Compliance With Medication Regimens for Mental and Physical Disorders
Abstract
OBJECTIVE: The authors reviewed research on medication compliance in psychiatric treatment and compared compliance rates with compliance rates in treatment of physical disorders. METHODS: MEDLINE was used to locate reports in the literature on medication compliance in psychiatric treatment for the years 1975 through 1996. These reports and studies cited in the reports were reviewed to determine the methods used to assess compliance and the compliance rates reported. Ten reports describing assessment methods and including medication compliance rates for antidepressant medication and 24 reports for antipsychotic medication were selected. They were compared with 12 reports that used microelectronic monitoring to assess medication compliance of patients with a range of nonpsychiatric disorders. RESULTS: Studies of psychiatric patients used various methods of estimating medication compliance, including interviews with patients, clinicians' judgment, and pill counts, but overall showed low rates of compliance. Patients receiving antipsychotics took an average of 58 percent of the recommended amount of the medications, with a range from 24 to 90 percent. Patients receiving antidepressants took 65 percent of the recommended amount, with a range from 40 to 90 percent. The mean compliance rate for patients with physical disorders was 76 percent, with a range from 60 to 92 percent, although the microelectronic monitoring showed frequent omission of doses and discontinuation of medication. CONCLUSIONS: Compliance with medication regimens among patients with psychiatric disorders may be lower than among patients with physical disorders. However, the difference may be largely attributable to the methods used for estimating compliance. The findings suggest the need for new and improved methods for monitoring compliance and increasing patients' compliance with pharmacotherapy.
Medication compliance has become a focus of increasing concern in the treatment of psychiatric disorders in recent years. With the growing fiscal pressure to reduce reliance on hospital treatment, to shorten hospital stays, and to reduce the intensity of outpatient treatment (1), contact between clinicians and patients may become increasingly restricted. As a result, opportunities to explain to patients the value of pharmacotherapy in psychiatric treatment and to encourage medication compliance may become more important than ever before. Thus information about factors that influence compliance and methods for facilitating optimal use of medication are especially important.
The difference between the efficacy of neuroleptic medications in carefully designed clinical trials and the effectiveness of these drugs in ordinary practice can be attributed largely to the less rigorous manner in which patients take medications—that is, partial compliance—in the typical outpatient treatment setting (2). Advancements in the treatment of psychiatric disorders are limited by discontinuation of medications and partial compliance, which steal power from even the most beneficial medications. Noncompliant patients' lack of treatment response can lead to their being switched from one drug to another, with little success because they do not take the drug as prescribed.
The psychiatric literature offers many theoretical explanations for why patients do not follow prescribed regimens. Unfortunately, most reports are either primarily descriptive or use unreliable methods of assessing compliance, such as patients' self-reports. Few studies adequately quantify the problem.
In this paper we review the literature on quantitative studies of medication compliance in psychiatric treatment. The purpose of the review is to evaluate estimated rates of compliance with psychopharmacologic treatment and compare them with rates of compliance in other areas of medicine.
Methods
We used MEDLINE to search the literature for the years 1975 to 1996. Key words used for the search were compliance, adherence, mental health, psychosis, schizophrenia, depression, and mood. Additional reports were selected from references in the papers identified in the search. Papers were included in our review if they reported studies in which medication compliance was evaluated and tabulated (including surveys and clinical trials with specific interventions) and if the method of assessing compliance was described. Meta-analyses of studies of compliance were considered separate resources.
Only ten reports about antidepressant medications and 26 reports about antipsychotic medications provided enough information to be included in the review. For comparison, we used data on rates of compliance with medication prescribed for a range of physical disorders. The data were drawn from a previous survey of 12 studies that used microelectronic monitoring of compliance, which is described below (3).
Four methods are commonly used to assess compliance with medication regimens. Each method has advantages and disadvantages.
Direct questioning of patients in interviews or by questionnaire, followed by clinicians' judgments about the accuracy of patients' responses, is a simple and rapid method but proved to be inadequate for evaluating medication compliance (4).
