Outcome for People With Schizophrenia Before and After Medicaid Capitation at a Community Agency in Colorado
Abstract
OBJECTIVE: To investigate the effect of a capitated funding mechanism for the psychiatric care of Medicaid recipients, a study of outcome, satisfaction, and service utilization among adults with schizophrenia and schizoaffective disorder was conducted at a Colorado agency before and after the introduction of the new funding mechanism. METHODS: Two random samples of 100 clients each were selected, one a year before capitation was introduced and one a year after. Subjects were interviewed about their quality of life, needs, and service satisfaction. Psychopathology and service utilization were also measured. RESULTS: Psychopathology was lower after capitation in most dimensions. The number of subjects admitted to the hospital during a six-month period beginning a year after capitation was 57 percent lower than in the equivalent period before capitation, with no increase in the amount of outpatient treatment provided. Subjects reported improved quality of life in the domains of work, finances, and social relations. Significant changes in needs or service satisfaction were not detected. CONCLUSIONS: No evidence was found that Medicaid capitation had an adverse effect on the client population after one year. Findings suggested that capitation led to an efficient use of treatment resources.
According to a 1996 Bazelon Center report, 43 states had obtained waivers of federal Medicaid rules that allowed innovative approaches to funding medical or psychiatric services, or both (1). Colorado was among those states—one of ten in which the waiver applied only to psychiatric care. On August 1, 1995, a capitated funding mechanism for psychiatric services for Medicaid recipients was initiated in much of Colorado. Under this mechanism, instead of billing for every service provided, agencies receive a predetermined amount for each Medicaid recipient in the catchment area.
Capitated funding creates incentives for agencies to develop cost-effective treatment approaches for Medicaid recipients and allows savings to be used for clients, programs, and other purposes. Proponents argue that it makes possible treatment methods that were not funded under fee-for-service arrangements (2) and promotes more cost-effective (3), client-centered, flexible, timely, and community-based treatment (4). Others, however, are concerned that new financial incentives could lead to reduced service quality and worse outcome for seriously disturbed clients (5,6).
This issue is becoming important for hundreds of thousands of psychiatrically disturbed Medicaid recipients across America, but as yet little information is available to address it. An early small-scale capitation study in Washington, D.C., demonstrated reduced hospitalization but no overall decrease in service utilization for seriously mentally ill patients (7). A capitation experiment for severely mentally ill adults in New York State demonstrated reduced hospital use and lower treatment costs but no difference in functioning or symptomatology (8,9). A California study produced similar results, although it was not clear whether benefits were due to capitated funding, assertive community treatment, or higher funding (10).
To further investigate the effect of capitation, a study of quality of life, needs, satisfaction with services, psychopathology, and service utilization of highly vulnerable clients—adults with schizophrenia and schizoaffective disorder—was conducted at the Mental Health Center of Boulder County, Colorado, before and after the introduction of capitation. The purpose of the study was to determine whether vulnerable patients with serious mental illness suffered adverse consequences after the switch to capitation. A before-and-after study design was used with random samples drawn in an identical fashion at each time.
Background
The Mental Health Center of Boulder County
The center is a nonprofit agency providing inpatient and outpatient services for children and adults in a mixed urban and rural catchment area of 250,000 people. The agency serves about 3,000 clients at any time, more than 600 of whom are adults with psychosis. Approximately half the adult clients with psychosis receive Medicaid; the remainder have Medicare or private insurance or are not insured.
Even before the introduction of capitation on August 1, 1995, the agency operated an extensive community support system for adults (11) with subsidized and supported housing, a sheltered workshop where about 55 to 60 clients worked part time, and a clubhouse that maintained around 35 supported employment placements. When necessary, patients were assigned to assertive community treatment teams with small caseloads that provided daily contact, case management, medication monitoring, and money management. Qualified patients were enrolled in appropriate benefit programs.
The use of adult acute psychiatric hospital beds was already low before capitation, averaging around four patients in private general hospital beds and eight in the state hospital at any given time, a total of five per 100,000 population. Treatment in both public and private hospitals was provided by the center's own psychiatrists. Hospital utilization was kept low through the use of Cedar House, the center's open-door, 15-bed hospital alternative for acute treatment (12).
