Global Functioning of Inpatients With Obsessive-Compulsive Disorder, Schizophrenia, and Major Depression
Abstract
A chart review was conducted to compare the social, occupational, and daily functioning of 17 inpatients with obsessive-compulsive disorder, 17 with major depression, and 17 with schizophrenia. Current Global Assessment of Functioning (GAF) scores of patients with schizophrenia were significantly lower than those of patients with depression and with obsessive-compulsive disorder. However, on work performance, daily living skills, and past-year GAF scores, patients with obsessive-compulsive disorder and those with schizophrenia did not differ significantly, and both groups were significantly more impaired than patients with depression. Results show that inpatients with obsessive-compulsive disorder may exhibit severe and chronic functional impairments requiring extensive supportive and rehabilitative services.
Although several studies have focused on employment and educational status (1,2), role performance, and social functioning (3) of outpatients and community samples of patients (4) with obsessive-compulsive disorder, recent studies that examine basic aspects of functioning in more severe cases of the disorder are lacking. Because obsessive-compulsive symptoms may be profoundly disabling (5,6,7), such studies are critical to our understanding of the disorder and to the provision of useful services for those with severe symptoms.
We undertook a retrospective chart review to assess the severity of impairments in social and occupational functioning and daily living skills among inpatients with obsessive-compulsive disorder, schizophrenia, and major depression. We hypothesized that inpatients with obsessive-compulsive disorder and those with schizophrenia would be more impaired than inpatients with depression. We also hypothesized that inpatients with schizophrenia and those with obsessive-compulsive disorder would not differ significantly on most measures of functioning.
Methods
By simple random sampling, we selected records of 51 inpatients, 17 each with primary DSM-III-R diagnoses of schizophrenia, major depression, and obsessive-compulsive disorder. Patients were diagnosed by their primary clinicians in consultation with the attending physician and treatment team. Patients with a diagnosis of major depression were eight women and nine men with a mean±SD age of 41.2±9.9 years. Those with a diagnosis of obsessive-compulsive disorder were three women and 14 men with a mean±SD age of 31.9±9.4 years. Patients with schizophrenia were eight women and nine men with a mean age of 30.4±9.3 years.
All patients were hospitalized between 1990 and 1993 at the Connecticut Mental Health Center. Patients with depression and obsessive-compulsive disorder were admitted to the clinical neuroscience research unit, and those with schizophrenia to the division of inpatient services.
By review of admission and discharge summaries and clinicians' notes, one of the authors (DL) collected data, shown in Table 1, on each patient's employment history, time lost from work over the past year, financial support, and contact with relatives during the year before admission. The quality of contact with family and friends, defined as the degree of emotional closeness reported by the patient or a significant other, was also assessed. The patient's ability to perform activities of daily living was evaluated based on the patient's self-report and staff observation. Global Assessment of Functioning (GAF) scores, rated on admission by the primary clinician, were also obtained.
Depending on the scale of measurement in each case, we used analysis of variance (ANOVA), Kruskal-Wallis ANOVA, or chi square tests to assess differences among patients by diagnosis. If the findings were significant, we made comparisons between the groups using two-tailed t tests, Mann-Whitney U tests, or Fisher's exact tests, as appropriate.
Results
Kruskal-Wallis ANOVA revealed a significant difference among diagnostic groups in employment history (H= 12.21, df=2, p<.002, N=46). Post hoc Mann-Whitney U tests demonstrated no significant difference between patients with schizophrenia and obsessive-compulsive disorder (z=-.06, p<.95, N=31). However, depressed patients' employment histories were significantly superior to those of patients with schizophrenia (z=-3.18, p<.002, N=31) and obsessive-compulsive disorder (z=-2.87, p<.004, N=30).
The groups differed significantly in time lost from work over the past year (H=13.80, df=2, p<.001, N=44). However, patients with schizophrenia did not differ significantly from those with obsessive-compulsive disorder in time lost from work (z=-1.67, p<.09, N=28), whereas depressed patients lost significantly less time from work than those with schizophrenia (z=-3.40, p<.001, N=27) and obsessive-compulsive disorder (z=-2.45, p<.01, N=33).
A significant difference was also found among patient groups in source of income (χ2=7.38, df=2, p<.025). Fisher's exact test showed no difference between those with schizophrenia and those with obsessive-compulsive disorder; however, significantly more patients with depression were supporting themselves than patients with schizophrenia (p<.039, df=1, N=33). Similarly, more patients with depression than with obsessive-compulsive disorder were self-supporting, but the difference between these groups was not significant.
Differences among the groups in the amount of contact and the quality of relationships with their families did not reach significance. However, the quality of the friendships of depressed patients was significantly better than the quality of the friendships of patients with obsessive-compulsive disorder (z=-2.35, p<.02, N=29) and patients with schizophrenia (z= -3.03, p<.002, N=27). The quality of friendships of patients with obsessive-compulsive disorder and of those with schizophrenia did not differ.
We also found a significant difference among groups in the ability to perform activities of daily living (H=26.70, df=2,49, p<.001, N=51). Again, although no difference was noted between patients with schizophrenia and those with obsessive-compulsive disorder, depressed patients had significantly less difficulty with activities of daily living than those with schizophrenia (z=-4.68, p<.001, N=34) and obsessive-compulsive disorder (z=-4.23, p<.001, N=34).
