Factors Affecting Engagement of Dual Diagnosis Patients in Outpatient Treatment
Abstract
This study examined factors associated with engagement in outpatient treatment of patients with dual diagnoses of psychiatric disorder and substance use disorder. The charts of all 57 patients referred to a dual diagnosis treatment program during a six-month period were reviewed, and data on patients' substance use diagnosis, psychiatric diagnosis, sex, ethnicity, and referral source were collected. Patients referred from inpatient treatment were more likely to attend three or more appointments at the dual diagnosis program than those referred from outpatient treatment. Substance of abuse interacted with both referral source and sex in predicting engagement.
Comorbidity of substance use disorders and other psychiatric disorders (dual diagnosis) is a common clinical problem with significant and clinically relevant effects on symptomatology, course, treatment outcome, and service utilization (1,2,3,4,5,6,7,8,9). One of the major difficulties in treating dual diagnosis is in engaging the patient in treatment (9). However, few studies have examined which subgroups of dual diagnosis patients are more or less likely to become engaged in treatment.
Miner and associates (10) used logistic regression to identify factors predicting outpatient treatment compliance among patients with schizophrenia or schizoaffective disorder and comorbid substance use disorders. They found that men, subjects with mixed-syndrome schizophrenia, and those with low scores for affective flattening and blunting on the Schedule for the Assessment of Negative Symptoms (indicating a low level of symptoms) were most likely to be noncompliant with outpatient treatment. The study did not include patients with other psychiatric diagnoses and did not consider the possible effects of referral source and ethnicity.
The aim of the study reported here was to identify patient variables associated with engagement in treatment in a clinical population of patients referred for dual diagnosis treatment. Because of their presumed association with greater severity of illness, the following three patient characteristics were hypothesized to be related to lower rates of engagement: inpatient rather than outpatient source of referral, drug rather than alcohol use disorder, and psychotic psychiatric diagnosis. Among inpatient referrals, we expected the Global Assessment of Functioning (GAF) score at discharge to correlate with engagement in subsequent treatment.
Methods
Subjects included all patients newly referred to a dual diagnosis outpatient treatment program within the six-month period from October 1996 through March 1997. Information was obtained by chart review. A total of 57 subjects—35 men and 22 women—were included in the study. Their mean age was 35.2 years, with a range from 19 to 57 years. Thirty-four patients were non-Hispanic white, 18 were Hispanic, and five were African American. The primary psychiatric and substance use disorder diagnoses were obtained from discharge summaries (inpatient referrals) or outpatient records (outpatient referrals). Twenty-eight patients (49 percent) had a psychotic disorder, 21 (37 percent) had a nonpsychotic mood disorder, and eight (14 percent) had an anxiety or personality disorder. Thirty-five patients (61 percent) had primarily alcohol use disorders, and 22 (39 percent) had other drug use disorders.
Referral source for each subject was recorded. Forty-six patients were referred from programs within the mental health center where the dual diagnosis program was located. Twenty-seven of those subjects (47.4 percent of all subjects) were referred from inpatient psychiatric treatment on an acute unit where length of stay averaged one to two weeks. Ten subjects (17.5 percent) were referred from psychiatric outpatient clinics, and nine (15.8 percent) were referred from the psychiatric emergency service. The remaining 11 subjects (19.3 percent) were referred from a variety of inpatient and outpatient services outside of the mental health center where the dual diagnosis program was located. For patients referred from inpatient treatment, GAF at admission and discharge was recorded. For each subject, the total number of appointments attended at the dual diagnosis treatment program was recorded. Subjects were categorized as engaged in treatment if they attended a total of three or more outpatient appointments in the study period.
Data were analyzed using SPSS for Windows. Significance level was set at p<.05 with no correction for multiple comparisons. All tests were two-tailed. Logistic regression analysis used the forward conditional method.