The capitation pilot project
The Boulder capitation pilot project is notable in that the agency developed its own utilization and quality control mechanisms and did not contract with an established managed care entity. Therefore, all savings were available for reinvestment in treatment programs. Utilization management was made easier by the fact that few external, private-sector providers served Medicaid clients before capitation. In the first year of capitation, three nonprofit hospitals and 30 individual external providers contracted with the agency to provide services. Few clients chose treatment with external providers.
A protocol for determining appropriate duration of outpatient utilization based on diagnosis and illness severity was developed but found unnecessary. Utilization of services provided by external providers was monitored on a case-by-case basis by senior clinical staff. Utilization of outpatient treatment provided by center staff was managed by supervision of therapists. Inpatient utilization was managed by preadmission assessment by emergency staff and psychiatrists, daily review, and weekly group review of all inpatients.
New services
Several service innovations for adult clients at the Mental Health Center of Boulder County resulted from the introduction of capitation.
• Family care. A new program of long-term care with foster families admitted four clients in the first year of capitation.
• Crisis-respite homes. Acutely disturbed clients were treated in a new short-term foster home program by a mobile psychiatric team (13). In the first year, 29 clients were treated.• Hospital diversion. The use of adult psychiatric hospital beds in general hospitals was reduced from an average of four a day to two a day through increased use of hospital alternatives.• A mobile treatment team. A team of 1.75 full-time-equivalent employees was developed for seriously disturbed patients whose functioning was less compromised than clients of the assertive community treatment team but who were unlikely to do well in office-based treatment because of marginal compliance and irregular attendance. In the first year, 50 patients were treated by the mobile team.• Increased case management. Case management staffing for the long-term residential program, the job development program, and other special programs was increased by 15 percent. Eight new full-time employees were added to the existing staff of 53 in these programs. Several of the new programs provided services that were not billable under fee-for-service Medicaid.
Medicaid recipients and those with other health insurance received identical treatment except that when admission to a hospital alternative was not feasible, Medicaid recipients were admitted to the state hospital rather than a private hospital.
Access improved with capitation. Fourteen percent of county Medicaid recipients received services in the year before capitation was implemented, and 17 percent in the year after capitation.
Financial effects of capitation
The center's budget for the year preceding capitation was $15.3 million. (State and federal funding, including Medicaid and Medicare, totaled $7.8 million.) In the first year of capitation, the center received 95 percent of the previous year's Medicaid reimbursement plus a 3 percent increase for inflation. In addition, the agency became the fundholder for previous private-provider expenditures of approximately $1.5 million for inpatient care and $300,000 for outpatient treatment. The budget for the first year of capitation was $17.8 million.
In the first year of capitation, expenditures for services from external providers amounted to only $25,000 for inpatient care and $16,000 for outpatient care. Intensive outpatient treatment resulted in savings of more than $1 million on child and adolescent inpatient care. Savings on adult hospital care were less substantial, because inpatient care for adults was already limited. Costs for new programs and utilization management were more than offset by reduced expenditures. Expenses in the first year of capitation increased by $830,000, but revenues exceeded expenditures by $2 million, allowing savings to be used for debt retirement, capital purchases, and capital reserves. Savings of $165,000 were used for increased services for indigent patients.
Methods
In the summer of 1994, one year before Medicaid capitation was introduced, people with schizophrenia and schizoaffective disorder between the ages of 18 and 50 were randomly selected from among open cases at the Mental Health Center of Boulder County. They ranged from severely disturbed clients, including a few in long-term hospital care, to some in full-time employment. Non-English-speaking clients were excluded. Clients was asked to consent until 100 agreed to be interviewed.
The same sampling procedure was followed in the summer of 1996, one year after the start of Medicaid capitation. New random samples were drawn on each occasion to avoid bias due to improvement over time, which is inherent in following the same cohort. At each time, the sample represented approximately 40 percent of the total patient pool. Forty-four of the clients interviewed in 1996 were also interviewed in 1994.