A count of the number of pills, tablets, or capsules a subject returns to researchers at the end of a study period constitutes a simple and rapid assessment of medication compliance. However, patients who want to avoid showing that they missed doses may not return unused medication. Pill counts provide accurate compliance estimates for compliant patients, but the accuracy diminishes among patients with lower compliance rates (5,6). Prescription renewals also can be used as a proxy indicator of compliance based on usage, making it convenient for computer analysis of refill rates. However, these analyses require that patients receive all refills from a single source and that the system records all changes in dose or drug.
Therapeutic drug monitoring, which involves testing the levels of a drug in the blood or urine, is invasive and requires costly laboratory analyses. However, blood levels can be misleading because rapidly cleared drugs achieve drug serum concentrations near target levels after several doses. Taking doses for a few days before a test raises drug levels reasonably close to target. These "spot levels" do not reflect compliance over a long period, although a blood level of zero clearly shows no recent drug ingestion (4). Urine tests provide evidence of ingestion of some medication at some recent time (4).
Microelectronic monitoring systems, a novel approach to assessing patient dosing, are now considered the best measure available for compliance assessment (7—9). In this method, a special bottle cap with a microprocessor is used to record data. The cap is engineered to record the date and time of every bottle opening. When the cap is connected to a computer, data are usually displayed as a calendar showing the number of container openings each day and the time of each bottle opening. The data can be shown to the patient as part of a program to enhance compliance in which the clinician would point out lapses and make suggestions about how to remember to take medication.
However, microelectronic systems are expensive and require computer software to view and analyze the data and are thus largely restricted to research. Although the results can be misleading if the patient opens the bottle but does not ingest the medication, such false recordings are presumed to be rare, based on previous studies (9). In addition, recent data are lost if the patient loses the bottle. (Previous data are stored on the computer.)
Results
Compliance with antipsychotic medications
Table 1 lists 24 reports (that include 26 patient groups) from which a compliance rate for antipsychotic medication could be determined (10-33). The methods for compliance assessment used in the studies were patient interview, clinician assessment, urine or blood marker, and pill count (number of tablets remaining). Most or all patients included in the studies had a diagnosis of schizophrenia. Rates of compliance differed by methodology and the number of patients evaluated, which ranged from 20 to 591. The mean level of compliance for antipsychotic medications among all 26 groups was 58±19 percent, with a range from 24 to 90 percent.
Thirteen papers reported on studies that used patient interviews. The mean rate of compliance in these studies was 52±17 percent, with a range from 24 to 87 percent. Thus the results for the studies using patient interviews, a less accurate method, skewed the overall rate.
The five studies that used clinician assessments found higher compliance (mean±SD=72±20 percent, with a range from 33 to 90 percent). Urine tests were used in seven studies, one in which they were supplemented by pill counts. The compliance rate in these studies was 60±18 percent, with a range from 35 to 88 percent. Thus a wide range of rates have been reported for compliance with antipsychotic medication.
Compliance with antidepressant medications
Table 2 lists ten reports from which a compliance rate for antidepressant medication could be determined (34-43). These reports are largely from clinical trials that included formal means for assessment of medication compliance. Pill counts and lithium blood levels were supplemented by patient interviews.
Results from two meta-analyses were included in the review. Goodwin and Jamison (42) surveyed ten reports with a mean rate of compliance of 66 percent (range=47 to 82 percent). In an evaluation of 67 studies, Montgomery and Kasper (43) found a mean compliance rate of 79 percent.
In the eight individual studies we reviewed, the number of subjects ranged from 40 to 254. The mean± SD rate of compliance was 63±18 percent, with a range from 40 to 90 percent, similar to the findings from meta-analyses.
Overall compliance for antidepressant medications was 65±18 percent, with a range from 40 to 90 percent, including all reports.
Compliance with medication for physical disorders
Before concluding that patients with psychiatric disorders have unusually poor compliance rates, we should consider comparable data from other populations (3). Table 3 lists data from a survey of 12 recent studies that used microelectronic systems to monitor dosing among patients with various physical disorders (8,44-54). Subjects in those studies took about 76±10 percent of doses as prescribed, with means ranging from 60 percent to 92 percent. However, compliance rates for individuals who participated in the studies ranged from 0 to 143 percent (rates over 100 percent indicate that the subject took more than the prescribed doses), showing a broad range of compliance with a variety of treatments for physical disorders.
