Effect of Staff Debriefing on Posttraumatic Stress Symptoms After Assaults by Community Housing Residents
Abstract
OBJECTIVE: The study examined the efficacy of critical incident stress debriefing in ameliorating the impact of posttraumatic stress on direct care psychiatric workers after a traumatic event at work. METHODS: Sixty-three direct care workers from two areas in Sydney, Australia, who worked in community residences for persons with developmental and psychiatric disabilities were surveyed about symptoms of intrusive thoughts, avoidance, and hyperarousal one week after they experienced an assault or another type of work-related trauma. Survey respondents included 14 workers who requested and attended a one-session critical incident stress debriefing during the week after the incident, 18 workers from the same area of Sydney who had access to the intervention but chose not to attend, and 31 who worked in an area where the intervention was not available. RESULTS: Sixty-two workers reported symptoms of posttraumatic stress. Lower levels were reported by workers in the area where the intervention was available. When other factors were controlled, the lowest levels of stress were reported by workers to whom the debriefing was available but who chose not to attend. No significant difference in overall stress reduction in the week after the incident was found between the workers who received the intervention and those who did not. CONCLUSIONS: Although critical incident stress debriefing was evaluated positively by the majority of participants, aspects of the intervention such as its timing and the work environment in which it is offered may affect the degree to which participants benefit from it.
Staff who are assaulted by clients in direct care settings are at risk of developing symptoms associated with posttraumatic stress disorder (PTSD) (1,2). Intrusive thoughts, re-experiencing the incident, numbing, avoidant behavior, and hyperalertness are common reactions to traumatic incidents such as an assault. Eighty percent of assaulted workers may experience one or more of these symptoms in the first weeks after the assault, with up to 30 percent continuing to experience symptoms of traumatic stress for between four and six weeks after the assault (3).
Reports of assaults on nurses are not rare. One study found that 73 percent of nursing staff in a teaching hospital had been assaulted at some stage of their employment (3). Another study reported 16 injuries for every 100 staff members during one year (4). In one investigation, 65 percent of workers required between one week and one year to recover from all effects of the assault (5).
Exposure to traumatic incidents can overwhelm the usual coping strategies used by workers (6). The resulting stress has been associated with reduced cognitive, emotional, and behavioral performance (7) and may negatively affect work performance (8). These findings have implications for both the career path of the worker and the efficiency and productivity of organizations.
Critical incident stress debriefing was developed for use with emergency services personnel based on the principles of early intervention (9). It is a formal process that aims to assist recovery from psychological trauma by reducing distressing symptoms, enhancing and supporting emotional expression, and encouraging ventilation of feelings. Some authors have asserted that it is effective in preventing or mitigating the detrimental effects of exposure to traumatic stressors (9-11). Samter and associates (11) reported that debriefing promotes an ability to deal effectively with future stressors by alleviating the tendency to suppress the affective element of the traumatic experience.
Other authors have indicated that debriefing may not necessarily facilitate a positive adjustment and in some cases may increase levels of intrusive thoughts and avoidance (12- 15). Wortman (16) voiced concern over participants' prematurely confronting cognitive defenses such as denial; she feared that debriefing encounters may function only to solidify cognitive defenses.
Critical incident stress debriefing is usually evaluated positively by health care and emergency service workers (10,17). Although it is used widely, its efficacy has not been established (18). This study used a self-report survey to examine the efficacy of critical incident stress debriefing in alleviating the symptoms of posttraumatic stress among direct care workers' after their involvement in work-related trauma.
Methods
Participants
The study population comprised 322 direct care workers in 32 community homes for persons with developmental and psychiatric disabilities in two areas of Sydney, Australia. Area A included 13 community homes and 135 direct care positions. Area B included 19 homes and 187 positions. The community housing in both areas was managed by the same organization but was administered at a local level by individual teams.
Workers became study participants if they were involved in a traumatic work-related incident (work trauma) during the six-month data collection period (May 1994 to November 1994). Ninety-four workers (29 percent) from the two areas experienced work trauma during the period. Sixty-three returned the survey questionnaire, for an overall response rate of 67 percent.
The 63 respondents were assigned to one of three groups. The critical incident stress debriefing group comprised 14 workers from area A who requested and received debriefing. The first comparison group included 18 workers from area A who did not request and did not receive debriefing. The second comparison group consisted of 31 workers from area B who did not receive debriefing because it was not provided in area B.