Subjects who consented were interviewed using the Lancashire Quality of Life Profile (LQOLP) developed by Oliver and coworkers (14), which is a structured interview based on Lehman's work (15); a needs-assessment instrument modified from the Camberwell Assessment of Need (16); and a questionnaire about satisfaction with services that has been used throughout the Colorado system for years. The first two instruments are guided self-reports, and the third is entirely self-report, so interrater reliability tests were not indicated.
The LQOLP includes subjective satisfaction ratings and objective questions in nine life domains, including employment, income, housing, and social and family relations. Satisfaction in each domain is recorded with 7-point Likert scales. The needs assessment instrument inquires about 16 needs, from living accommodations to sexual life. Respondents report who provides help in each area and satisfaction with and importance of the help. Interviews were conducted by independent trained interviewers, the majority of whom were mental health consumers.
Subjects' psychopathology was rated by psychiatrists using the Brief Psychiatric Rating Scale—Expanded Version (BPRS) (17). Psychiatrists were trained to use the BPRS in two training sessions; interrater reliability tests were not performed. Subjects were diagnosed by psychiatrists using DSM-IV criteria. Information about medications used in 1994 and 1996 was gathered from clinical records. Information on inpatient and outpatient treatment was obtained from the administrative database, which used an identical method in 1994 and in 1996 to record treatment contacts.
Differences between samples were tested using chi square or t tests. To reduce error due to multiple tests, Bonferroni limits were applied separately to measures of quality of life, needs assessment, and satisfaction, and psychopathology ratings were reduced to five dimensions.
Results
Sample
Before a sample of 100 consenting subjects was achieved, 36 patients refused to be interviewed in 1994 and 25 in 1996. In 1994 fewer refusers than consenters had been hospitalized in the previous six months (6 percent versus 21 percent; 2=4.08, df=1, p=.043), and refusers had received less outpatient service than consenters in that time period (83.8 units versus 186.5 units; t=3.22, df=76, p=.002). In 1996 no significant differences were found between refusers and consenters.
Table 1 summarizes data on the characteristics of the 1994 and 1996 samples. No significant differences in demographic or clinical measures were found between the samples. Forty-nine percent of the 1994 sample and 61 percent of the 1996 sample were Medicaid recipients.
Quality of life
Table 2 lists some measures of quality of life and psychopathology for the 1994 and 1996 samples. All significant differences indicated greater quality of life for the 1996 sample.
In 1996 more patients had worked continuously for two years, but the difference was not significant using the Bonferroni correction. Between 1994 and 1996, the average number of months worked among working subjects increased 60 percent, a significant change. Income from such ancillary sources as food stamps was significantly greater in 1996, and fewer patients reported they lacked money to enjoy life.
In 1996 the time patients spent in their current living accommodation increased 25 percent, and all measures of satisfaction with accommodations were greater than in 1994, although the differences were not significant.
In 1996 more subjects reported having a friend on whom they could rely for help, but this difference was not significant using the Bonferroni correction.
Psychopathology and treatment utilization
The mean total psychopathology score on the BPRS was 11.5 percent lower in 1996, and scores for positive symptoms as well as manic and depressive symptoms were lower. A similar decrease in score (10.2 percent) was noted for the 44 subjects interviewed at both times.
The number of patients admitted to the hospital in the six months from July to December was 57 percent lower in 1996 than in 1994. The number of units of outpatient treatment provided over the same six-month period was 19 percent lower in 1996 than two years earlier.
Medication
In 1996 a total of 34 of the 100 subjects were taking novel antipsychotics. Two years earlier 14 of these 34 patients were taking standard antipsychotics, 15 were taking novel antipsychotics, and six were not taking medication. Of the 44 patients who were included in both the pre- and postcapitation samples, ten had switched between 1994 and 1996 from standard to novel antipsychotics, 24 were taking standard drugs at both times, and nine were taking novel drugs at both times. Three were taking no medication at one time or the other.
Patients who switched from standard to novel drugs showed a greater improvement in total psychopathology score (17.2 percent improvement) between 1994 and 1996 than those who remained on the same type of medication, novel or standard, at each time (7.5 percent improvement). However, this difference was not significant in a multivariate analysis of variance. Rates of hospital admission and outpatient service utilization were not reduced more among those who switched from standard to novel drugs, compared with those who remained on the same type of medication. Nor was switching to novel drugs associated with greater improvements in work hours or duration of employment.
