihood of an involuntary return to the psychiatric emergency service was dependent on the same factors that initially brought the patients to the service—their psychosis and level of dangerousness. Having insurance or the financial resources to pay for services also increased the probability of an involuntary return to the psychiatric emergency service. It is noteworthy that interventions initiated after the patients' evaluation in the psychiatric emergency service were not significant predictors of their involuntary return to the emergency service, nor did they, as in past studies, prevent involuntary return. Specifically, patients' compliance with medications or with referral recommendations did not predict involuntary return, nor did the number of days of hospitalization after the initial evaluation.
These results must be understood in the light of the definition of dangerousness that constituted the TRIAD assessment tool. High scores on the TRIAD scale result from the combination of behaviors and circumstances that in concert lead to the perception that an individual is dangerous because of a mental disorder and civilly committable. Individuals who are released or discharged from the psychiatric emergency service or from the hospital after an admission precipitated by an evaluation in the emergency service were likely to return involuntarily because of the same circumstances that brought them to the service in the first place.
The crisis-oriented nature of the current service system, including the brief stays in psychiatric hospitals, halfway houses, or other alternative and less restrictive living situations, provides a structure that contributes to the pattern of rehospitalization within 12 months. Furthermore, the extent of outpatient support for all but the high-cost patients is limited. The low levels of outpatient psychiatric care available to most patients have only a residual effect on their outcomes. Patients, therefore, return to the psychiatric emergency service with a new psychotic episode, are again perceived as a threat or danger to themselves or others, and the revolving-door syndrome continues.
Our findings replicate those of Lyons and associates (27) in showing that the only significant predictors of a return to an inpatient setting were the same clinical characteristics that initially brought patients to the psychiatric emergency service. However, our interpretation of these findings differs from those of Lyons' group. In adopting a pro-managed-care perspective, Lyons' group tended to use their results to dismiss the critical role of inpatient stays in hospital outcomes. Yet Appleby and colleagues (19) found that increased length of hospitalization was negatively related to the probability of readmission.
This discrepancy in the findings may be explained by variability in the lengths of hospitalization of the patients in these three studies. The average patient in our study stayed in the hospital six days after entering the psychiatric emergency service. The patients in the study by Lyons and associates also averaged six days of hospitalization. In contrast, Appleby's patient group was hospitalized for a median of 17 days, with a third of the patients staying more than 30 days. We believe that hospital admissions have now become so short that, for many patients, they preclude any successful resolution of the initial circumstances that brought the person to the hospital.
These conclusions are further reinforced by Klinkenberg and Calsyn's findings (9) that hospital admission after the initial episode in the psychiatric emergency service was associated with prevention of returns to the service. In their study, patients were hospitalized for an average of 24 days—four times the length of stay of the patients in our study and in the study by Lyons and colleagues (Klinkenberg WD, personal communication, 1997).
We did an additional analysis to further test the hypothesis that hospital stays have been so unduly shortened that they may now have become irrelevant in linear modeling of return to the psychiatric emergency service. We cross-tabulated the duration of hospital stay after evaluation in the psychiatric emergency service and patient recidivism within 12 months. Duration of stay was divided into four categories: less than 24 hours—generally overnight and some part of the following day (the situations of patients with this length of stay were believed to be most easily resolved); one to eight days; nine to 16 days; and 17 days or more, the median duration reported by Appleby and colleagues (19) in which the prophylactic effects of hospitalization were obtained. Also at 17 days, clinicians in our study had to seek a renewal of certification orders if the patient was to be retained. This requirement to justify continued treatment under conditions of bed scarcity is similar to that faced by clinicians who must seek authorization for extended treatment under managed care utilization review.
The categorical cross-tabulation was significant (χ2 =8.3, df=3, p=.03) and seemed to indicate a curvilinear relationship in the data. Those individuals staying less than 24 hours returned at a rate of one in four (26.5 percent); the group who stayed one to eight days returned at a rate of more than one in three (37.8 percent); the group who stayed nine to 16 days returned at a rate of one in two (49 percent); and the group who stayed 17 days or more returned at a rate of less than one in three (32 percent). The data suggest that stays of the mid-range groups were too brief to resolve their situations, and they support the observation that had the clinicians not faced a difficult process of justifying continued hospitalization, the situations of these individuals might have been more adequately resolved. The culprit may be the strict recertification requirements, but the analogy to clinical justification under managed care utilization review with conditions of bed scarcity is very strong.
White and associates (28) found insurance coverage to be a factor predicting admission after evaluation in the psychiatric emergency service. When Medicaid coverage is included as a type of insurance, the insured patients in our study were more likely to return to the psychiatric emergency service. These individuals were most likely to have access to psychiatric care and thus were more likely to come to the attention of people capable of initiating an involuntary return to the emergency service. More important, they had resources to cover the costs of care that they apparently still required. It must be emphasized that patients in our sample, whether in the returnee or nonreturnee groups, were rated as having a strong ability to benefit from hospitalization.
