Clinicians' Decision Making About Involuntary Commitment
Abstract
OBJECTIVE: Clinicians' decision making about involuntary commitment was examined, with a focus on the effects of patient and clinician characteristics and bed availability on decisions to detain patients, the first step in involuntary commitment. METHODS: Eighteen psychologists and social workers in the emergency service of a community mental health center completed the Risk Assessment Questionnaire for 169 consecutive patients they deemed to present some degree of risk. Forty-two patients were detained. RESULTS: Three underlying constructs were significantly associated with a patient's overall risk rating, which in turn predicted the decision to detain. Two were clinician characteristics: the clinician detention ratio, which reflects the proportion of patients detained by the clinician in the past three months, and the setting in which the evaluation occurred, either an in-house emergency service or a mobile crisis unit. The availability of detention beds in the community was also a significant predictor of whether a patient would be detained. No patient characteristic, including diagnosis, sex, age, or insurance status, was significantly related to the detention decision. CONCLUSIONS: The findings suggest that the decision-making process is influenced by multiple factors, such as setting, the clinician's tendency to detain patients, and the availability of detention beds.
The decision to involuntarily commit an individual has become more challenging due to rapid changes in health care. A growing body of research on commitment issues has provided some empirical understanding of this process. Studies have examined decisions in relation to legal criteria of commitment statutes (1,2,3,4,5,6,7,8,9,10,11,12,13,14), symptoms associated with the decision to commit (1,2,8,10,12,15,16), and the effects of clinician variables (2,6,13) and situational variables (2,3,4,6).
Some data suggest that clinicians' judgments are consistent with legal requirements for commitment (1,4,8,9,10). Other studies note that in addition to the legal criteria, clinicians may take other factors into account, such as treatability or availability of outside resources (2,5,7,13,17). However, the consistency with which clinicians agree on commitment varies.
Even when clinicians' judgments are consistent with the law, unexplained variations in decision making exist. Factors such as the patient's outside support, treatability, residential status (1,13,18,19), diagnosis and dangerousness (8,11,15), and negative attitude, age, and education (16) have been found to have significant effects on decision making, or to correlate with commitment status.
Less research has been reported on the role of clinician characteristics. Some studies have investigated the effects of professional status (6,13), and others have produced conflicting reports of the effects of clinicians' experience on commitment decisions (2,20).
Although the research cited above has addressed some of the central issues, little analysis has been done of the actual process by which clinicians arrive at the decision to involuntarily commit a patient (21). This study investigated the relationships between patient and clinician characteristics, bed availability, clinicians' assessment of overall risk, and the decision to detain patients for commitment.
Methods
Design
The study was conducted in Virginia, where persons can be involuntarily committed only if they present a danger either to themselves or to others or have a substantial inability to care for themselves because of mental illness. This assessment is made by a clinician, who arranges detention in a psychiatric facility if one of the criteria is met. The patient is then seen by a judge who decides whether the patient can legally be committed. This study involved only the mental health assessment and thus refers to the decision to detain rather than to commit.
Emergency service clinicians in an outpatient community mental health center completed questionnaires rating the risk factors of consecutive patients evaluated between 8 a.m. and midnight from March 1989 to May 1989. After all clinical decisions had been made, clinicians completed questionnaires on all patients with some degree of risk who were seen either in the in-house emergency service or on the mobile crisis unit.
The questionnaire examined 17 independent variables that included patient characteristics, such as diagnosis, age, sex, and health insurance; several ratings of risk; and clinician characteristics, such as setting, years of experience, discipline, age, and sex. The questionnaire also included a clinician detention ratio, which reflects a clinician's tendency to detain patients in the past three months (22). The availability of detention beds (involuntary) and state and private beds in local psychiatric hospitals (voluntary) were additional independent variables. The two dependent variables were the overall risk rating and the decision to detain.
Subjects
Eighteen clinicians between the ages of 29 and 52 who had from one to 20 years of experience participated in the study. Eight clinicians were men. Six clinicians were social workers, and 12 were psychologists. Seventy-two percent of the 169 evaluations examined in this study were done in the emergency service, and 28 percent on the mobile crisis unit.