Needs
More 1996 subjects reported a problem with finances, but this difference was not significant using the Bonferroni correction. Critical needs—that is, those that were both frequent and important—were the same for both samples. These needs were in the areas of psychological problems, health, finances, budgeting, obtaining information about illness, transportation, and food.
Satisfaction with services
No significant differences were found between the two samples in satisfaction with services. However, a trend toward lower satisfaction in several areas was noted in 1996.
Discussion
Limitations of the study
One year before the introduction of Medicaid capitation and one year after, we measured quality of life, needs, satisfaction with treatment, psychopathology, and utilization of treatment among clients of a mental health center who had schizophrenia and schizoaffective disorder. However, we cannot directly attribute any changes to capitated funding, because unrelated events may have affected the patient population.
Clients in the precapitation sample who refused to be interviewed appeared less disturbed than those who consented, a difference not evident in the postcapitation sample. The precapitation selection bias could have made it easier to demonstrate improvements with capitation. However, no significant differences were found between the pre- and postcapitation samples in demographic characteristics or age at first hospitalization. Furthermore, analysis of the data for the 44 patients who were included in both pre- and postcapitation samples indicates that all significant differences in the full sample were evident to a similar degree in this subsample.
A further limitation of the study is that the researchers were not independent of the agency providing the capitated services.
Service use and psychopathology
The number of Medicaid recipients in the 1996 sample was 24 percent greater than in 1994, suggesting that capitation did not lead to severely ill Medicaid recipients' being rejected in favor of fee-for-service clients. Over a six-month period, 19 percent fewer treatment contacts were recorded for the 1996 sample than for the 1994 sample. Treatment contacts may have actually declined or contacts may have been less adequately recorded under capitation because such records were no longer needed for billing. In addition, some services that were counted as multiple contacts in 1994 may have been "bundled" into single units in 1996.
Total psychopathology was lower in 1996, due to reductions in positive, manic, and depressive symptoms. The number of subjects admitted to the hospital in the last six months of 1996 was 57 percent lower than in the same period of 1994, despite the apparent reduction in outpatient treatment in 1996. Four patients in the 1996 sample were treated in crisis homes as an alternative to the hospital. Although hospital care was already very limited before capitation was introduced, reductions in hospitalization were possible with capitation, which is similar to experience elsewhere (18,19).
Did increased use of novel antipsychotics contribute to improved outcome? More than 40 percent of subjects taking novel antipsychotics in 1996 were using standard antipsychotic medication two years earlier, and psychopathology decreased more among patients who switched from standard to novel medication. However, because outpatient service utilization, hospitalization, and employment were unaffected by the switch to novel drugs, it seems unlikely that the novel drugs were a major factor in producing the broad array of improvements noted.
Quality of life
After capitation, subjects reported greater quality of life in several domains, particularly work and finances. The number in sustained employment was three times greater in 1996, and the average duration of work was more than double. The strength of the local labor market may have helped. Between 1994 and 1996 the Boulder unemployment rate decreased from 4.3 percent to 3.3 percent. The increase in sustained employment may also have been due to growth of the mental health center's supported employment program, which expanded from 35 patients in supported employment in 1994 to 55 in 1996. Of the 19 patients in the 1996 sample who were employed continuously for two years, approximately equal numbers were in sheltered, supported, or independent employment. Sustained employment may also have increased secondary to improvements in stability of illness and community tenure.
More subjects in 1996 reported having a friend to rely on for help. Previous research has indicated that this measure improves with clubhouse involvement (Huxley P, Warner R, unpublished manuscript, 1996), and this finding may be related to an observed increase in clubhouse attendance in the sample.
The average duration of stay in current living accommodations increased from three years to four between 1994 and 1996. The improvement may have been due to improved stability of illness, or to the stabilizing effect of rent subsidies, which are usually tied to specific accommodations. Between 1994 and 1996, the number of subsidized rent certificates managed by the mental health center increased by a third because of increased residential program staffing. Forty-six percent of the 1996 sample had a rent subsidy. No subjects were in the newly established long-term foster family care program.