Discussion
We found that the ranges of medication compliance rates reported for populations with psychiatric illness—24 to 90 percent for patients treated with antipsychotic medication and 40 to 90 percent for patients treated with antidepressants—were much wider than those reported for patients with physical disorders in studies using microelectronic monitoring, 60 to 92 percent. These differences may be attributed partly to the various definitions of compliance used in the studies and partly to the design and methods of assessment.
Thus it is not clear what differences in compliance might exist between populations with psychiatric illness and those with physical disorders. No studies of psychiatric patients that have used microelectronic monitoring or other methods of long-term quantitative assessment have been reported. However, an overview of the extensive literature on medication compliance found no differences in compliance rates between populations with physical disorders and those with psychiatric disorders (55).
Despite the potential for severe psychiatric or medical consequences, people do not consistently take the prescribed amount of medication. However, our review suggests little difference in rates of compliance among populations prescribed a variety of medications for various psychiatric and physical disorders.
The studies of patients with physical disorders included in our review used a system of continuous microelectronic monitoring that provided compliance data over a follow-up period. The studies of antidepressant treatment we reviewed were clinical trials in which pill counts were used to provide a quantitative, systematic assessment of compliance. Pill counts tend to overestimate compliance compared with microelectronic monitoring, with closest approximation among subjects with higher rates of compliance (5,6). Of the three groups of studies we reviewed, those that examined treatment with antipsychotic medication had the least quantitative study designs. Most of these studies reported rates of compliance based on patient interviews or clinicians' estimates.
Several studies show that the problem of poor initial compliance is compounded by the continued decline in compliance over time. Maddox and associates (41) found that only 40 percent of 46 patients started on an antidepressant continued to take it for a year. In a study of 40 patients with mood disorders, relapse was significantly associated with poor compliance (56). In another study, six of 12 patients who had relapses were identified as noncompliant, but only two of 28 patients without a recurrence were noncompliant (p<.04). Sullivan and associates (57) compared estimates of medication compliance with rates of hospitalization in a study of 101 patients with mental illness. Overall, poor compliance with medication was a significant factor in the need for rehospitalization (odds ratio of 8.2). In a retrospective review of 225 relapses among patients with schizophrenia, Razali and Yaha (58) found that only 27 percent of patients had good compliance with medication.
Many studies show that compliance is erratic (8,10,39,59,60). For example, patients with epilepsy in a long-term follow-up study that used continuous microelectronic monitoring were more compliant than usual (86 percent versus 75 percent, p<.01) during the week before and the week after a clinic visit, suggesting that compliance was influenced by anticipation of the visit and reinforcement of the need for treatment during the visit (59). However, compliance was significantly lower one month after the visit (67 percent, p<.05), suggesting reduced vigilance about the daily regimen as the time since a medical visit lengthened. In addition, microelectronic monitoring revealed that days with no dosing could be matched to a seizure occurring the following day.
Blackwell's 1996 paper (55) reviewed the literature published over the past 25 years on medication compliance for physical and psychiatric disorders. His eloquent analysis of social history as a context for medical issues was based on about 12,000 publications, half of them review articles and half reporting original data. The literature suggesed that good compliance is related to patients' satisfaction, continuity of care, and acceptance of the need for treatment. Poor compliance was thought to be common among patients with chronic, asymptomatic disorders and was associated with complex treatment regimens, adverse effects, and social dysfunction. A more pragmatic view has been offered by Urquhart (61), who developed the concept of "forgiving" medications—those that continue to provide a therapeutic effect even when a dose is late or forgotten.
The effects of strategies aimed at improving compliance are unlikely to differ significantly in different patient populations. The simplest techniques to help patients enhance their medication-taking behaviors are based on the use of cues that establish a daily pattern for the individual (62). Using a specific cue such as a specific time of day, a meal, or other daily habit helps reinforce the behavior of taking a dose of medication as part of a daily routine. We are currently engaged in research to evaluate the effectiveness of simple cues and other direct feedback techniques for patients with severe mental illnesses.