The questionnaire response rates of the first and second comparison groups, 72 percent and 73 percent respectively, were higher than the response rate of the group that received debriefing, 58 percent. However, the response rate of the debriefing group was comparable to and in many instances higher than the rates in previous studies on the impact of assault and violence (1,5) and posttraumatic stress (19,20).
Demographic characteristics of respondents are presented in Table 1. The three groups were comparable in gender, age, education, experience in the field, and position held. The second comparison group reported significantly longer periods of employment in the current workplace than the other groups.
Intervention
Critical incident stress debriefing based on the Mitchell model (9), conducted as a group intervention by qualified personnel, was available to direct care workers in area A who experienced work trauma and asked for the debriefing. This intervention was available in area A for approximately nine months before the study but was not available to workers in area B. General discussion of the intervention at staff meetings ensured that workers in area A were aware of the availability of debriefing and of the procedure for obtaining it. Attendance was voluntary and thus involved self-selection. Generally, a participant attended one session, with individual follow-up if needed.
A belief central to the culture of many of the helping professions is that workers should be able to handle work-related assaults (2) and be able to cope at all times (21). Thus a key component of the debriefing process was the emphasis on restoration of the individual's coping skills and promotion of a sense of control after the event. Rather than using the debriefing as a tool solely for emotional expression, the participants were helped to develop a cognitive-psychological framework from which an understanding of their reactions and the recovery process could be gained.
After an introduction to the debriefing process, participants were encouraged to discuss the facts of the event with other members of the group to help clarify the questions "What happened?" and "Why did it happen?" Individual and group reactions to the event, including thoughts, feelings, and symptoms, were explored. Participants shared their individual methods of coping to help each other establish a variety of strategies for coping with incidents in the future, including support systems. This aspect of the process is called re-entry. The educational component of the debriefing included information on the nature of the stress response and a variety of techniques for managing physical, behavioral, cognitive, and emotional symptoms.
Instrument
Research in traumatic stress in direct care professions (1) and emergency-disaster studies (22) indicates that to encourage a good response rate a research instrument must be sensitive to the norms and customs of the group, allow privacy in addressing sensitive issues, and be time efficient. A review of the commercially available inventories did not uncover an appropriate instrument that fulfilled these criteria. Therefore, a paper-and-pencil self-report questionnaire that was sensitive to the work culture was developed for the study, based on literature in this area (1,11,23).
The constructs used in the questionnaire were defined as in previous research on traumatic stress (23) and were further clarified using a pilot study. Issues raised by participants in the pilot study centered on the questionnaire's length and on workers' willingness to complete it. Several items were deleted, and the final instrument had 36 items.
Eleven questions addressed the impact of the incident. They elicited information on the nature of the incident (for example, whether it was an assault or was related to the self-destructive behavior of a patient), the amount of missed work time, the injuries sustained (that is, whether a physical injury or emotional distress, or both, resulted), the levels of distress experienced at the time of the incident and when the questionnaire was completed, and exposure to work trauma in the three months before the incident.
A shorter version of the Impact of Event Scale (24) was incorporated into the questionnaire to measure the stress response syndrome. The items included four measures of intrusive thoughts and symptoms of re-experiencing and five measures of avoidance. Six items measuring the level of arousal adapted from the Everstine Trauma Response Index (25) were included to complete the triad of measures for posttraumatic stress. The questionnaire also included three items on the impact of the incident on levels of work stress and seven items to evaluate the debriefing. Cronbach's alpha coefficients for each scale ranged from .72 to .93, indicating a high interitem reliability.
Scales measuring the perceived levels of distress, work stress, and intrusive thoughts, avoidance, and arousal used a 6-point Likert scale. The response categories did not permit a neutral response, and the direction of the scale was reversed for some questions to avoid response acquiescence. Items were summed to yield a total score for each scale.
Procedure
Housing managers were contacted weekly during the data collection period to determine if any direct care workers had been involved in work trauma in the preceding week. Workers who were involved in incidents were given the questionnaire by the author approximately one week after the date of the reported incident. This period allowed for the debriefing process to have occurred when requested by the worker. Respondents were asked to complete the questionnaire anonymously and return it in the stamped envelope.
Because the sample was not random, comparisons were made between groups using the Mann-Whitney U test and chi square test; where applicable within-group comparisons used the Wilcoxon signed-rank test. An alpha level of .05 was used for all statistical tests.