Measures
As described elsewhere (22), the Risk Assessment Questionnaire (RAQ) is used to collect demographic, insurance, and diagnostic information about the patient; data on detention, release, or voluntary hospitalization; and information about the clinician's awareness before the evaluation of the current availability of detention and voluntary beds in the community. The RAQ also asks the clinician to rate the importance of three risk categories—danger to self, danger to others, and substantial inability to care for self—in the decision-making process about commitment. In addition, the RAQ tracks the clinician's assessment of the patient's risk.
Each of the three legal risk categories and a category of exacerbating factors, such as substance abuse, impaired impulse control, and availability of personal or professional support, are examined. In each category, nine to 12 descriptors are rated using 7-point Likert scales. Summary judgments of risk in each category and of the patient's overall level of risk are also rated using 7-point Likert scales.
Statistical analyses
The internal consistency of each scale was assessed with Cronbach's alpha and reassessed after each descriptor score was multiplied by the exacerbating-factors score. The resulting interactive scales demonstrated even greater reliability (23) than the simple scales. The scores within each risk category were then averaged to produce one overall descriptor score for each patient for each of the three risk categories.
As reported in an earlier study (22), a progression of analyses led to the hypothesis that the three subscales in each of the risk categories could be combined and tested with a factor analysis. Accordingly, a factor analysis using a Varimax rotation was performed on the nine variables (descriptor score, risk rating, and importance rating for each of the three risk categories) to test the hypothesis that the variables might be measures of one or more underlying constructs used by clinicians in evaluating patients.
Regression analyses were then used to test the effects of patient, clinician, and bed variables. When the effect on overall risk rating was examined, multiple regression statistics were used. Logistic regression analyses were used to test the ability of these variables to predict disposition.
Results
Table 1 summarizes results from the RAQ for the 169 patients included in the study. Table 2 gives the distribution of the risk rating scores for the sample.
Factor analysis of the nine decision-making variables produced three robust constructs, each with eigenvalues greater than 1 (24). The three factors were a danger to self (eigenvalue=3.24), a danger to others (eigenvalue=2.08), and a substantial inability to care for self (eigenvalue=1.37). Together these three factors accounted for 74.3 percent of the total variance within the data set. Danger to self accounted for 36 percent, danger to others for 23.1 percent, and substantial inability to care for self for 15.2 percent. Composite scores were created for each patient using the three factor scores generated by the factor analysis.
Multiple regression analyses of the effects of the three factor scores on the overall risk rating indicated that they accounted for 48 percent of the variance in that rating and were highly significant predictors of the overall risk rating. Analyses yielded beta values of .368 for danger to self (p< .001), .190 for danger to others (p< .003), and .406 for substantial inability to care for self (p<.001) (all beta weights were standardized). Logistic regression demonstrated that the overall risk rating significantly predicted the decision to detain (beta=1.50, p<.001).
Patient, clinician, and bed variables were then investigated in terms of their joint effects both on the overall risk rating (F=10.91, df=17.136, p< .001) and on the decision to detain (χ2=147.69, df=15, p<.001).
Patient variables
Danger to self (beta=.306, p<.001) and substantial inability to care for self (beta=.343, p<.001) were both highly significant predictors of the overall risk rating. However, once exogenous variables were controlled, danger to others was not a significant predictor.
In the logistic regression, the three factor scores were subsumed under the overall risk rating, which was a significant predictor of the decision to detain (beta=4.8, p<.004).
Clinician variables
Two clinician characteristics demonstrated differential effects in their ability to predict the overall risk rating and the decision to detain. The clinician's experience significantly predicted the overall risk rating (beta=.258, p<.001) but not the decision to detain. The clinician detention ratio did not predict the overall risk rating but did predict the decision to detain (beta=.395, p<.019). The evaluation setting—emergency service or mobile crisis unit—significantly predicted both the overall risk rating (beta=-.163, p<.02) and the decision to detain (beta=-4.95, p<.02).