Conclusions
The literature on compliance with medication regimens suggests that no consequence of noncompliance is so severe or onerous that it invariably produces full treatment compliance. Thus it is not surprising that patients who received antidepressant medication differed little from those with physical disorders in their compliance with a medication regimen and that the compliance rates of patients who received antipsychotic medication and were likely to have the cognitive deficits associated with schizophrenia were not much lower than those of patients with other disorders. Use of more reliable, quantitative methods in studies of psychiatric populations may reveal even less difference in compliance rates between psychiatric patients who receive antipsychotic or antidepressant medication and patients who receive a variety of medications for treatment of nonpsychiatric disorders.
Acknowledgments
This work was supported by grant R24-MH54446 from the medication effectiveness research program of the National Institute of Mental Health and by the Health Services Research Service and the Northeast Program Evaluation Center of the Department of Veterans Affairs.
Ms. Cramer is lecturer and Dr. Rosenheck is clinical professor in the department of psychiatry at Yale University School of Medicine in New Haven, Connecticut. Ms. Cramer is also project director in the psychiatry service at the Veterans Affairs Connecticut Healthcare System in West Haven, Connecticut. Dr. Rosenheck is director of the VA Northeast Program Evaluation Center in West Haven. Address correspondence to Ms. Cramer, Health Services Research, Room 7-84, VA Connecticut Healthcare System, 950 Campbell Avenue, West Haven, Connecticut 06516.
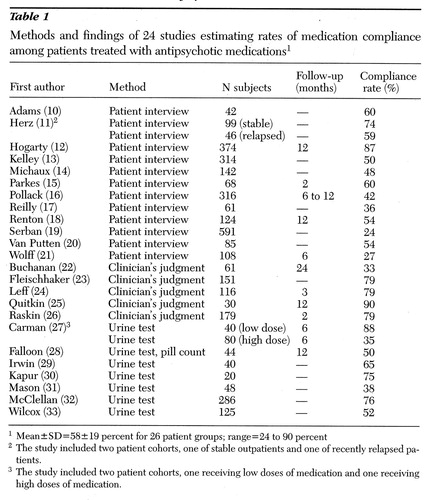 |
Table 1. Methods and findings of 24 studies estimating rates of medication compliance among patients treated with antipsychotic medications1
1Mean±SD=58±19 percent for 26 patient groups; range=24 to 90 percent
2The study included two patient cohorts, one of stable outpatients and one of recently relapsed patients.
3The study included two patient cohorts, one receiving low doses of medication and one receiving high doses of medication.
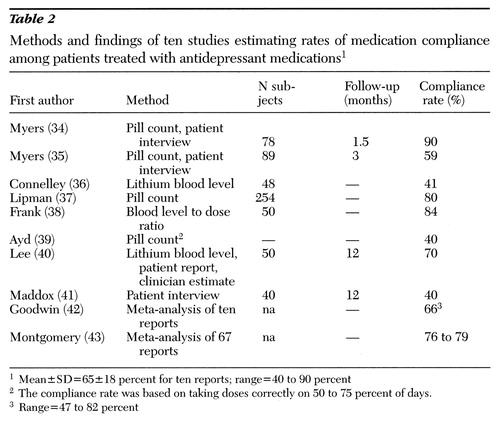 |
Table 2. Methods and findings of ten studies estimating rates of medication compliance among patients treated with antidepressant medications1
1Mean±SD=65±18 percent for ten reports; range=40 to 90 percent
2The compliance rate was based on taking doses correctly on 50 to 75 percent of days.