Results
Nature and impact of incidents
Of the 63 workers who completed the questionnaire, 43 (68 percent) were physically assaulted by residents. Six workers (10 percent) were involved in incidents of self-injurious behavior by residents, and four (6 percent) were involved in assaults by one resident on another. Eight other workers (13 percent) experienced work trauma related to medical emergencies involving residents, residents absconding, verbal abuse by residents, and other aggression by residents. Two respondents did not provide this information.
Twenty-eight respondents (44 percent) indicated that they had been physically injured during the incident, and 56 (88 percent) reported emotional distress. The majority of respondents (54 respondents, or 86 percent) did not officially take leave after the incident. The amount of reported leave taken ranged from one to eight days, with a mean of three days. No significant differences in the nature of incidents, degree of injury, or amount of leave taken was observed between the three groups.
Distress was rated from 0, no distress, to 5, very distressed. The mean level of distress at the time of the incident was 4.3 for the debriefing group, 3.3 for the first comparison group, and 3.6 for the second comparison group. The debriefing group reported significantly higher levels of distress at the time of the incident than the first comparison group (Mann-Whitney U=62.5, p=.01) and the second comparison group (Mann-Whitney U=120, p=.01).
Responses indicated that stress tended to lessen for workers in all groups during the week between the incident and completion of the questionnaire. The mean rating for level of distress at the time of questionnaire completion was 2.1 for the debriefing group, 1.5 for the first comparison group, and 1.6 for the second comparison group. The tendency toward less distress over time was significant within all groups (p<.01). No significant difference in stress reduction was observed between the debriefing group and either of the comparison groups.
Fifty-six of the 63 respondents (89 percent) had experienced at least one previous work trauma. Most respondents (46 workers, or 73 percent) reported feeling a level of distress in response to the current incident that was similar to or greater than the level felt during previous incidents. Twenty-six respondents (41 percent) rated their current distress level as higher.
Work stress
Work stress was determined by asking respondents how much stress they felt at work, how much work stress was caused by work trauma, and how much work stress was caused by the ongoing possibility of the occurrence of work trauma.
As shown in Table 2, direct care workers from both areas reported similar levels of stress related to their everyday work and to the possibility of work trauma occurring, with no significant differences between the groups. However, the debriefing group reported a significantly higher level of work stress related to exposure to work trauma than the second comparison group. The second comparison group also reported significantly higher levels of work stress on this measure than the first comparison group (Mann-Whitney U=167, p=.02).
Posttraumatic stress symptoms
Table 3 shows the workers' ratings of symptoms of posttraumatic stress. The standard deviations for all groups indicate that workers in both areas reported the same range of individual differences in posttraumatic stress response.
All ratings of posttraumatic stress were higher for workers in area B where no debriefing was available than for workers in area A where debriefing was available. The measure of the stress response syndrome, which was the sum of the ratings of intrusive thoughts and avoidance, was significantly higher for workers in area B. The ratings for intrusive thoughts, the stress response syndrome, and posttraumatic stress response were all significantly higher in the second comparison group than in the first comparison group.
Within area A, the first comparison group consistently had lower ratings than the debriefing group on the individual measures of stress symptoms. On one hand, this finding may demonstrate the validity of allowing workers to choose whether to attend a debriefing. Alternatively, it may reflect the possibility that involvement in the debriefing intervention intensified the stress response of workers or their perception of stress.
In response to the question "Do you think debriefing has helped reduce the stress associated with traumatic incidents in your workplace?" eight of the 14 workers who attended a debriefing session (57 percent) responded positively. The other six workers reported that they did not feel debriefing assisted them in the reduction of posttraumatic stress.
Discussion
The results of this study highlight the frequency with which work trauma occurs in community housing and support earlier findings that direct care staff exposed to traumatic incidents are at increased risk of developing symptoms of PTSD (1,3). The majority of respondents in this study followed a normal process of stress recovery (26), reporting diminishing levels of distress during the seven-day period after the incident. However, some workers reported high levels of distress one week after the incident. This result was not unexpected because many workers reported experiencing work trauma daily.
The impact of these incidents was described well by one respondent: "There seems to be a cumulative effect where the emotional disruption of one incident blurs into the other, unrelentlessly (sic) adding emotional tension rather than resolving this energy." This situation illustrates the chronicity of the trauma experienced by some direct care workers and how lack of recovery periods may increase a worker's susceptibility to PTSD symptoms. It especially highlights the problems of determining when interventions are appropriate among workers who experience cumulative traumatic stress. In isolation each incident may appear to be unimportant and not to require special attention.
