Case Management and Recidivism of Mentally Ill Persons Released From Jail
Abstract
OBJECTIVE: The study tested the hypothesis that case management provided to mentally ill offenders both in jail and after release from jail would reduce their recidivism. METHODS: A total of 261 inmates of the Lucas County (Toledo, Ohio) jail who were diagnosed with a mental disorder were tracked for three years after their release. The relationships between recidivism and diagnostic, demographic, and case management variables were examined through event history analysis. RESULTS: Recidivism was associated with age, employment, previous arrests, and receipt of community-based case management. Receipt of jail-based case management, although not directly related to recidivism, significantly increased the probability of receiving community-based case management. Receipt of community case management was significantly associated with a lower probability of rearrest and a longer period before rearrest. CONCLUSIONS: This study found hopeful signs that expanding access to case management, both inside and outside jail, will help mentally ill people live in their communities and stay out of jail.
A large number of people with mental illness are confined in jails (1,2,3,4,5,6,7,8,9,10,11,12,13). To decrease the jailing of persons with mental illness, we must understand what types of services could reduce their recidivism. Most research on forensic mental health clients has focused on demographic and diagnostic factors associated with arrest. Youth and a history of arrests (1,14,15,16), as well as personality disorders and substance use disorders (1,3,4), are most consistently found among people with mental illness who are arrested.
However, beyond suggesting a need for substance abuse treatment, research has provided little guidance for interventions to reduce criminal behavior by mentally ill people. Only one major, recent study examined the effect of community mental health treatment services on postincarceration recidivism. Solomon and associates (17) investigated the effect of intensive case management, with and without a special treatment team, and the usual system of community mental health care on the six-month recidivism of homeless mentally ill people leaving jail. They found no significant difference in recidivism between recipients of the three treatments.
The study reported here examined the relationship between the intensity of case management and the criminal recidivism of 261 mentally ill persons released from jail and tracked for three years. We hypothesized that after demographic, criminal history, and diagnostic variables were controlled, recidivism would be inversely related to the amount of case management received both inside and outside jail.
Methods
Study site
In 1989 the Lucas County Sheriff's Office and Mental Health Board in Toledo, Ohio, formed the Lucas County jail mental health project to improve services to jail detainees with serious mental health problems. Mental health services, including diagnostic assessment, counseling, crisis intervention, psychiatric evaluations, and medication, begin in jail and continue after release. The core service, both in jail and after release, is case management.
As described by the program administrators (18), case management has two primary purposes: to link the client to services in the community that foster independence and to decrease the risk of recidivism and the likelihood of psychiatric hospitalization. A team of case managers from the community mental health centers who are based at the jail contact mentally ill inmates and begin community re-entry planning. They establish rapport and trust with inmates and provide additional stability in their lives. They educate and help clients understand the criminal justice system and use of mental health services. They educate attorneys and court personnel about clients' needs and disabilities. Case managers link clients to services in the community and prepare appropriate treatment plans, including housing, medication, and follow-up appointments.
When clients are released from jail, they are referred to community-based case managers, who help them follow through with treatment plans, including medication maintenance and access to needed community support services. They also assist clients with a transition to the community mental health center and to the designated psychiatrist and case worker, and they provide court follow-up as required.
Sample
The sample included all jail detainees who were evaluated by clinicians at the jail from September 1989 through August 1990 and diagnosed with a DSM-III-R axis I or axis II mental disorder (19) other than or in addition to substance abuse. Detainees were included in the sample if they were released directly after detention in the jail or if they spent a subsequent term of no more than 12 months in another correctional facility.
The sample consisted of 261 subjects, of whom 185 (71 percent) were male. A total of 134 subjects (51 percent) were African American, 116 (44 percent) were white, ten (4 percent) were Hispanic, and one (.4 percent) was in a category "other." Subjects' mean±SD age was 30±8.9 years, and the mean±SD education level was 11±1.8 years. Only 63 subjects (24 percent) reported being employed immediately before arrest. The median income of the census tracts where subjects resided before arrest was $16,931.