Bed variables
The clinician's knowledge of the availability of voluntary private beds significantly predicted the overall risk rating (beta=-.159, p<.012). Knowledge of the availability of detention beds predicted the decision to detain (beta=4.12, p<.012).
Figure 1 illustrates the effects of patient, clinician, and bed variables. The results reported in Figure 1 did not substantially change in sign or significance when the ordinary least-squares and logistic regression estimates were corrected for heteroscedasticity and autocorrelation among patients who saw the same therapist. Three variables had results that may be sensitive to these adjustments. The availability of detention beds had only a marginally significant impact on reducing the probability of a decision to detain. The availability of voluntary private beds may have directly, and negatively, affected the decision to detain. The factor of danger to others may have directly, and positively, affected the decision to detain, while having a marginal positive effect on the overall risk rating. These results are qualified because the logistic regression did not converge when all of the independent variables shown in Figure 1 were simultaneously included in the model.
Discussion
The findings of this study suggest that, in contrast to a simple model in which clinicians make judgments using legal criteria alone, the decision-making process is influenced by multiple factors, such as the evaluation setting, the clinician's tendency to detain patients, and the availability of detention beds.
Danger to others
When the model was tested using only the three factor scores to predict the patient's overall risk rating, all three were significant predictors. Surprisingly, when the full model that included all the exogenous variables was tested, danger to others was no longer a significant predictor of the overall risk rating. Although this unexpected result bears further investigation, a likely explanation is the low variance in the ratings of danger to others among the patients in the sample (see Table 2).
Clinician characteristics
The clinician's role in evaluating an at-risk patient is complex. Clinicians typically consider the availability of patients' personal and professional support systems and community resources when making detention decisions. The results of this study suggest that qualities of the clinician may also play a role. Although experienced clinicians did not detain significantly more patients than less experienced clinicians, they did assess similar patients as being at higher risk than did less experienced clinicians. Clinicians appear to take risk factors more seriously the longer they practice, but they detain no more patients than less experienced clinicians.
The finding that the detention record of the clinician over the past three months was an indicator of the clinician's general tendency to detain patients at risk is of considerable interest. Staff worked varying amounts of time in the emergency service and on the mobile crisis unit, and patients seen on the mobile unit tended to require detention more often. Thus a system based on proportions was used to calculate the clinician detention ratio so that scores would not reflect differences in detention rates between the two settings but rather the differences in detention rates among staff.
The differences found suggest that even when all other factors are controlled, some clinicians have a greater tendency to detain patients than do others. One explanation of these findings is that clinicians' decisions are significantly and consistently affected by their personal attitudes about commitment, which are formed by multiple influences such as guidelines, past role models, effects of litigation, and personality.
Setting
The findings related to setting are of particular interest because mobile units are sometimes proposed as an effective mechanism for keeping patients out of the hospital. In this study, patients seen on the mobile crisis unit were significantly more likely to be detained than those seen in the emergency service, even when the clinician's rating of overall risk was controlled. Three factors may have played a role in increasing detention on the mobile unit. First, patients in this setting may have been unwilling to accept help. Second, assessments on the mobile crisis unit are often quite dramatic and involve high levels of emotion. Third, working on the mobile unit involves evening hours and working solo or with only one partner, factors that increase fatigue and stress and, perhaps, cautiousness (19,25). It appears that the conditions in which an assessment takes place may have unrecognized impact on clinicians' judgments.
Bed availability
The findings related to the availability of detention and voluntary hospital beds are tentative because the availability of beds was frequently unknown by the clinician. However, it is notable that even when the overall risk rating and all other patient and clinician variables were controlled, a patient had a significantly greater chance of being detained when detention beds were available, even though a police guard could be assigned to a patient when there were no free detention beds. This finding suggests that the impact of community resources on decision making and on the treatment of clients at risk deserves further exploration.
The meaning of the significant association between the availability of voluntary private beds and a low overall risk rating is unclear, and it may be best understood as a chance finding unless replicated by further study.