The results of our study are generalizable only to the patient population served by the seven hospitals in the San Francisco Bay Area from which the study sample was drawn. Yet the findings have significant implications in a penurious system based on managed care principles and focused on crisis prevention rather than long-term care. Extensive restrictions on inpatient care may be penny wise and pound foolish, especially in health care environments that have already negotiated reduced rates for inpatient care.
Our findings suggest that the more critical goal is to find a means to stabilize the patient's situation at the end of the initial evaluation in the psychiatric emergency service or by the end of the hospitalization that follows the initial evaluation. Particular attention must be given to circumstances contributing to the person's dangerousness or grave disability. Because both factors are defined by combinations of behavior and circumstances, the failure to allow enough time to modify the circumstances associated with these factors may lead to the patient's return to the psychiatric emergency service.
Conclusions
Managed care produces extreme economic pressure to limit the use of psychiatric emergency services and inpatient hospitalization. This study found that the patient's condition at the initial evaluation was the most important factor predicting recidivism. Other factors such as psychiatric hospitalization history, demographic characteristics, the duration of hospitalization after the initial evaluation, or the patient's conformity with the aftercare regimen did not predict recidivism. It may be necessary to consider using longer inpatient stays after the initial evaluation to reduce the likelihood of involuntary return to the psychiatric emergency service. In our cost-conscious environment, obtaining greater access to inpatient care is increasingly difficult. At the least, greater emphasis must be placed on developing supervised residential alternatives to inpatient care (29).
The results of our study as well as those of other studies, such as the one by Appleby and associates (19), suggest that brief hospitalization, currently the mainstay of treatment efforts, may be insufficient to meet the needs of patients with serious mental illness. Such brief hospital stays may be merely setting up the conditions for a revolving-door effect or Band-Aid treatment. These conditions, however, cannot be attributed to the lack of high-quality efforts on the part of hard-working and often frustrated hospital staff members (30). More likely they derive from a lack of financial resources. For example, we found that when these resources were present, inpatient care was more likely to be available. The probability that patients would receive additional inpatient care during the 12-month follow-up period was 172 percent higher for patients with insurance than for those without it. Rather than being an abuse of available insurance, this increased use of inpatient care is more likely a recognition of the patient's ability to benefit from such care.
Acknowledgments
This study was supported by grant RO1-MH-37310 and training grant MH-18828 from the National Institute of Mental Health.
Dr. Segal is professor and director of the mental health and social welfare research group in the School of Social Welfare at the University of California, Berkeley. Dr. Akutsu and Dr. Watson are affiliated with the research group. Dr. Akutsu is also assistant professor at Pacific Graduate School of Psychology in Palo Alto, California. Address correspondence to Dr. Segal, Mental Health and Social Welfare Research Group, School of Social Welfare, 120 Haviland Hall (MC 7400), University of California, Berkeley, California, 94720-7400 (e-mail, [email protected]).
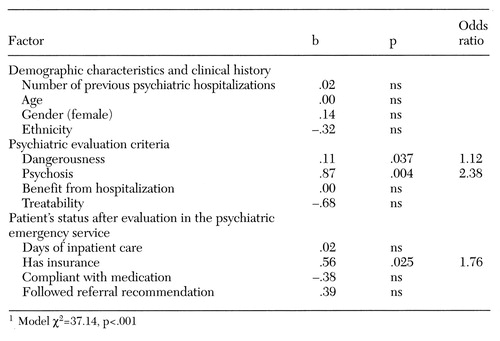 |
Table 1. Factors predicting patients' involuntary return to the psychiatric emergency service within 12 months of an initial evaluation (N=417)1
1. Winegar N: The Clinician's Guide to Managed Mental Health Care. Binghamton, NY, Haworth, 1992Google Scholar
2. Dorwart RA: Managed mental health care: myths and realities in the 1990s. Hospital and Community Psychiatry 41:1087-1091, 1990Abstract, Google Scholar
3. Fishel L, Janzen C, Bemak F, et al: A preliminary study of recidivism under managed mental health care. Hospital and Community Psychiatry 44:919-920, 1993Abstract, Google Scholar
4. Ellison JM, Blum N, Barsky AJ: Repeat visitors in the psychiatric emergency service: a critical review of the data. Hospital and Community Psychiatry 37:37-41, 1986Abstract, Google Scholar
5. Oyewumi LK, Odejide O, Kazarian SS: Psychiatric emergency services in a Canadian city: I. prevalence and patterns of use. Canadian Journal of Psychiatry 37:91-95, 1992Crossref, Medline, Google Scholar