Subjects had a mean±SD of 14.9± 18.6 previous criminal charges, including 9.3±15.3 nonviolent misdemeanors, 2.3±3.3 violent misdemeanors, 2.3±3.6 nonviolent felonies, and 1±1.5 violent felony. A total of 125 subjects (48 percent) had previous psychiatric hospitalizations, and 63 (24 percent) were actively psychotic at jail admission.
The largest DSM-III-R diagnostic category was personality disorder (86 subjects, or 33 percent), followed by schizophrenia (58 subjects, or 22 percent), and affective disorder (45 subjects, or 17 percent). The remaining 72 subjects (28 percent) mostly had adjustment disorders. Most subjects also had a co-occurring substance use diagnosis. Of the subjects with a personality disorder, 62 (72 percent) also had a substance use diagnosis; this figure was 31 (69 percent) for those with affective disorder, 20 (35 percent) for those with schizophrenia, and 40 (56 percent) for those with all other diagnoses.
Procedures
Whenever a jail-based case manager provided service to a subject, the case manager recorded the date and the amount of service provided (in minutes). Community-based case managers, employed at four different agencies, recorded the same information. Each agency then provided a summary of case management services, including the subject's name, date of service, and amount of service for each meeting between a case manager and a subject. These service records were then compiled into one computer data file.
The period each subject remained in the community without rearrest and the charges associated with rearrests were determined from police records. Recidivism was operationally defined as rearrest within Lucas County. Although most subjects continued to reside in Lucas County after release from jail, a few may have moved elsewhere and been rearrested, which would have led to an undercount of rearrests in this study.
Analysis
Recoding of key variables.
The distributions of several variables ranged widely and were severely skewed, violating the assumption of normality required by regression analysis. The income variable was one such variable. No information on the income of each subject was obtained; therefore, the U.S. census report of median annual income in the census tract where each subject resided was used as an indicator of each subject's income. Because the distribution of median census tract annual incomes was severely skewed, this variable was recoded into five levels: less than $5,000, $5,000 to $14,999, $15,000 to $19,999, $20,000 to $29,999, and $30,000 or more, producing roughly equal pentiles (that is, each category included about one-fifth of the subjects).
The distribution of receipt of community case management was also severely skewed—71 percent of all subjects received no community case management and a few subjects received more than 100 hours. In one model it was recoded as dichotomous (any case management versus none). In other models it was recoded as ordinal (none, one minute to less than two hours, two hours to less than 20 hours, 20 to 100 hours, and more than 100 hours). The logic behind this classification was to divide subjects who had received community case management into roughly equal quartiles.
Community case management time was treated in two ways—cumulatively (the total received over the entire follow-up period) and based on average intensity (the total amount of community case management in minutes averaged over all the months at risk of rearrest). Because the distribution of intensity was highly skewed and widely dispersed, it was collapsed into five categories based on the amount received per month (none, one to 15 minutes, 16 to 59 minutes, one to four hours, and more than four hours). Again, the logic of classification was to divide subjects who received community case management into approximately equal quartiles of service intensity.
Preliminary correlation analysis revealed only low correlations among most of the explanatory variables, eliminating the potential problem of multicollinearity. Thus all variables could be included in one regression model. An important exception was the indicators of severe mental illness. Three of these variables—actively psychotic on admission, severely mentally disabled, and a diagnosis of schizophrenia—were highly correlated. Thus only the actively psychotic variable was used in regression analyses. (Severely mentally disabled is a legal classification applied in Ohio on the basis of diagnosis, duration of illness, and functioning level.)
Event history analysis.
Cases in the original data set were "time-censored" by either the occurrence of an arrest or the expiration of the 36-month follow-up period. Time-censoring seriously biases parameter estimates when standard linear or logistic regression procedures are applied. Therefore, the relative impact of multiple variables on rearrest was evaluated through event history analysis (20,21). This procedure involved first transforming the original data file for the 261 cases into a "person-month" file, in which each case was composed of all the data associated with one subject in a single month after his or her release from jail.