Conclusions
The findings of this research are preliminary, but the small sample of clinicians in one community mental health center has produced provocative data. Methodological and sampling limitations of this study make the results tentative. Further research is needed involving multiple sites and a more extensive evaluation of factors considered in assessments of patients in a mobile setting. However, the results of this initial research imply that decision making about involuntary commitment is a complex and multidetermined process.
The results support findings of previous research that clinicians do indeed make decisions according to legal criteria. However, evidence was also found that characteristics of the clinicians themselves may strongly influence the decision to detain. Moreover, clinicians' judgment may be affected by the setting in which they evaluate patients and the availability of detention beds. Additional research could provide insight into this important clinical process that has implications for appropriate care, patient rights, and the safety of both at-risk patients and the community.
Dr. Engleman is affiliated with the West Falls Psychotherapy Group, 7700 Leesburg Pike, Suite 200, Falls Church, Virginia 22043. Dr. Jobes is affiliated with the department of psychology at Catholic University of America in Washington, D.C. Dr. Berman is with the Washington Psychological Center in Washington, D.C. Dr. Langbein is with the department of public administration at American University in Washington, D.C.
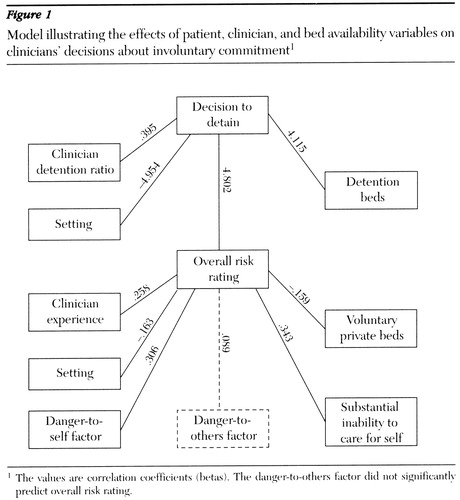
Figure 1. Model illustrating the effects of patient, clinician, and bed availability variables on clinicians' decisions about involuntary commitment1
1 The values are correlation coefficients (betas)The danger-to-others factor did not significantly predict overall risk rating.
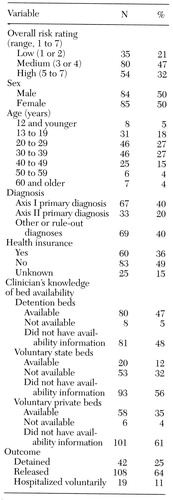 |
Table 1. Variables relevant to assessments of 169 patients being considered by clinicians for detention for involuntary commitment
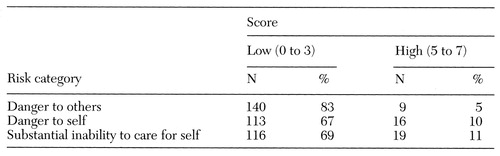 |
Table 2. Risk rating scores in three categories for 169 patients being considered by clinicians for detention for involuntary commitment
1. Appelbaum PS, Hamm RM: Decision to seek commitment. Archives of General Psychiatry 39:447-451, 1982Crossref, Medline, Google Scholar
2. Bagby RM, Thompson JS, Dickens SE, et al: Decision making in psychiatric civil commitment: an experimental analysis. American Journal of Psychiatry 148:28-33, 1991Link, Google Scholar
3. Faulkner LR, McFarland BH, Bloom JD: An empirical study of emergency commitment. American Journal of Psychiatry 146:182-186, 1989Link, Google Scholar
4. Lidz CW, Mulvey EP, Appelbaum PS, et al: Commitment: the consistency of clinicians and the use of legal standards. American Journal of Psychiatry 146:176-181, 1989Link, Google Scholar
5. McCready M, Merskey H: On the recording of mental illness for civil commitment. Canadian Journal of Psychiatry 27:140-143, 1982Crossref, Medline, Google Scholar
6. Miller RD, Fiddleman PB: The adequacy of commitment evaluations performed by psychiatric and non-psychiatric physicians. Journal of Psychiatry and Law 10:45-56, 1982Crossref, Google Scholar
7. Page S, Firth J: Civil commitment practices in 1977: troubled semantics and troubled psychiatry. Canadian Journal of Psychiatry 24:329-334, 1979Crossref, Google Scholar
