Analysis of Health Service Areas: Another Piece of the Psychiatric Workforce Puzzle
Abstract
Planning for development of a national or regional psychiatrist workforce that is the appropriate size must consider numerous issues. They include the dynamics of workforce distribution, effects of managed care, reduction in potential residency slots, participation of international medical graduates, apathy toward the field of psychiatry, service area variations, and increased interest in allied mental health professions, along with the burgeoning global burden of psychiatric illness. This paper examines the application of two benchmark standards for the number of psychiatrists needed per 100,000 population—the standard developed by the Graduate Medical Education National Advisory Committee and the Average Requirement Benchmark—to the supply of psychiatrists in Georgia in 1996 by county and by health service regions, which are geographical units based on health care utilization patterns of Medicare and Medicaid recipients. Areas with a surplus or deficit of psychiatrists are identified. The findings provide contextual evidence of a surplus of psychiatric physicians in the most populous areas of the state, given a substantial presence of health maintenance organizations. The state's less populated rural areas may potentially benefit from a redistribution of the psychiatrist workforce. The authors recommend continued refinement of models to estimate psychiatric workforce needs and suggest development of a comprehensive model that uses needs-based, demand-based, and benchmarking approaches.
Requirements for the size and distribution of the physician workforce continue to evoke significant concern and debate. Health policy makers and planners clearly need to identify the types of physicians that are required and the geographic areas where the requirements are greatest. However, research on this issue has produced conflicting results (1,2,3,4,5,6,7,8,9,10,11,12,13,14,15).
Prediction of workforce needs in psychiatry is particularly complicated due to the complexity of the interrelated factors that influence projections. These factors include the epidemiology of mental illnesses, the distribution and supply of practitioners, the effects of managed care, varying definitions of a full-time practitioner and average workload, the accuracy of population projections, the availability of allied health professionals, employment of international medical graduates, and variations in interest in psychiatry as a specialty among physicians in training (16).
The issue of psychiatric workforce requirements is particularly relevant to the delivery of mental health care in rural areas because the effects of an undersupply of psychiatrists are likely to be felt first in those areas. This paper reports an analysis of the distribution of psychiatrists in Georgia, a predominantly rural state, in 1996.
Several studies sponsored by government and private agencies have addressed the complex issue of psychiatric workforce needs. The results have varied widely, from predicting a significant psychiatrist oversupply to predicting an undersupply (11,12,13,14). Several models for estimating workforce requirements exist, each with its strengths and weaknesses. In a meta-analysis of research on the physician workforce conducted between 1980 and 1990, Feil and colleagues (13) noted five primary models for estimating requirements. These models were of three types—needs based, demand based, and benchmark based. Factors considered in these models included patients' diagnoses and treatment needs, the number of psychiatrists a system could afford, data from other countries, the number of full-time-equivalent staff needed for a given system, and the percentage increase or decrease of staff needed to supply the corresponding demands.
Needs-based planning typically estimates the frequency of disease and compares those estimates with the projected number of physicians available to treat that frequency of disease (1). Panels of experts estimate the number of physicians needed in any given specialty to treat disease according to its incidence and prevalence. Needs-based planning is limited, however, by its inability to react quickly to advances in technology and by the complexity of many medical problems.
Demand-based planning projects future estimates based on the current level of utilization of physicians. This method is limited, because it fails to take into account that use of medical resources increases as the supply of those medical resources increases (1,2). This method also assumes that the current relationship between supply and demand provides adequate care.
Benchmarking, which provides estimates of the number of physicians needed stemming from a standard based on actual use of physicians in a particular health plan or geographical area, is seen as possessing inherent advantages over needs-based and demand-based planning (17).
In reviewing these various models and their potential utility for examining the psychiatric workforce needs for the state of Georgia, it became clear that no current single model adequately addressed all of the salient variables. Because benchmarking is seen to have certain advantages over other approaches, we chose to use this method to examine psychiatric physician workforce needs. To gain a broader view of the issue, our analysis used two benchmark standards that represent different assumptions about the future of health care delivery—the benchmark developed by the Graduate Medical Education National Advisory Committee (GMENAC) (18) and the Average Requirement Benchmark (1), which is based on the utilization patterns of selected health maintenance organizations.