Because the follow-up period was three years, data about each subject occupies from one to 36 cases in the person-month file; the last case for a subject represents the month in which that subject was rearrested or the end of the follow-up period if the subject was not rearrested. A separate person-month file was similarly created for the analysis of rearrest for a violent offense. These person-month files were then analyzed using SPSS logistic regression procedures.
Results
Case management services
A total of 203 subjects (78 percent) received some case management services in jail. The median total amount of services they received was 40 minutes, with two-thirds receiving less than an hour and 15 percent receiving more than two hours.
Case management fell off dramatically after subjects left jail. As Table 1 shows, only 75 subjects (29 percent) received any community case management in the three years after release. Whether a subject received community case management was determined by both the subject's receptiveness and the program offerings of the community mental health center serving the subject's area of residence. Receipt of case management after release from jail was voluntary. Furthermore, the percentage of subjects receiving community case management declined over time, from 27 percent the first year to 15 percent the second year and 10 percent the third year.
The amount of case management services subjects received was recorded until their first arrest after release. Each month a subject was in the community (before the first arrest) constituted one person-month at risk of arrest. Hypothetically, therefore, if all 261 subjects avoided arrest over the entire three-year study period, they would have accumulated a total of 9,396 person-months at risk (261 subjects × 36 months). Because some of the subjects were arrested, however, the number of person-months at risk was 4,454.
Recipients of community case management
Compared with subjects who did not receive community case management, recipients of community case management were significantly younger (29 versus 32 years; F=8.814, df=260, p<.01) and more likely to be legally classified as severely mentally disabled (34 percent versus 15 percent; χ2 =8.395, df=1, p<.01). Recipients were also more likely to have psychotic symptoms on admission to jail (62 percent versus 18 percent; χ2 =44.616, df=1, p<.001), to be diagnosed as having schizophrenia (66 percent versus 19 percent; χ2 = 45.880, df=1, p<.001), to have previous psychiatric hospitalizations (44 percent versus 15 percent; χ2 =25.612, df=1, p<.001), and to have been found not competent to stand trial (60 percent versus 28 percent; χ2 =4.963, df=1, p<.05). (It should be noted that in the jurisdiction where the study was conducted, defendants who are found incompetent to stand trial typically are transferred briefly to a local state psychiatric hospital and then back to jail.)
In addition, subjects who had more severe disorders, as measured by each of the indicators listed above, received far more community case management services, on average, than did subjects whose disorders were less severe.
Typically, the most recent arrest of subjects who received community case management was for a violent misdemeanor (34 subjects, or 45 percent). They had fewer previous felony arrests than those who did not receive community case management (2.5 versus 3.7 arrests; F=4.384, df=260, p<.05) but longer pretrial jail stays (means=47 and 33 days; F=5.399, df=260, p<.05).
Subjects released from jail on probation (to community supervision immediately after conviction) or parole (to community supervision after serving a term in jail after conviction) were equally likely to receive community case management as subjects released directly to the community.
Recidivism
During the follow-up period, 188 of the 261 subjects (72 percent) were rearrested. Among those with the most serious charges, 60 (23 percent) were arrested for violent misdemeanors, 50 (19 percent) for nonviolent felonies, 36 (14 percent) for nonviolent misdemeanors, 29 (11 percent) for violent felonies, and 13 (5 percent) for parole or probation violations. Rearrest typically occurred quickly; 107 subjects (41 percent) were rearrested within six months, and 138 (53 percent) were arrested within one year.
As shown in Tables 2 and 3, subjects who were nonwhite, unemployed, and younger were significantly more likely than other subjects to be rearrested for any offense. Subjects were significantly more likely to be rearrested for a violent offense if they were younger, were nonwhite, did not have an affective disorder, had a personality disorder, and had a more extensive criminal history. These differences in rearrest by age, race-ethnicity, employment status, and previous criminal record are also found in the general population (14).
Subjects who received jail case management were equally as likely as subjects who received none to be arrested for any offense (72 percent and 72 percent, respectively) or a violent offense (65 percent and 67 percent, respectively). However, recipients of community case management were significantly less likely than nonrecipients to be arrested for either any offense (60 percent versus 77 percent; χ2 =7.561, df=1, p<.01) or a violent offense (52 percent versus 71 percent; χ2 =8.512, df=1, p<.05).