6. Nurius PS: Emergency psychiatric services: a study of changing utilization patterns and issues. International Journal of Psychiatry in Medicine 13:239-254, 1983Crossref, Medline, Google Scholar
7. Sullivan PF, Bulik CM, Forman SD, et al: Characteristics of repeat users of a psychiatric emergency service. Hospital and Community Psychiatry 44:376-380, 1993Abstract, Google Scholar
8. Surles RC, McGurrin MC: Increased use of psychiatric emergency services by young chronic mentally ill patients. Hospital and Community Psychiatry 38:401-405, 1987Abstract, Google Scholar
9. Klinkenberg WD, Calsyn RJ: The moderating effects of race on return visits to the psychiatric emergency room. Psychiatric Services 48:942-945, 1997Link, Google Scholar
10. Perez E, Minoletti A, Blouin J, et al: Repeated users of a psychiatric emergency service in a Canadian general hospital. Psychiatric Quarterly 58:189-201, 1986-1987Google Scholar
11. Slaby AE, Perry PL: Use and abuse of psychiatric emergency services. International Journal of Psychiatry in Medicine 10:1-8, 1980Crossref, Medline, Google Scholar
12. Voineskos G: New chronic patients in the emergency service. Psychiatric Journal of the University of Ottawa 10:95-100, 1985Medline, Google Scholar
13. Bassuk E, Gerson S: Chronic crisis patients: a discrete clinical group. American Journal of Psychiatry 137:1513-1517, 1980Link, Google Scholar
14. Snowden LR, Holschuh J: Ethnic differences in emergency psychiatric care and hospitalization in a program for the severely mentally ill. Community Mental Health Journal 28:281-291, 1992Crossref, Medline, Google Scholar
15. Munves PI, Trimboli F, North AJ: A study of repeat visits to a psychiatric emergency room. Hospital and Community Psychiatry 34:634-638, 1983Abstract, Google Scholar
16. Ellison JM, Blum NR, Barsky AJ: Frequent repeaters in a psychiatric emergency service. Hospital and Community Psychiatry 40:958-960, 1989Abstract, Google Scholar
17. Lim MH: A psychiatric emergency clinic: a study of attendance over six months. British Journal of Psychiatry 143:460-466, 1983Crossref, Medline, Google Scholar
18. Hansen TE, Elliott KD: Frequent psychiatric visitors to a Veterans Affairs medical center emergency care unit. Hospital and Community Psychiatry 44:372-375, 1993Abstract, Google Scholar
19. Appleby L, Desai PN, Luchins DJ, et al: Length of stay and recidivism in schizophrenia: a study of public psychiatric patients. American Journal of Psychiatry 150:72-76, 1993Link, Google Scholar
20. Caton CLM, Goldstein JM, Serrano O, et al: The impact of discharge planning on chronic schizophrenic patients. Hospital and Community Psychiatry 35:255-262, 1984Abstract, Google Scholar
21. Brown G, Bone M, Dalison B, et al: Schizophrenia and Social Care. London, Oxford University Press, 1966Google Scholar
22. Zolik ES, Lantz EM, Sommers R: Brief versus standard psychiatric hospitalization: a review of the literature. Community Mental Health Journal 1:233-237, 1965Crossref, Google Scholar
23. Segal SP, Egley L, Watson M, et al: Quality of care and outcomes in the PES. American Journal of Public Health 85:1429-1431, 1995Crossref, Medline, Google Scholar
24. Segal SP, Watson M, Goldfinger S, et al: Civil commitment in the psychiatric emergency room: I. the assessment of dangerousness by emergency room clinicians. Archives of General Psychiatry 45:748-752, 1988Crossref, Medline, Google Scholar
25. Segal SP, Watson M, Goldfinger S, et al: Civil commitment in the psychiatric emergency room: II. mental disorder indicators and three dangerousness criteria. Archives of General Psychiatry 45:753-758, 1988Crossref, Medline, Google Scholar
26. Segal SP, Watson M, Goldfinger S, et al: Civil commitment in the psychiatric emergency room: III. disposition as a function of mental disorder and dangerousness indicators. Archives of General Psychiatry 45:759-763, 1988Crossref, Medline, Google Scholar
27. Lyons J, O'Mahoney M, Miller S, et al: Predicting readmission to the psychiatric hospital in a managed care environment: implications for quality indicators. American Journal of Psychiatry 154:337-340, 1997Link, Google Scholar
28. White CL, Bateman A, Fisher WH, et al: Factors associated with admission to public and private hospitals from a psychiatric emergency screening site. Psychiatric Services 46:467-472, 1995Link, Google Scholar
29. Segal SP, Watson M, Akutsu PD: Quality of care and use of less restrictive alternatives in the psychiatric emergency service. Psychiatric Services 47:623-627, 1996Link, Google Scholar
30. Segal SP, Egley L, Watson M, et al: Quality of care in psychiatric emergency services. Breakthrough 1:17-30, 1997Google Scholar