A total of 84.4 percent of the psychiatrists in Georgia practice in Metropolitan Statistical Areas (MSAs). An MSA is an area of contiguous counties that contains at least one city with a population over 50,000 and whose territory is interrelated both economically and socially. Of Georgia's 159 counties, only 54 contain psychiatric physician practices (19). We calculated and compared estimates of the psychiatric physician workforce using both county and health service area boundaries. Georgia's health service areas were adapted from the 1991 Vital and Health Statistics Report prepared by the Department of Health and Human Services (20). This report identified health service areas using a hierarchical cluster analysis of 1988 Medicare data showing which high-level tertiary care hospitals that offer both cardiac and neurological treatment are utilized by Medicare and Medicaid recipients. We viewed health service area boundaries as potentially providing a more accurate picture of health care utilization patterns than county political boundaries. The health service areas also suggest the potential markets for future HMO penetration.
Methods
The GMENAC standard of 15.4 psychiatrists per 100,000 population, which is considered liberal in this era of managed care, and the Average Requirement Benchmark of 8.1 per 100,000 population were used to assess the projected need for psychiatrists according to county and health service area boundaries. The Average Requirement Benchmark represents an average of benchmark rates ranging from the high GMENAC standard of 15.4 psychiatrists per 100,000 population to the low benchmark of 3.8 per 100,000 found in a proposals by Kaiser Permanente (3,21). Many researchers have indicated that the proliferation of HMOs will affect the need for physicians (11,17,22). In addition, current health reform proposals project that a majority of Americans will be enrolled in some form of managed care by the turn of the century. Therefore, it seemed logical to apply benchmark standards that are currently in use by these organizations (11,8,9,10,11,12,13,14,16,17,22,23,24,25,26). Given the wide variety of benchmarking standards, the Average Requirement Benchmark provides a useful tool for health planners in considering the possible consequences of managed care for the psychiatric workforce.
Using data from The Dartmouth Atlas of Health Care in the United States (17), we calculated the number of psychiatrists in 1996 for each county and health service area in Georgia. The GMENAC standard of 15.4 psychiatrists per 100,000 population and the Average Requirement Benchmark of 8.1 psychiatrists per 100,000 population were applied to both the counties and the health service areas, and the surpluses or deficits in each location were determined.
Results
Four maps of Georgia were created, two using county boundaries and two using health service area boundaries. Figure 1 and Figure 2 show application of the GMENAC and Average Requirement Benchmark standards to the counties and health service areas.
Figure 1 shows the results of applying the GMENAC standard. Using the GMENAC standard of 15.4 psychiatrists per 100,000 population, 149 of Georgia's 159 counties had a deficit of psychiatrists, and only ten had a surplus. Using the GMENAC method, four health service areas showed a surplus of psychiatrists and the remaining 27 had a deficit.
Figure 2 provides a graphical representation of the Average Requirement Benchmark applied to Georgia's counties and health service areas. Using the Average Requirement Benchmark of 8.1 psychiatrists per 100,000 population, the number of counties with a surplus increased to 25, and 134 counties had a deficit. When the Average Requirement Benchmark was applied to the health service areas, the number of surplus areas increased to eight, with 23 remaining in the deficit range.
Table 1 provides a synopsis of the effects of applying the GMENAC and Average Requirement Benchmark standards to the counties and health service areas. Of interest is the difference the service area definition makes in the percentage of the population in areas of surplus or deficit. Applying the GMENAC standard on a county-by-county basis resulted in a distribution of 27 percent of Georgia's population in areas of surplus and 73 percent in areas of deficit. When the Average Requirement Benchmark was applied county by county, the percentage of the population in areas of surplus jumped to 46 percent, with the remaining 54 percent of the population in areas of deficit. Correspondingly, when health service areas were used as the units of measure, the GMENAC standard yielded 38 percent in surplus areas and 62 percent in deficit areas. When the Average Requirement Benchmark was applied to areas, 54 percent of the state's population was in a surplus area, and 46 percent was in a deficit area.
Thus when the Average Requirement Benchmark, which represents a moderate HMO penetration, was used, as much as 54 percent of the state's population was in an area with too many psychiatrists. Consequently, psychiatrists in surplus areas may be encouraged to relocate to more rural areas where no surplus was evident.
Discussion and conclusions
The application of the Average Requirement Benchmark and the more liberal GMENAC standard to health service areas should be viewed as yet another piece of the workforce puzzle. Along with previous research, these results may lead to a better understanding of this complex issue. Applying the two benchmark standards—one liberal and one moderate—to two types of service areas shows how wide the differences between workforce projections can be.
As for the state of Georgia, the results of this analysis show how the service area designation (counties or health service areas) and standard used (GMENAC standard or Average Requirement Benchmark) affects calculation of the need for psychiatric physicians. On the negative side, psychiatrists in surplus areas may be forced to relocate. On the positive side, the state's rural areas may potentially benefit from a redistribution of this workforce.