The mean±SD current GAF score for the 17 depressed patients was 40.9±11.2; for 13 patients for whom data were available, the highest mean score for the past year was 60.4± 14.4. The mean current GAF score for 16 patients with obsessive-compulsive disorder was 40.5±13.5; the highest mean score for the past year was 47.3±14.4 for 12 patients with available data. The mean current score for 15 patients with schizophrenia was 29.7±3.5; the highest mean GAF score in the past year was 40.8±5 for the eight patients with available data. ANOVA demonstrated significant differences among the three groups on current-year GAF scores (F=5.76, df=2,45, p<.006) and past-year GAF scores (F=6.54, df=2,30, p<.004).
Current GAF scores of patients with schizophrenia were significantly lower than those of patients with obsessive-compulsive disorder (t=3.11, df=17, p<.006) and with depression (t=3.91, df=19, p<.001). Current GAF scores of patients with obsessive-compulsive disorder and depression did not differ. However, GAF scores of depressed patients for the past year were significantly higher than those of patients with obsessive-compulsive disorder (t=2.27, df=23, p<.033) and with schizophrenia (t=4.51, df=16, p< .001). No significant difference in past-year GAF scores was found between patients with schizophrenia and obsessive-compulsive disorder.
Discussion
In this study, inpatients with obsessive-compulsive disorder were found to have more functional impairments than those with major depression and to differ little from inpatients with schizophrenia on most functional measures. These preliminary findings, although compelling, are tentative. The small sample size limited the study's statistical power and ability to control for comorbid diagnoses. In addition, retrospective data collection from charts of multiple clinicians may produce measurement error, and the use of multiple univariate tests increases the risk of an incorrect finding of significant difference between groups. A larger, prospective study of age- and sex-matched subjects that uses standardized instruments administered by blind raters and that analyzes the data by multivariate statistics is needed to confirm the hypotheses.
Although the findings cannot be generalized to the entire range of patients with obsessive-compulsive disorder, they do underscore the severe impairments of an often-overlooked subset of obsessive-compulsive patients. Among these patients, poor concentration and the need to engage in compulsive, repetitive behaviors may significantly hamper work performance. Social relationships frequently suffer due to the overriding focus on completion of rituals, and the ability to attend to personal hygiene, eat, dress, perform household chores, manage money, and use the telephone are also often compromised. Supported housing, structured day programs, and rehabilitative services with a behavioral-therapy orientation may enhance functioning.
Acknowledgments
This work was partly supported by grants MH25642, MH30929, and MH36229 from the National Institute of Mental Health, by a Stanley Foundation research award to Dr. Price, and by the Connecticut Department of Public Health and Addiction Services.
Ms. Calvocoressi is affiliated with the departments of psychiatry and epidemiology and public health at Yale University School of Medicine. Ms. Libman is with the Milford (Conn.) Mental Health Clinic. Ms. Vegso is affiliated with the clinical neuroscience research unit in the department of psychiatry at Yale University. Dr. McDougle is with the department of psychiatry at Indiana University. Dr. Price is with Butler Hospital and the department of psychiatry and human behavior at Brown University School of Medicine, 345 Blackstone Boulevard, Providence, Rhode Island 02906. Send correspondence to Dr. Price.
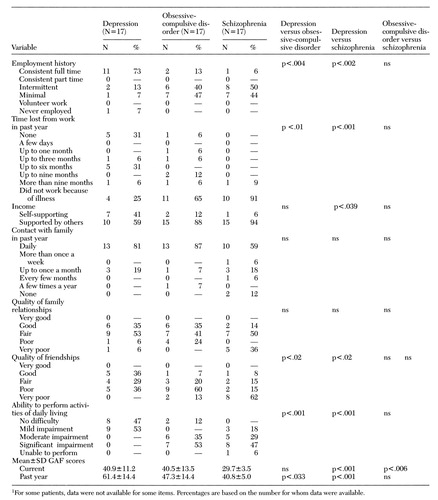 |
Table 1. Occupational and social functioning and ability to perform activities of daily living of inpatients with depression, obsessive-compulsive disorder, and schizophrenia1
1. Steketee G, Grayson JB, Foa EB: A comparison of characteristics of obsessive-compulsive disorder and other anxiety disorders. Journal of Anxiety Disorders 1:325-335, 1987Crossref, Google Scholar
2. Gojer J, Khanna S, Channabasavanna SM: Obsessive-compulsive disorder, anxiety, and depression. Indian Journal of Psychological Medicine 10:25-30, 1987Google Scholar
3. Koran LM, Thienemann ML, Davenport R: Quality of life for patients with obsessive-compulsive disorder. American Journal of Psychiatry 153:783-788, 1996Link, Google Scholar
4. Karno M, Golding JM, Sorenson SB, et al: The epidemiology of obsessive-compulsive disorder in five US communities. Archives of General Psychiatry 45:1094-1099, 1988Crossref, Medline, Google Scholar
5. Calvocoressi L, McDougle CJ, Wasylink S, et al: Inpatient treatment of patients with severe obsessive-compulsive disorder. Hospital and Community Psychiatry 44:1150-1154, 1993Abstract, Google Scholar
6. Rachman SJ, Hodgson RJ: Obsessions and Compulsions. Englewood Cliffs, NJ, Prentice-Hall, 1980Google Scholar
7. Perse T: Obsessive-compulsive disorder: a treatment review. Journal of Clinical Psychiatry 49:48-55, 1988Medline, Google Scholar