3Range=47 to 82 percent
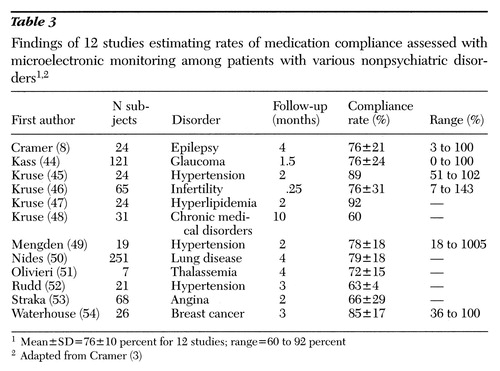 |
Table 3. Findings of 12 studies estimating rates of medication compliance assessed with microelectronic monitoring among patients with various nonpsychiatric disorders1,2
1Mean±SD=76±10 percent for 12 studies; range=60 to 92 percent
2Adapted from Cramer (3)
1. Feldman JL, Fitzpatrick RJ: Managed Mental Health Care. Washington, DC, American Psychiatric Press, 1992Google Scholar
2. Cramer JA, Spilker B (eds): Patient Compliance in Medical Practice and Clinical Trials. New York, Raven Press, 1991Google Scholar
3. Cramer JA: Partial medication compliance: the enigma in poor medical outcomes. American Journal of Managed Care 1:45- 52, 1995Google Scholar
4. Cramer JA: Overview of methods to measure and enhance patient compliance, in Patient Compliance in Medical Practice and Clinical Trials. Edited by Cramer JA, Spilker B. New York, Raven Press, 1991Google Scholar
5. Rudd P, Bynny RL, Zachary V, et al: Pill count measures of compliance in a drug trial: variability and suitability. American Journal of Hypertension 1:309-312, 1988Crossref, Medline, Google Scholar
6. Pullar T, Birtwell AJ, Wiles PG, et al: Use of a pharmacologic indicator to compare compliance with tablets prescribed to be taken once, twice, or three times daily. Clinical Pharmacology and Therapeutics 44:545- 545, 1988Google Scholar
7. Cramer JA: Microelectronic systems for monitoring and enhancing patient compliance with medication regimens. Drugs 49:321-327, 1995Crossref, Medline, Google Scholar
8. Cramer JA, Mattson RH, Prevey ML, et al: How often is medication taken as prescribed? A novel assessment technique. JAMA 261:3273-3277, 1989Crossref, Medline, Google Scholar
9. Cramer JA, Mattson RH: Monitoring compliance with antiepileptic drug therapy, in Patient Compliance in Medical Practice and Clinical Trials. Edited by Cramer JA, Spilker B. New York, Raven Press, 1991Google Scholar
10. Adams SG, Howe JT: Predicting medication compliance in a psychiatric population. Journal of Nervous and Mental Disease 181:558-560, 1993Crossref, Medline, Google Scholar
11. Herz MI, Melville C: Relapse in schizophrenia. American Journal of Psychiatry 137:801-805, 1980Link, Google Scholar
12. Hogarty GE, Goldberg SC, Collaborative Study Group: Drug and sociopathy in the aftercare of schizophrenic patients: one-year relapse rates. Archives of General Psychiatry 28:54-64, 1973Crossref, Medline, Google Scholar
13. Kelley GR, Scott JE: Medication compliance and health education among outpatients with chronic mental disorders. Medical Care 28:1181-1197, 1990Crossref, Medline, Google Scholar
14. Michaux WW: Side effects, resistance, and dosage deviations in psychiatric outpatients treated with tranquilizers. Journal of Nervous and Mental Disease 133:203-212, 1961Crossref, Medline, Google Scholar
15. Parkes CM, Brown GW, Monck EM: The general practitioner and the schizophrenic patient. British Medical Journal 2:972-976, 1962Crossref, Medline, Google Scholar
16. Pollack B: The effect of chlorpromazine in reducing the relapse rate in 716 released patients: study 3. American Journal of Psychiatry 114:749-751, 1958Link, Google Scholar
17. Reilly EL, Wilson WP, McClinton HK: Clinical characteristics and medication history of schizophrenics readmitted to the hospital. International Journal of Neuropsychiatry 3:85-90, 1967Google Scholar
18. Renton CA, Affleck JW, Carstairs GM, et al: A follow-up of schizophrenic patients in Edinburgh. Acta Psychiatrica Scandinavica 39:548-600, 1963Crossref, Medline, Google Scholar
19. Serban G, Thomas A: Attitudes and behaviors of acute and chronic schizophrenic patients regarding ambulatory treatment. American Journal of Psychiatry 131:991- 995, 1974Link, Google Scholar
20. Van Putten T: Why do schizophrenic patients refuse to take their drugs? Archives of General Psychiatry 31:67-72, 1974Google Scholar