Results
Subjects attended a mean±SD of 3.77±3.28 appointments, with a range from none to 11. Thirty-two subjects (56.1 percent) attended three or more appointments. Contrary to our hypothesis, the mean total number of appointments was higher for inpatient referrals than for outpatient referrals (mean±SD=5.10±3.38 for inpatient referrals and 2.3±2.49 for outpatient referrals; t=3.53, df=55, p= .001). No other patient variable was significantly related to total number of appointments. Rates of engagement were significantly higher for inpatient referrals (73 percent, compared with 37 percent for outpatient referrals; χ2 =7.6, df=1, p=.006) and for women (73 percent, compared with 46 percent for men; χ2 =4, df=1, p=.045).
Substance of abuse, psychotic diagnosis, ethnicity, and GAF score were not significantly related to total number of appointments or engagement. There were no significant correlations between engagement and age, length of time since first appointment scheduled, substance abuse versus dependence, or referral from inside versus outside the mental health center.
The logistic regression analysis to predict engagement included referral source (inpatient versus outpatient), substance abused (alcohol versus drugs), sex, ethnicity, diagnosis (psychotic versus nonpsychotic), and all possible two-way interactions of those variables. The resulting model, summarized in Table 1, included referral source, the interaction of referral source and substance abused, and the interaction of substance abused and sex. The model was highly statistically significant (χ2 =23, df=3, p<.001) and correctly classified 73.7 percent of the cases.
In interpreting the interactions, we noted that subjects with a drug diagnosis were significantly more likely to attend three or more appointments if they were referred from inpatient treatment. Of subjects with a drug diagnosis, nine of ten patients referred from inpatient treatment engaged in the dual diagnosis program, compared with one of 12 patients referred from outpatient treatment (χ2 =14.67, df=1, p<.001). However, among subjects with alcohol abuse or dependence, inpatient referrals were no more likely to engage in the dual diagnosis program than outpatient referrals (13 of 20 patients referred from inpatient treatment and nine of 15 patients referred from outpatient treatment were engaged in the dual diagnosis program).
Conversely, outpatient referrals with an alcohol diagnosis were more likely to engage in treatment than those with a drug diagnosis. Of patients referred from outpatient treatment, nine of 15 patients with an alcohol diagnosis engaged in the dual diagnosis program, compared with one of 12 patients with a drug diagnosis (χ2 =7.63, df=1, p=.007). However, among inpatient referrals, patients with an alcohol diagnosis were no more likely than those with a drug diagnosis to engage in the dual diagnosis program (13 of 20 patients with an alcohol diagnosis and nine of ten patients with a drug diagnosis).
A trend was found for the relationship between gender and engagement in treatment for subjects with an alcohol diagnosis. Eleven of 13 female patients with an alcohol diagnosis engaged in the dual diagnosis program, compared with 11 of 22 male patients with an alcohol diagnosis (χ2 = 4.19, df=1, p=.07). However, among patients with a drug diagnosis, female patients were no more likely than male patients to engage in the dual diagnosis program (five of nine female patients and five of 13 male patients engaged in treatment).
Discussion
The reasons for better rates of engagement for the inpatient referrals are not immediately obvious. One plausible explanation is that hospitalization stabilizes patients, making them more amenable to outpatient treatment. Similarly, the interaction of substance and referral source suggests that hospitalization makes a greater difference for patients with drug use disorders. Among inpatient referrals, patients with a drug diagnosis were significantly sicker on admission than those with an alcohol diagnosis (mean±SD GAF scores, 24.36± 7.37 versus 33.13±6.80; t=3.181, df= 55, p=.004). However, the patients with a drug diagnosis improved more during hospitalization, and their mean GAF score was not significantly different from that of the alcohol group at discharge (mean±SD GAF scores, 48.44±9.44 and 47.73± 4.67). Thus inpatient treatment may be necessary to allow patients with drug-related disorders to stabilize enough to engage in outpatient treatment. The effect of sex on engagement, though less robust, is interesting and warrants further study.