The question of whether critical incident stress debriefing helps participants deal constructively with trauma-related stress requires some consideration. Workers in area A, where the option of debriefing was provided in the week after the incident, reported a lower level of stress response symptoms than workers in area B, where debriefing was not an option. These results are consistent with previous studies of debriefing interventions (9,10). Workers in area A also reported significantly lower measures of work stress in response to work-related trauma. These results suggest that the debriefing—or its availability—ameliorated the stress response, especially in light of the finding that the nature of the incidents and degree of injury sustained were similar for workers from both areas and the fact that work management, policies, and procedures were similar in the two areas.
However, it should be noted that although policies and procedures were similar, differences in workplace environments between the areas may have influenced the way traumatic experiences were perceived and may to some extent account for the differences found. Training for the direct care workers in the study is similar to that for many helping professions in its emphasis on competency, not dependency. Many such workers feel that assault is part of the job (27) and that they should be able to handle work-based assault (2) and be able to cope at all times (21). The degree to which the particular work environment embraces these attitudes may have a direct impact on workers' willingness to see themselves as victims, acknowledge their responses to the event, and attempt to address their reactions. It may be that the work environment in area B did not acknowledge or validate the impact of work-based trauma on workers' functioning, which may have increased workers' psychological difficulties in coping with work trauma.
One of the most interesting findings of the study was that workers from area A who were debriefed rated their stress levels higher than workers from the same area who chose not to attend a debriefing. It may be that workers with high stress levels after work trauma sought debriefing while those with lower stress levels may not have felt the need for it. Indeed, debriefed workers accounted for more than 70 percent of all responses in the highest stress category, while the workers in area A who did not request debriefing (comparison group 1) accounted for 22 percent. More than 60 percent of the debriefed workers indicated that the current incident was more distressing than previous incidents, whereas only 37 percent of workers in comparison group 1 reported higher distress. These measures suggest that debriefed workers perceived the incident as more distressing than those in comparison group 1 and chose an appropriate means to reduce their distress. Conflict between the roles of helper and victim felt by some workers may also have contributed to vulnerability to stress (28).
One of the essential elements of critical incident stress debriefing is the psychoeducational component that provides participants with techniques for developing coping mechanisms and support systems for future use. Although the questionnaire in this study did not address past attendance at debriefing sessions, it may be that workers in area A who chose not to attend a debriefing had previously attended one and had learned methods of coping (11) that they were able to use, resulting in lower reported stress levels.
The debriefing intervention may have contributed to higher stress levels among participants. Discussion of individual reactions to the event may have increased participants' awareness of their reactions, resulting in higher ratings of stress. Alternatively, comments such as "I felt very blamed and in fact found that session more distressing than the incident itself" highlight concerns expressed by Bryant (12) and Griffiths and Watts (13) that critical incident stress debriefing does not necessarily ameliorate the psychological impact of trauma.
Further, although most of the 14 workers who participated in debriefing viewed it positively, it is interesting that six did not feel it assisted them in any way. Although workers may have used the debriefing evaluation form to express frustration about their inability to change the frequency with which trauma occurred in the workplace, the negative evaluations more likely reflect some participants' dissatisfaction with an aspect of the intervention or its failure to meet their expectations.
The close proximity of the traumatic incident, the debriefing, and the self-ratings of stress was an important aspect of this study, especially in regard to the utility of the intervention. Although such proximity may have allowed participants better recall, the timing of the debriefing may have had an unanticipated influence on the stress response of some workers. For workers who reported frequent assaults, a specific incident may have initiated debriefing; however, that incident may have required less attention in the debriefing than the impact of cumulative trauma. Many workers who experience repetitive trauma develop self-protective coping strategies—for example, cognitive defenses, such as denial (16). In these cases, debriefing held further in time from the initiating event may be more viable, allowing the worker some distance and insight with which to approach and benefit from debriefing.
Possible biases arising from subject selection were reduced because the study included all direct care workers who experienced work trauma during the data collection period, not just those who requested the intervention. In interpreting the results, self-selection by workers into the intervention, factors affecting participants' recall, the low response rate of the debriefing group, and the self-report technique should be considered.
Conclusions
This study explored critical incident stress debriefing to reduce stress response after traumatic incidents in the workplace. Workers in the area that offered debriefing after trauma reported a lower level of stress response than those in the area that did not provide debriefing. However, when other factors were controlled, the lowest level of stress response was reported by the workers to whom debriefing was available but who chose not to attend. It is important that no significant difference in overall stress reduction between the debriefing group and the comparison groups was observed in the week after the incident, during which time participants received the intervention.