21. Wolff RJ, Colacino DM: A preliminary report on the continued post-hospital use of tranquilizing drugs. American Journal of Psychiatry 118:499-503, 1961Link, Google Scholar
22. Buchanan A: A two-year prospective study of treatment compliance in patients with schizophrenia. Psychological Medicine 22:787-797, 1992Crossref, Medline, Google Scholar
23. Fleishhacker WW, Meise U, Gunther V, et al: Compliance with antipsychotic drug treatment: influence of side effects. Acta Psychiatrica Scandinavica 89 (suppl 382):11-15, 1994Google Scholar
24. Leff JP, Wing JK: Trial of maintenance therapy in schizophrenia. British Medical Journal 3:599-604, 1971Crossref, Medline, Google Scholar
25. Quitkin F, Rifkin A, Kane J, et al: Long- acting oral vs injectable antipsychotic drugs in schizophrenics. Archives of General Psychiatry 35:889-892, 1978Crossref, Medline, Google Scholar
26. Raskin A: A comparison of acceptors and resistors of drug treatment as an adjunct to psychotherapy. Journal of Consulting and Clinical Psychology 25:366, 1961Crossref, Google Scholar
27. Carman JS, Wyatt ES, Fleck R, et al: Neuroleptic compliance in schizophrenic outpatients. Psychiatric Hospitals 15:173-178, 1984Google Scholar
28. Falloon I, Watt DC, Shepherd M: A comparative controlled trial of pimozide and fluphenazine decanoate in the continued therapy of schizophrenia. Psychological Medicine 8:59-70, 1978Crossref, Medline, Google Scholar
29. Irwin DS, Weitzel WD, Morgan DW: Phenothiazine intake and staff attitudes. American Journal of Psychiatry 127:1631-1635, 1971Link, Google Scholar
30. Kapur S, Ganguli R, Ulrich R, et al: Use of random sequence riboflavin as a marker of medication compliance in chronic schizophrenics. Schizophrenia Research 6:49-53, 1992Google Scholar
31. Mason AS, Forrest IS, Forrest FW, et al: Adherence to maintenance therapy and rehospitalization. Diseases of the Nervous System 24:103-104, 1963Google Scholar
32. McClellan TA, Cowan G: Use of antipsychotic and antidepressant drugs by chronically ill patients. American Journal of Psychiatry 126:1771-1773, 1970Link, Google Scholar
33. Willcox DRC, Gillan R: Do psychiatric out-patients take their drugs? British Medical Journal 2:790-792, 1965Google Scholar
34. Myers ED, Calvert EJ: Information, compliance, and side-effects: a study of patients on antidepressant medication. British Journal of Clinical Pharmacology 17:21-25, 1984Crossref, Medline, Google Scholar
35. Myers ED, Branthwaite A: Out-patient compliance with antidepressant medication. British Journal of Psychiatry 160:83- 86, 1992Crossref, Medline, Google Scholar
36. Connelly CE, Davenport YB, Nurnberger JT: Adherence to treatment regimen in a lithium carbonate clinic. Archives of General Psychiatry 39:585-588, 1982Crossref, Medline, Google Scholar
37. Lipman RS, Rickels K, Uhlenhuth EH, et al: Neurotics who fail to take their drugs. British Journal of Psychiatry 111:1043- 1049, 1965Crossref, Medline, Google Scholar
38. Frank JD, Gliedman LH, Imber SD, et al: Why patients leave psychotherapy. Archives of Neurology and Psychiatry 77:283-299, 1957Crossref, Google Scholar
39. Ayd FJ: Single daily dose of antidepressants. JAMA 230:263-264, 1974Crossref, Medline, Google Scholar
40. Lee S: The prevalence and nature of lithium noncompliance among Chinese psychiatric patients in Hong Kong. Journal of Nervous and Mental Disease 181:618-625, 1993Crossref, Medline, Google Scholar
41. Maddox JC, Levi M, Thompson C: The compliance with antidepressants in general practice. Journal of Psychopharmacology 8:48-53, 1994Crossref, Medline, Google Scholar
42. Goodwin FK, Jamison KR: Manic-Depressive Illness. New York, Oxford University Press, 1990Google Scholar
43. Montgomery SA, Kasper S: Comparison of compliance between serotonin reuptake inhibitors and tricyclic antidepressants: a meta-analysis. International Clinical Psychopharmacology 9(suppl 4):33-40, 1995Medline, Google Scholar
44. Kass MA, Meltzer DW, Gordon M, et al: Compliance with topical pilocarpine treatment. American Journal of Ophthalmology 101:515-523, 1986Crossref, Medline, Google Scholar