This study had several significant limitations, including its retrospective design, small sample size, and use of a single clinical population. Clinical diagnoses were used, and the inpatient and outpatient treatments were not standardized. GAF scores were not available for patients referred from outpatient treatment, so we could not compare the severity of illness for inpatients and outpatients. Finally, the study could not identify the "active ingredient" of inpatient treatment or whether it could be incorporated into outpatient treatment.
Conclusions
Engagement in treatment is one of the major difficulties in treating patients with dual diagnosis. This study found that several patient variables, including referral source, substance of abuse, and sex, were related to patients' engagement in outpatient treatment. Dually diagnosed patients referred from inpatient treatment had a significantly higher rate of engagement. However, this effect was limited to patients with drug use disorders rather than alcohol use disorders. Although the study results should be replicated, they suggest that for dual diagnosis patients with drug use disorders, a brief period of inpatient treatment before referral may enhance engagement in outpatient treatment.
Dr. Bogenschutz is assistant professor of psychiatry and Dr. Siegfreid is a psychiatric resident in the department of psychiatry at the University of New Mexico Medical School in Albuquerque. Address correspondence to Dr. Bogenschutz at the Department of Psychiatry, University of New Mexico Health Sciences Center, 2400 Tucker Avenue, N.E., Albuquerque, New Mexico 87131 (e-mail, [email protected]).
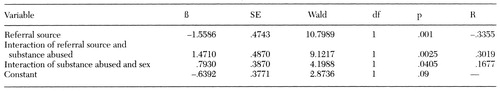 |
Table 1. Logistic regression model of patient variables predicting engagement in outpatient dual diagnosis treatment
1. Regier DA, Farmer ME, Rae DS, et al: Comorbidity of mental disorders with alcohol and other drug abuse. JAMA 264:2511-2518, 1990Crossref, Medline, Google Scholar
2. Drake RE, Wallach MA: Substance abuse among the chronically mentally ill. Hospital and Community Psychiatry 40:1041-1046, 1989Abstract, Google Scholar
3. Owen RR, Fischer EP, Boothe BM, et al: Medication non-compliance and substance abuse among patients with schizophrenia. Psychiatric Services 47:853-858, 1996Link, Google Scholar
4. Ries R, Mullen M, Cox G: Symptom severity and utilization of treatment among dually diagnosed inpatients. Hospital and Community Psychiatry 45:562-568, 1994Abstract, Google Scholar
5. Bowers MB, Mazure CM, Nelson JC, et al: Psychotogenic drug use and neuroleptic response. Schizophrenia Bulletin 16:81-85, 1990Crossref, Medline, Google Scholar
6. Kovasznay B, Fleischer J, Tanenberg-Karant M, et al: Substance use disorder and the early course of illness in schizophrenia and affective psychosis. Schizophrenia Bulletin 23:195-201, 1997Crossref, Medline, Google Scholar
7. Haywood TW, Kravitz HM, Grossman LS, et al: Predicting the "revolving-door" phenomenon among patients with schizophrenic, schizoaffective, and affective disorders. American Journal of Psychiatry 152:856-861, 1995Link, Google Scholar
8. Turner WM, Tsuang MT: Impact of substance abuse on the course and outcome of schizophrenia. Schizophrenia Bulletin 16:87-95, 1990Crossref, Medline, Google Scholar
9. Mueser KT, Bellack AS, Blanchard JJ: Comorbidity of schizophrenia and substance abuse: implications for treatment. Journal of Consulting and Clinical Psychology 60:845-856, 1992Crossref, Medline, Google Scholar
10. Miner CR, Rosenthal RN, Hellerstein DJ, et al: Prediction of compliance with outpatient referral in patients with schizophrenia and psychoactive substance use disorders. Archives of General Psychiatry 54:706-712, 1997Crossref, Medline, Google Scholar