Fewer 1996 subjects reported that they lacked money to enjoy life, presumably because average income increased and more subjects had rent subsidies. Expanded case management activity probably helped increase peripheral income from food stamps and other sources.
Needs
Modest decreases were found in the frequency of nearly all the needs reported to be frequent and important, including health, finances, budgeting, and food. Increased case management may have helped address these needs. Housing was not noted to be a prominent need, perhaps because of ready access to subsidized housing.
Satisfaction with services
Satisfaction with services declined slightly between 1994 and 1996. Researchers in the area of quality of life often find that satisfaction ratings do not follow indicators of objective circumstances (20,21; Warner R, unpublished manuscript, 1997). Lehman (22) noted that positive change may produce transient decreases in satisfaction because of renewed awareness of how life could be better. In this study, clients with a high risk of relapse may have been expressing dissatisfaction with closer monitoring.
Conclusions
No evidence was found to indicate that Medicaid capitation had significant adverse effects on this client population after one year. The proportion of people in treatment for schizophrenia who were Medicaid recipients was greater after capitation. All the significant changes were positive, with improvements in psychopathology, hospitalization rate, sustained employment, and income, although these changes may have been unrelated to the introduction of capitation. Findings suggested that capitation led to efficient resource utilization because positive changes occurred with no increase in outpatient treatment and with a reduction in inpatient care.
The experience may not be as easily repeated elsewhere. The Mental Health Center of Boulder County enjoyed certain advantages entering capitation. The local private sector provided few services to Medicaid clients. The agency already focused resources on high-risk clients, having developed a community support system with hospital alternatives and a variety of housing options, which helped limit hospitalization. Inpatient care and outpatient care were integrated by using agency staff and psychiatrists to provide care at private and public hospitals. The agency established its own utilization management protocol and did not enter an expensive contract with a managed care provider.
Agencies planning a capitation pilot project may wish to foster the development of similar elements before accepting financial risk.
Dr. Warner is medical director of the Mental Health Center of Boulder County, 1333 Iris Avenue, Boulder, Colorado 80304 (e-mail, [email protected]). He is also clinical professor in the department of psychiatry at the University of Colorado in Denver and Boulder. Dr. Huxley is professor of psychiatric social work in the department of psychiatry at Manchester University in Manchester, England.
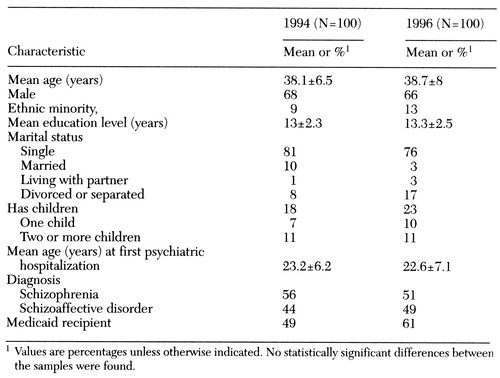 |
Table 1. Characteristics of the random samples of patients with schizophrenia and schizoaffective disorder a year before and a year after implementation of capitation in Boulder
1 Values are percentages unless otherwise indicatedNo statistically significant differences between the samples were found.
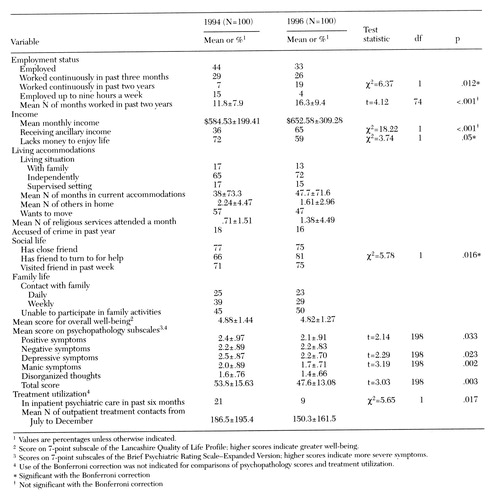 |
Table 2. Quality of life, psychopathology, and treatment utilization among samples of patients with schizophrenia and schizoaffective disorder a year before and after implementation of capitation in Boulder
1 Values are percentages unless otherwise indicated
2 Score on 7-point subscale of the Lancashire Quality of Life Profile; higher scores indicate greater well-being.
3 Scores on 7-point subscales of the Brief Psychiatric Rating Scale-Expanded Version; higher scores indicate more severe symptoms.