45. Kruse W, Rampmaier J, Ullrich G, et al: Patterns of drug compliance with medications to be taken once or twice daily assessed by continuous electronic monitoring in primary care. International Journal of Clinical Pharmacology and Therapeutics 32:452-457, 1994Medline, Google Scholar
46. Kruse W, Eggert-Kruse W, Rampmaier J, et al: Dosage frequency and drug compliance behavior: a comparative study on compliance with a medication to be taken twice or four times daily. European Journal of Clinical Pharmacology 41:589-592, 1991Crossref, Medline, Google Scholar
47. Kruse W, Nikolaus T, Rampmaier J, et al: Actual versus prescribed timing of lovastatin doses assessed by electronic compliance monitoring. European Journal of Clinical Pharmacology 45:211-215, 1993Crossref, Medline, Google Scholar
48. Kruse W, Weber E: Dynamics of drug regimen compliance: its assessment by microprocessor-based monitoring. European Journal of Clinical Pharmacology 38:561- 565, 1990Crossref, Medline, Google Scholar
49. Mengden T, Binswanger B, Spuhler T, et al: The use of self-measured blood pressure determinations in assessing dynamics of drug compliance in a study with amplodipine once a day, morning versus evening. Journal of Hypertension 11:1403-1411, 1993Crossref, Medline, Google Scholar
50. Nides MA, Tashkin DP, Simmons MS, et al: Improving inhaler adherence in a clinical trial through the use of the Nebulizer Chronolog. Chest 104:501-507, 1993Crossref, Medline, Google Scholar
51. Olivieri NF, Matsui D, Hermann C, et al: Compliance assessed by the Medication Event Monitoring System. Archives of Diseases in Childhood 66:1399-1402, 1991Crossref, Medline, Google Scholar
52. Rudd P, Ahmed S, Zachary V: Antihypertensive drug trials: contributions from medication monitors, in Patient Compliance in Medical Practice and Clinical Trials. Edited by Cramer JA, Spilker B. New York, Raven Press, 1991Google Scholar
53. Straka RJ, Fish JT, Benson SR, et al: Magnitude and nature of noncompliance with treatment using isosorbide dinitrate in patients with ischemic heart disease. Journal of Clinical Pharmacology 36:587-594, 1996Crossref, Medline, Google Scholar
54. Waterhouse DM, Calzone KA, Mele C, et al: Adherence to oral tamoxifen: a comparison of patient self-report, pill counts, and microelectronic monitoring. Journal of Clinical Oncology 11:1189-1197, 1993Crossref, Medline, Google Scholar
55. Blackwell B: From compliance to alliance: a quarter century of research. Netherlands Journal of Medicine 48:140-149, 1996Crossref, Medline, Google Scholar
56. Salem RB, Keane TM, Williams JG: Drug related admissions to a Veterans Administration psychiatric unit. Drug Intelligence and Clinical Pharmacology 18:74-76, 1984Crossref, Medline, Google Scholar
57. Sullivan G, Wells KB, Morgenstern H, et al: Identifying modifiable risk factors for rehospitalization: a case-control study of seriously mentally ill persons in Mississippi. American Journal of Psychiatry 152:1749- 1756, 1995Link, Google Scholar
58. Razali MS, Yaha H: Compliance with treatment in schizophrenia: a drug intervention program in a developing country. Acta Psychiatrica Scandinavica 91:331-335, 1995Crossref, Medline, Google Scholar
59. Cramer JA, Scheyer R, Mattson R: Compliance declines between clinic visits. Archives of Internal Medicine 150:1509- 1510, 1990Crossref, Medline, Google Scholar
60. Farmer KC, Jacobs EW, Phillips CR: Long-term patient compliance with prescribed regimens of calcium channel blockers. Clinical Therapeutics 16:316-326, 1994Medline, Google Scholar
61. Urquhart J: Variable patient compliance in ambulatory trials: nuisance, threat, opportunity. Journal of Antimicrobial Chemotherapy 32:643-649, 1993Crossref, Medline, Google Scholar
62. Cramer JA: Medication use by the elderly: enhancing compliance behaviors and packaging aids. Drugs and Aging, in pressGoogle Scholar