With few exceptions, the majority of recent studies have reported evidence of a physician oversupply, based on their underlying assumptions. The familiar phrase "It all depends on how you look at it" seems strikingly applicable when assessing projections for the psychiatric workforce. As Jay Scully, M.D., former director of the American Psychiatric Association's office of education, has stated, projections for the future depend on the model used to predict workforce needs (14). On the one hand, the approach for estimating the number of psychiatrists that comes closest to doing what is right for patients is the approach based on their needs (12). However, when one moves from the idealistic to the realistic, current utilization patterns and the potential influence of managed care must be considered. Clearly, a significant difference is seen in the workforce need for psychiatric physicians depending on the underlying assumptions, including both the calculations used and the boundaries of the geographic areas to which they are applied.
Some have suggested that given the limitations of current forecasts and the difficulties in improving on them, policy may have to be driven by more practical considerations, such as how many physicians we can afford (13). Perhaps the answer lies not in arguing over which study is correct, but rather in seeing the results of each model as an important piece of the overall puzzle to which new models and estimates can be added, bringing us closer to an understanding this complex subject.
Future research may usefully explore the development of a new comprehensive model that incorporates the strengths of needs-based, demand-based, and benchmarking approaches. This new model may be capable of weighting the elements included in calculations, resulting in a more accurate methodology for psychiatric workforce projection. In addition, researchers may wish to consider the development of an outcomes-based model for workforce projections. Developers of such a model would need to determine what types of outcomes should result from addressing the psychiatric burden of illness and then determine how many psychiatrists would be needed to accomplish this task.
Clearly, a major issue facing researchers in this area is the lack of a gold-standard workforce projection methodology. Researchers should continue their efforts to develop such a methodology. Perhaps then all the necessary pieces of this complicated puzzle will be brought into place and the stage will be set for addressing tomorrow's psychiatric workforce needs.
The authors are affiliated with the community science program at Mercer University School of Medicine, 1550 College Street, Macon, Georgia 31207. Dr. Eveland is assistant professor, Dr. Dever is associate dean for primary care, Dr. Schafer is assistant professor, Ms. Sprinkel is instructor, Ms. Davis is research analyst, and Ms. Rumpf is program coordinator. Send e-mail to Dr. Eveland at [email protected]. This paper is one of several on rural psychiatry in this issue.

Figure1Countries and health service areas in Georgia with a surplus or deficit of psychiatrists, based on the Graduate Medical Education National Advisory Committee (GMENAC) standard, 19961
1The GMENAC standard is 15.4 psychiatrists per 100,000 population.
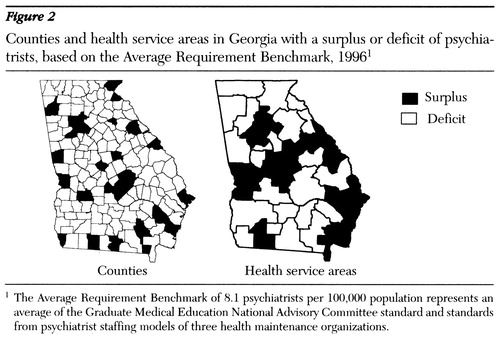
Figure 2. Countries and health service areas in Georgia with a surplus or deficit of psychiatrists, based on the Average Requirement Benchmark, 19961
1 The Average Requirement Benchmark of 81 psychiatrists per 100,000 population represents an average of the Graduate Medical Education National Advisory Committee standards from pyschiatrist staffing models of three health maintenance organizations.