4 Use of the Bonferroni correction was not indicated for comparisons of psychopathology scores and treatment utilization.
* Significant with the Bonferroni correction
† Not significant with the Bonferroni correction
1. Managed Mental Health Care: Survey of the States. Washington, DC, Bazelon Center for Mental Health Care, 1996Google Scholar
2. Warner R: Deinstitutionalization: how did we get where we are? Journal of Social Issues 45:17-30, 1989Google Scholar
3. Yank GR, Hargrove DS, Davis KE: Toward the financial integration of public mental health services. Community Mental Health Journal 28:97-109, 1992Crossref, Medline, Google Scholar
4. Godshalx S: Advantages of working in a capitated mental health system. Psychiatric Services 47:477-478, 1996Link, Google Scholar
5. Lehman AF: Capitation payment and mental health care: a review of the opportunities and risks. Hospital and Community Psychiatry 38:31-38, 1987Abstract, Google Scholar
6. McFarland B: Health maintenance organizations and persons with severe mental illness. Community Mental Health Journal 30:221-242, 1994Crossref, Medline, Google Scholar
7. Harris M, Bergman H: Capitation financing for the chronic mentally ill: a case management approach. Hospital and Community Psychiatry 39:68-72, 1988Abstract, Google Scholar
8. Cole RE, Reed SK, Babigian HM, et al: A mental health capitation program: I. patient outcomes. Hospital and Community Psychiatry 45:1090-1096, 1994Abstract, Google Scholar
9. Reed SK, Hennessy K, Mitchell OS, et al: A mental health capitation program: II. cost-benefit analysis. Hospital and Community Psychiatry 45:1097-1103, 1994Abstract, Google Scholar
10. Chandler D, Meisel MBA, McGowen M, et al: Client outcomes in two model capitated integrated service agencies. Psychiatric Services 47:175-180, 1996Link, Google Scholar
11. Mosher LR, Burti LR: Community Mental Health: Principles and Practice. New York, Norton, 1989Google Scholar
12. Warner R, Wollesen C: Cedar House: a non-coercive hospital alternative in Boulder, Colorado, in Alternatives to the Hospital for Acute Psychiatric Treatment. Edited by Warner R. Washington, DC, American Psychiatric Press, 1995Google Scholar
13. Bennett R: The Crisis Home Program of Dane County, ibidGoogle Scholar
14. Oliver J, Huxley P, Bridges K, et al: Quality of Life and Mental Health Services. London, Routledge, 1996Google Scholar
15. Lehman AF: The well-being of chronic mental patients: assessing their quality of life. Archives of General Psychiatry 40:369-73, 1983Crossref, Medline, Google Scholar
16. Thornicroft G, Brewin C, Wing J: Measuring Mental Health Needs. London, Royal College of Psychiatrists, 1992Google Scholar
17. Ventura J, Lukoff D, Nuechterlein KH, et al: Training and quality assurance with the BPRS. International Journal of Methods in Psychiatric Research 3:221-224, 1993Google Scholar
18. Christianson JB, Gray DZ: What CMHCs can learn from two states' efforts to capitate Medicaid benefits. Hospital and Community Psychiatry 45:777-781, 1994Abstract, Google Scholar
19. Cuffel BJ, Wait D, Head T: Shifting the responsibility for payment for state hospital services to community mental health agencies. Hospital and Community Psychiatry 45:460-465, 1994Abstract, Google Scholar
20. Rohland BM, Rohrer JE: Evaluation of managed mental health care for Medicaid enrollees in Iowa. Psychiatric Services 47:1185-1187, 1996Link, Google Scholar
21. Warner R, de Girolamo G, Fioritti A, et al: The quality of life of people with schizophrenia in Boulder, Colorado, and Bologna, Italy. Schizophrenia Bulletin, in pressGoogle Scholar
22. Lehman AF: Measures of quality of life among persons with severe and persistent mental disorders, in Mental Health Outcome Measures. Edited by Thornicroft G, Tansella M. Berlin, Springer, 1996Google Scholar