The favorable view of the debriefing expressed by the majority of participants and the fact that participating in the intervention—or having it available—had a positive impact on stress levels suggest that critical incident stress debriefing has a role in addressing work-related trauma. The degree to which this intervention reduces symptoms of stress must be examined in light of the timing of the intervention and the work environment in which it is offered.
The evidence that some workers in the study regularly experienced traumatic incidents points to the need for further research on the impact of cumulative trauma and appropriate methods and timing of interventions. In addition, the impact of other variables such as coping strategies of workers, aspects of the work environment, cultural differences, and levels of social support should be explored.
Direct care workers, by virtue of their employment, are at increased risk of developing symptoms associated with PTSD. Further research into the effects of stress arising from trauma in the workplace is crucial and will ensure that appropriate support services and policies are implemented.
Ms. Matthews is affiliated with the School of Community Health, Faculty of Health Sciences, University of Sydney, P.O. Box 170, Lidcombe, New South Wales 2141, Australia.
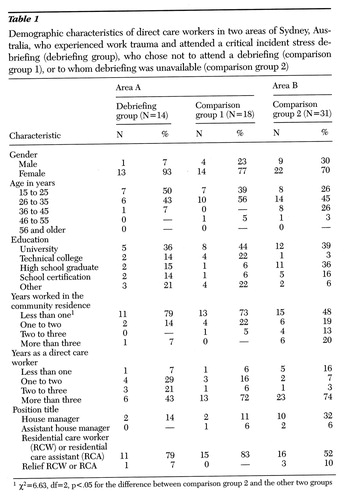 |
Table 1. Demographic characteristics of direct care workers in two areas of Sydney, Australia, who experienced work trauma and attended a critical incident stress debriefing (debriefing group), who chose not to attend a debriefing (comparison group 1), or to whom debriefing was unavailable (comparison group 2)1
1χ2=6.63, df=2, p<.05 for the difference between comparison group 2 and the other two groups
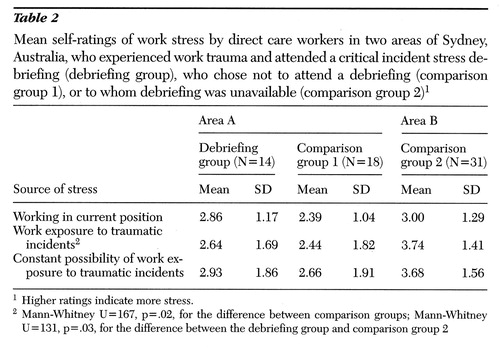 |
Table 2. Mean self-ratings of work stress by direct care workers in two areas of Sydney, Australia, who experienced work trauma and attended a critical incident stress debriefing (debriefing group), who chose not to attend a debriefing (comparison group 1), or to whom debriefing was unavailable (comparison group 2)1
1Higher ratings indicate more stress.
2Mann-Whitney U=167, p=.02, for the difference between comparison groups; Mann-Whitney U=131, p=.03, for the difference between the debriefing group and comparison group 2
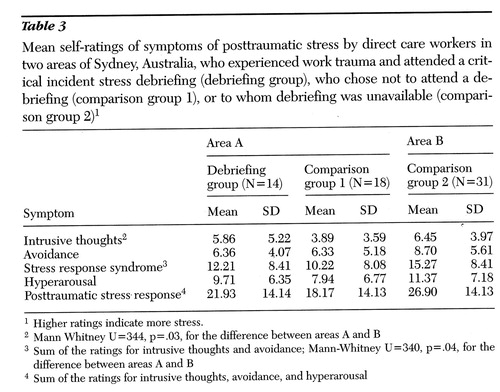 |
Table 3. Mean self-ratings of symptoms of posttraumatic stress by direct care workers in two areas of Sydney, Australia, who experienced work trauma and attended a critical incident stress debriefing (debriefing group), who chose not to attend a debriefing (comparison group 1), or to whom debriefing was unavailable (comparison group 2)1
1Higher ratings indicate more stress.