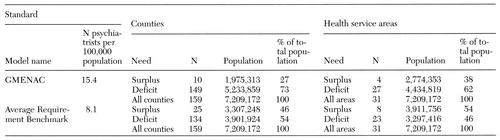 |
Table 1. Psychiatric workforce needs in Georgia based on the standard of the Graduate Medical Education National Advisory Committee (GMENAC) and the Average Requirement Benchmark, by counties and health service areas, 1996
1. Schroder SA: How can we tell whether there are too many or too few physicians? The case for benchmarking. JAMA 276:1841-1843, 1996Crossref, Medline, Google Scholar
2. Goodman DC, Fisher ES, Bubolz TA, et al: Benchmarking the US physician workforce: an alternative to needs-based or demand-based planning. JAMA 276:1811-1817, 1996Crossref, Medline, Google Scholar
3. McClendon BJ, Politzer RM, Christian E, et al: Downsizing the physician workforce. Public Health Reports 112:231-239, 1997Medline, Google Scholar
4. Scully JH, Weissman SH: The psychiatric workforce in transition, in The American Psychiatric Press Review of Psychiatry, vol. 15. Edited by Dickstein LJ, Riba MB, Oldham JM. Washington, DC, American Psychiatric Press, 1996Google Scholar
5. Sierles FS, Taylor MA: Decline of US medical students' career choice of psychiatry and what to do about it. American Journal of Psychiatry 152:1416-1424, 1995Link, Google Scholar
6. American Psychiatric Association, American Academy of Child and Adolescent Psychiatry, America Association for Geriatric Psychiatry: Joint Statement on Graduate Medical Education to the House Ways and Means Subcommittee on Health, US Congress, Apr 16, 1996Google Scholar
7. American Psychiatric Association, American Academy of Child and Adolescent Psychiatry, American Association for Geriatric Psychiatry: Joint Statement on Graduate Medical Education to the House of Representatives Ways and Means Committee, Subcommittee on Health, Washington, DC, Apr 16, 1996Google Scholar
8. Scully JH: Why be concerned about recruitment? American Journal of Psychiatry 152:1413-1414, 1995Google Scholar
9. Murry CJL, Lopez AD (eds): The Global Burden of Disease: A Comprehensive Assessment of Mortality and Disability From Diseases, Injuries, and Risk Factors in 1990 and Projected to 2020. Cambridge, Mass, Harvard School of Public Health, 1996Google Scholar
10. Schwartz AL: Will competition change the physician workforce? Early signals from the market. Academic Medicine 69:245-260, 1994Crossref, Medline, Google Scholar
11. Tarlov AR: HMO enrollment growth and physicians: the third compartment. Health Affairs 5(1):23-35, 1986Google Scholar
12. Faulkner LR, Goldman CR: Estimating psychiatric manpower requirements based on patients' needs. Psychiatric Services 48:666-670, 1997Link, Google Scholar
13. Feil E, Welch G, Fisher E: Why estimates of physician supply and requirements disagree. JAMA 269:2659-2663, 1993Crossref, Medline, Google Scholar
14. Moran M: Experts disagree on how many psychiatrists needed in future. Psychiatric News, Dec 2, 1994, pp 2,16Google Scholar
15. Knesper DJ: Documenting a shortage of psychiatrists: the repair shop model. American Journal of Psychiatry 137:1439-1442, 1980Link, Google Scholar
16. Weissman S: Recruitment and workforce issues in late 20th century American psychiatry. Psychiatric Quarterly 67:125-137, 1996Crossref, Medline, Google Scholar
17. Wennberg JE, Cooper MM (eds): The Dartmouth Atlas of Health Care in the United States. Chicago, American Hospital Publishing, 1996Google Scholar
18. Report of the Graduate Medical Education National Advisory Committee to the Secretary, Department of Health and Human Services. DHHS Pub (HRA) 81-651. Washington, DC, US Department of Health and Human Services, Health Resources Administration, Office of Graduate Medical Education, Sept 30, 1980Google Scholar
19. Dever GEA, Sprinkel C: Physician Workforce 1996: Toward the Year 2000. Atlanta, Joint Board of Family Practice, 1997Google Scholar
20. Vital and Health Statistics: Health Service Areas for the United States: Series 2: Data Evaluation and Methods. DHHS Pub (PHS) 92-1386. Washington, DC, US Department of Health and Human Services, Nov 1991Google Scholar
21. Morgan KO, Morgan S (eds): Health Care State Rankings 1997. Lawrence, Kans, Quitno, 1997Google Scholar
22. Steinwachs D, Weiner JP, Shapiro S, et al: A comparison of the requirements for primary care physicians in HMOs with projections made by the Graduate Medical Education National Advisory Committee. New England Journal of Medicine 314:217-222, 1986Crossref, Medline, Google Scholar
23. Weiner JP: The demand for physician services in a changing health care system: a synthesis. Medical Care Review 50:411-449, 1993Crossref, Medline, Google Scholar
24. Wennburg J, Goodman D, Nease R, et al: Finding equilibrium in the US physician supply. Health Affairs 12(2):89-103, 1993Google Scholar
25. Mullan F, Rivo ML, Politzer RM: Doctors, dollars, and determination: making physician workforce policy. Health Affairs 12(suppl):138-151, 1993Google Scholar
26. Straub W: Requirements for Primary Care Physicians Under Managed Competition. Jackson Hole, Wyo, Jackson Hole Group, 1993Google Scholar



