Psychiatric Hospitalization of Persons With Dual Diagnoses: Estimates From Two National Surveys
Abstract
Individuals with both mental illness and alcohol or drug use disorders present distinctive treatment and human service problems, including increased risk for psychiatric hospitalization in community hospitals. Using national hospital discharge abstract data for 1990 and 1994, this study compared differences in psychiatric hospitalization in community hospitals of patients with mental illness only and those with mental disorders and substance use disorders. Individuals with dual diagnoses were younger, and a greater proportion were men. Medicaid was the primary payer for a larger percentage of those with dual diagnoses. Nationally, the number of commmunity hospitalizations for dually diagnosed patients increased 15 percent from 1990 to 1994, and total hospital charges increased from $1.9 to $2.2 billion.
Persons with dual diagnoses are distinctive in that they have an underlying mental illness as well as an alcohol or drug use disorder. In an evaluation of a residential treatment program for patients with this condition in Washington State, 43 percent were hospitalized for psychiatric reasons in community hospitals in the year before admission to residential treatment (Maynard C, Cox GB, unpublished report, 1998).
The purpose of this study was to examine at the national level the pervasiveness of community psychiatric hospitalization of patients with both mental illness and substance use disorders. Using hospital discharge abstract data from two different national databases, the National Hospital Discharge Survey and the Nationwide Inpatient Sample from the Healthcare Cost and Utilization Project, we addressed two questions. First, among patients hospitalized in the community for psychiatric reasons, how do those who have both diagnoses compare with those who have only diagnoses of mental disorders, and, second, did the number of hospitalizations for patients with dual diagnoses increase from 1990 to 1994?
Methods
National Hospital Discharge Survey
The National Hospital Discharge Survey is an annual sample of hospital discharge records from nonfederal short-stay hospitals located in the 50 states and the District of Columbia (1). State mental hospitals as well as federal, military, and Veterans Affairs hospitals are not included. The study reported here used information from both the 1990 (N= 235,947) and 1994 (N=245,121) surveys.
The hospital records contain demographic information about patients as well as information about the geographic location of the hospital, length of stay, and primary payer. Also included are the principal diagnosis and up to six secondary ICD-9-CM codes. In addition, sampling weights are provided for calculating national estimates of the number of hospitalizations.
Nationwide Inpatient Sample
The Nationwide Inpatient Sample contains data on more than 6 million hospital discharges from more than 900 hospitals in 17 states for 1994 (2). These records represent 20 percent of hospital discharges in the participating states. Hospitals were randomly selected based on several categories. They were ownership control, bed size, teaching status, urban or rural location, and region of the United States. To calculate national estimates, each hospital was assigned a sampling weight in relation to the universe of hospitals, which included nonfederal acute care community hospitals identified by the American Hospital Association. The sampling frame was constructed from the subset of the universe of hospitals that released their discharge data for research purposes.
Records from the Nationwide Inpatient Sample contain more information than do those from the National Hospital Discharge Survey; for example, the former identifies the actual hospital and includes total charges.
Patient population
We selected hospitalizations of patients who had a principal diagnosis in one of the following diagnostic categories: alcohol use disorders; drug use disorders; senility and organic mental disorders; affective disorders; schizophrenia and related disorders; other psychoses; anxiety, somatoform, and personality disorders; preadult disorders; other mental conditions; and personal history of mental disorders. These diagnostic categories and their corresponding ICD-9-CM diagnosis codes have been defined elsewhere (3). Individuals with dual diagnoses had a combination of alcohol or drug use disorders plus one or more disorders in one or more of the other eight diagnostic categories.
Results
Patients with dual diagnoses accounted for 17 percent and 19 percent of psychiatric hospitalizations in the National Hospital Discharge Survey in 1990 and 1994, respectively. In the Nationwide Inpatient Sample, which had more secondary diagnosis codes, they constituted 25 percent of hospitalizations for mental disorders.
Table 1 shows the characteristics of mentally ill patients in the three samples who did and did not have dual diagnoses. Patients with dual diagnoses were younger than their counterparts with only mental illness, and a greater proportion were men. The primary payer was also different for the two groups—Medicaid was the primary payer for a larger percentage of the dual diagnosis group.
In the National Hospital Discharge Survey, a slight but statistically significant increase was noted from 1990 to 1994 in the proportion of hospitalizations for which both mental illness and substance use disorders were recorded (χ2 =31.6, df=1, p<.001). Using the case weights provided, we estimated that the number of these hospitalizations for all nonfederal acute care hospitals increased 15 percent, from 252,797 hospitalizations in 1990 to 291,801 in 1994. The number of hospitalizations decreased 2.4 percent between 1990 and 1994 for those with mental illness only.
Using case weights for the Nationwide Inpatient Sample for all U.S. hospitals, we estimated a total of 429,558 hospitalizations of patients with both mental illness and alcohol or drug use disorders. This estimate is 47 percent greater than the estimate from the 1994 National Hospital Discharge Survey, although for 1994 the total number of hospitalizations for mental disorders only was 2 percent higher in the Nationwide Inpatient Sample. To make the two surveys comparable, only the first six diagnostic codes were considered. Even with this adjustment, there were still an estimated 373,212 hospitalizations of patients with dual diagnoses in 1994.