8. Schwartz HI, Appelbaum PS, Kaplan RD: Clinical judgments in the decision to commit: psychiatric discretion and the law. Archives of General Psychiatry 41:811-815, 1984Crossref, Medline, Google Scholar
9. Segal SP, Watson MA, Nelson S: Consistency in the application of civil commitment standards in the psychiatric emergency room. Journal of Psychiatry and Law 14:125-146, 1986Crossref, Google Scholar
10. Segal SP, Watson MA, Goldfinger SM, et al: Civil commitment in the psychiatric emergency room: I. the assessment of dangerousness by emergency room clinicians. Archives of General Psychiatry 45:748-752, 1988Crossref, Medline, Google Scholar
11. Segal SP, Watson MA, Goldfinger SM, et al: Civil commitment in the psychiatric emergency room: II. mental disorder indicators and three dangerousness criteria. Archives of General Psychiatry 45:753-758, 1988Crossref, Medline, Google Scholar
12. Segal SP, Watson MA, Goldfinger SM, et al: Civil commitment in the psychiatric emergency room: III. disposition as a function of mental disorder and dangerousness indicators. Archives of General Psychiatry 45:759-763, 1988Crossref, Medline, Google Scholar
13. Thompson JS, Ager JW: An experimental analysis of the civil commitment recommendations of psychologists and psychiatrists. Behavioral Sciences and the Law 6:119-129, 1988Crossref, Google Scholar
14. Bagby RM, Thompson JS, Dickens SE, et al: Decision making in psychiatric civil commitment: an experimental analysis. American Journal of Psychiatry 148:28-33, 1991Link, Google Scholar
15. Hiday VA: Civil commitment: a review of empirical research. Behavioral Sciences and the Law 6:15-44, 1988Crossref, Google Scholar
16. Nicholson RA: Correlates of commitment status in psychiatric patients. Psychological Bulletin 100:241-250, 1986Crossref, Medline, Google Scholar
17. Affleck GG, Peszke MA, Wintrob RM: Psychiatrists' familiarity with legal statutes governing emergency involuntary hospitalization. American Journal of Psychiatry 135:205-209, 1978Link, Google Scholar
18. Anderson JA, Eppard J: Clinical decision making during assessment for involuntary psychiatric admission. Psychiatric Services 46:727-728, 1995Link, Google Scholar
19. Rissmiller DJ, Hogate PM, August D, et al: Commitment decisions: identification of indeterminate cases. Crisis 15:110-115, 1994Medline, Google Scholar
20. Meyerson AT, Moss JZ, Belville R, et al: Influence of experience on major clinical decisions. Archives of General Psychiatry 36:423-427, 1979Crossref, Medline, Google Scholar
21. Anderson J, Eppard J: Clinical decision making during assessment for involuntary psychiatric admission. Psychiatric Services 46:727-728, 1995Link, Google Scholar
22. Engleman NB: Involuntary commitment: an investigation of the clinician's decision-making process. Doctoral dissertation. Washington, DC, American University, Department of Psychology, 1990Google Scholar
23. McIver JP, Carmines EG: Unidimensional scaling, in Sage University Paper Series on Quantitative Applications in the Social Sciences. Edited by Sullivan JL. Beverly Hills, Calif, Sage, 1981Google Scholar
24. Kim J, Mueller CW: Factor analysis: statistical methods and practical issues, in Sage University Paper Series on Quantitative Applications in the Social Sciences. Edited by Sullivan JL. Beverly Hills, Calif, Sage, 1978Google Scholar
25. Mendel WM, Rapport S: Determinants of the decision for psychiatric hospitalization. Archives of General Psychiatry 20:321-328, 1969Crossref, Medline, Google Scholar