2Mann Whitney U=344, p=.03, for the difference between areas A and B
3Sum of the ratings for intrusive thoughts and avoidance; Mann-Whitney U=340, p=.04, for the difference between areas A and B
4Sum of the ratings for intrusive thoughts, avoidance, and hyperarousal
1. Caldwell MF: Incidence of PTSD among staff victims of patient violence. Hospital and Community Psychiatry 43:838-839, 1992Abstract, Google Scholar
2. Engle F, Marsh S: Helping the employee victim of violence in hospitals. Hospital and Community Psychiatry 37:159-162, 1986Medline, Google Scholar
3. Poster E, Ryan J: At risk of assault. Nursing Times 89(23):30-33, 1993Google Scholar
4. Carmel H, Hunter J: Staff injuries from inpatient violence. Hospital and Community Psychiatry 40:41-45, 1989Abstract, Google Scholar
5. Lanza ML: The reactions of nursing staff to physical assault by a patient. Hospital and Community Psychiatry 34:44-47, 1983Abstract, Google Scholar
6. Lewis GW: Managing crises and trauma in the workplace. American Association of Occupational Health Nursing Journal 41:124- 130, 1993Google Scholar
7. Mitchell JT, Dyregov A: Traumatic stress in disaster workers and emergency personnel: prevention and intervention, in International Handbook of Traumatic Stress Syndromes. Edited by Wilson JP, Raphael B. New York, Plenum, 1993Google Scholar
8. Paine WS: Job Stress and Burnout. Beverly Hills, Sage, 1992Google Scholar
9. Mitchell JT: When disaster strikes: the critical incident stress debriefing process. Journal of Emergency Medical Services 8(1):36-39, 1983Google Scholar
10. Robinson R, Mitchell JT: Evaluation of psychological debriefings. Journal of Traumatic Stress 6:367-382, 1993Crossref, Google Scholar
11. Samter J, Fitzgerald ML, Braudaway CA, et al: Debriefing: from military origin to therapeutic application. Journal of Psychosocial Nursing 31:23-27, 1993Google Scholar
12. Bryant R: Ethical considerations of managing posttraumatic responses. Bulletin of the Australian Psychological Society 16(3):3-5, 1994Google Scholar
13. Griffiths J, Watts R: The Kempsy and Grafton Bus Crashes: The Aftermath. Lismore, New South Wales, Australia, University of New England, Instructional Design Solutions, 1992Google Scholar
14. Hytten K, Hasle A: Fire fighters: a study of stress and coping. Acta Psychiatrica Scandinavica 80(suppl 355):50-55, 1989Google Scholar
15. McFarlane AC: The longitudinal course of posttraumatic morbidity, the range of outcomes, and their predictors. Journal of Nervous and Mental Disease 176:30-39, 1988Crossref, Medline, Google Scholar
16. Wortman C: Coping with victimization: conclusions and indications for future research. Journal of Social Issues 39:195-221, 1983Google Scholar
17. Laube-Morgan J: The professional's psychological response in disaster: implications for practice. Journal of Psychosocial Nursing 30:17-22, 1992Google Scholar
18. Watts R: The efficacy of critical incident stress debriefing for personnel. Bulletin of the Australian Psychological Society 16(3):6-7, 1994Google Scholar
19. Green MM, McFarlane AC, Hunter CE, et al: Undiagnosed posttraumatic stress disorder following motor vehicle accidents. Medical Journal of Australia 159:529-534, 1993Crossref, Medline, Google Scholar
20. McFarlane AC: Life events and psychiatric disorder: the role of a natural disaster. British Journal of Psychiatry 151:362-367, 1987Crossref, Medline, Google Scholar
21. Turnbull J: Victim support. Nursing Times 89(23):33-34, 1993Google Scholar
22. Baum A, Solomon SD, Ursano RJ, et al: Emergency/disaster studies, in International Handbook of Traumatic Stress Syndrome. Edited by Wilson JP, Raphael B. New York, Plenum, 1993Google Scholar
23. Horowitz MJ: Stress-Response Syndromes. New York, Aronson, 1976Google Scholar
24. Horowitz MJ, Wilner N, Alvarez W: Impact of Event Scale: a measure of subjective stress. Psychosomatic Medicine 41:309- 318, 1979Google Scholar
25. Everstine DS, Everstine L: The Trauma Response: Treatment for Emotional Injury. New York, Norton, 1993Google Scholar
26. Raphael B, Meldrum L: Helping people cope with trauma, in Coping With Trauma: The Victim and the Helper. Edited by Watts R, Horne D. Brisbane, Australian Academic Press, 1994Google Scholar
27. Ryan J, Poster E: When a patient hits you: a post-assault programme that puts nurses first. Canadian Nurse 87(8):23-25, 1991Google Scholar
28. Bowie V: Coping With Violence: A Guide for the Human Services. Campbelltown, Australia, Karibuni Press, 1989 Google Scholar