In 1994 in the Nationwide Inpatient Sample, the mean charge per hospital stay was almost $7,400 for patients with dual diagnoses. Applying this charge to the more conservative estimates of hospitalizations from the National Hospital Discharge Survey resulted in total charges of $1.9 billion for 1990 and $2.2 billion for 1994 for patients with dual diagnoses. Using the higher number from the Nationwide Inpatient Sample, we estimated that community psychiatric hospitalization for patients with mental illness and chemical dependencies resulted in hospital charges of $3.2 billion.
Discussion and conclusions
Psychiatric hospitalization for individuals with dual diagnoses is often indicative of a breakdown in the treatment process or an undesired change in the disorder (4). Patients with dual diagnoses place heavy demands on publicly funded psychiatric hospitalization, which increased from 1990 to 1994. Compared with persons with mental disorders only, those with dual diagnoses are younger men who are more likely to be arrested, hospitalized, or placed in conservatorship (5,6) and after hospitalization are more likely to be rehospitalized (7). Other reports indicate that individuals with dual disorders are not receiving the services they need (8,9). One powerful argument for improved residential and outpatient treatment, as well as stable housing (10), is that these factors may reduce high costs associated with psychiatric hospitalization.
It is important to recognize limitations of large administrative databases. For 1994 the National Hospital Discharge Survey and the Nationwide Inpatient Sample produced different estimates of the number of hospitalizations for the dual diagnosis group, although the estimates for those with mental disorders only were similar. This discrepancy may be partly due to the different diagnostic coding practices at the individual hospitals. Changes in coding practices might explain the increase in hospitalization for patients with dual diagnoses. In addition, diagnosis of these patients is often a complex undertaking and can be quite arbitrary depending on the clinician.
A second limitation is that none of the databases contained record linkage numbers to permit identification of repeat hospitalizations. Strictly speaking, the unit of analysis in this report is the hospitalization and not the patient. Finally, the national estimates of total charges and number of hospitalizations are based on random samples and may not be representative of all nonfederal short-term hospitals.
Despite these limitations, the findings of this report document the pervasiveness of psychiatric hospitalization for those with dual diagnoses.
First-Person Accounts Invited for Column
Patients, former patients, family members, and mental health professionals are invited to submit first-person accounts of experiences with mental illness and treatment for the Personal Accounts column of Psychiatric Services. Maximum length is 1,600 words. The column appears every other month.
Material to be considered for publication should be sent to the column editor, Jeffrey L. Geller, M.D., M.P.H., at the Department of Psychiatry, University of Massachusetts Medical School, 55 Lake Avenue North, Worcester, Massachusetts 01655. Authors may publish under a pseudonym if they wish.
Dr. Maynard is research scientist in the department of medicine at the University of Washington, 3937 15th Avenue, N.E., Seattle, Washington 98105 (e-mail, [email protected]). Dr. Cox is senior research scientist in the Alcohol and Drug Abuse Institute at the university.
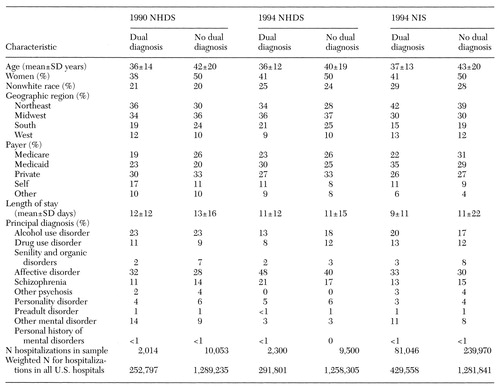 |
Table 1. Characteristics of mentally ill patients included in the 1990 and 1994 National Hospital Discharge Survey (NHDS) and the 1994 Nationwide Inpatient Sample (NIS) who did and did not have dual diagnoses
1. WR Simmons: Development of the Design of the NCHS Hospital Discharge Survey. Vital and Health Statistics. Public Health Service pub 1000, series 2, no 39. Hyattsville, Md, National Center for Health Statistics, Sept 1970Google Scholar
2. Health Care Cost and Utilization Project (HCUP-3): Nationwide Inpatient Sample, Release 3. Rockville, Md, Agency for Health Care Policy and Research, 1994Google Scholar
3. Clinical Classifications for Health Policy Research, Version 2: Software and User's Guide. AHCPR pub 96-0046. Rockville, Md, Agency for Health Care Policy and Research, Apr 1996Google Scholar
4. Jerrell JM, Ridgely MS: Evaluating changes in symptoms and functioning of dually diagnosed clients in specialized treatment. Psychiatric Services 46:233-238, 1995Link, Google Scholar
5. Ford L, Snowden LR, Walser EJ: Outpatient mental health and the dual-diagnosis patient: utilization of services and community adjustment. Evaluation and Program Planning 14:291-298, 1991Crossref, Google Scholar
6. Barry KL, Fleming MF, Greenley JR, et al: Characteristics of persons with severe mental illness and substance abuse in rural areas. Psychiatric Services 47:88-90, 1996Link, Google Scholar
7. Caan W, Crowe M: Using readmission rates as indicators of outcome in comparing psychiatric services. Journal of Mental Health 3:521-524, 1994Crossref, Google Scholar
8. Lehman AF, Myers CP, Johnson J, et al: Service needs and utilization for dual diagnosis patients. American Journal on Addictions 4:163-169, 1995Crossref, Google Scholar
9. Grella CE, Hser YI: A county survey of mental health services in drug treatment programs. Psychiatric Services 48:950-952, 1997Link, Google Scholar
10. Bebout RR, Drake RE, Xie H, et al: Housing status among formerly homeless dually diagnosed adults. Psychiatric Services 48:936-941, 1997Link, Google Scholar