Figure 1 shows the recidivism of the subjects categorized by whether they received case management in jail and whether they subsequently received case management in the community. A significant association was found between receipt of jail case management and receipt of community case management (χ2 =30.069, df= 1, p<.001). Figure 1 shows that only subjects who received jail case management subsequently received community case management. As noted above, a significant association was also found between receipt of community case management and avoidance of rearrest. Subjects who received community case management were less likely to be rearrested than subjects who received no case management.
Not only were recipients of community case management less likely to be arrested but they also remained in the community longer before rearrest than subjects who received none (mean of 21 months in the community versus 14 months; F=12.369, df=1, p<.001).
Figure 2 shows the survival rates of subjects categorized by whether they received community case management. Survival rates reflect the proportion of subjects not yet arrested at each month after release. The figure shows clearly that the relationship between receipt of community case management and first arrest was strongest during the first year, after which approximately equal proportions of recipients and nonrecipients were arrested for the first time.
Three logistic regression models were computed in the event history analysis, which is shown in Table 4. In model 1 the community case management variable was excluded. In model 2 community case management was included as a dichotomous variable (any case management versus no case management). In model 3 the intensity of community case management (mean amount received per month) was entered as a categorical variable. Models A1, A2, and A3 all include rearrest for any offense. Models V1, V2, and V3 are limited to rearrest for a violent offense.
Model A1, which included 911 subjects but excluded the community case management variable, fit the data well, as shown in Table 4 by the significance of the -2 log likelihood chi square test and the goodness of fit statistic (see Yamaguchi [21] for a full discussion of significance tests appropriate to event history analysis). The variables age, race, employment status, income level, and total charges in the criminal history were significantly related to the odds of rearrest for any offense. These same variables remained significant whether or not community case management was added to the analysis of arrest for all offenses in models A2 and A3 and for violent offenses in models V1, 2, and 3.
Model A2 also fit the data well. Introducing the variable of any community case management in model A2 significantly added to the explanatory power of the original variable set. The difference between -2 log likelihood chi square values of model A2 and model A1 is 9.050 (df=1, p<.05). Furthermore, receiving community case management was associated with a 45 percent decrease in the probability of rearrest.
Model A3, which included intensity of community case management as a categorical variable, was also a good fit. Including this variable added significant explanatory power to model A1. The difference between -2 log likelihood chi square values of model A3 and model A1 is 26.425 (df=4, p<.001). The odds of rearrest were less for subjects receiving either one to 15 minutes or 16 to 59 minutes of case management a month than for subjects who received none. However, receipt of more than 60 minutes a month of community case management did not further reduce the likelihood of recidivism.
Arrest for a violent offense
Table 4 also shows three logistic regression models computed to predict rearrest for a violent offense. Model V1, which included all subjects but excluded the community case management variable, fit the data well. Model V2, in which community case management was included as a dichotomous variable, was also a good fit. Receipt of any community case management reduced the odds of violent recidivism by 64 percent. Model V2 was a significant improvement over model V1. The difference in -2 log likelihood chi square values is 15.878 (df=1, p<.05).
Model V3, which included the four dummy variables of intensity of case management, was also a good fit, and an improvement over model V1. The difference in -2 log likelihood chi square values between the two models is 13.989 (df=4, p<.001). Subjects receiving either one to 15 minutes or 16 to 59 minutes of case management per month had a lower probability of recidivism for a violent offense than subjects receiving no community case management. However, receiving more than 60 minutes per month did not significantly reduce the likelihood of violent recidivism.
Recidivism and income
A positive relationship between income (as measured by the median income of the census tract where subjects resided) and recidivism appeared consistently in the regression models. No obvious explanation exists for this finding. It may be an artifact of the income measure, which was probably an unreliable indicator of subjects' income, given the high rate of unemployment among the subjects. This unexpected relationship may also indicate the level of tolerance of deviant behavior—and the responsiveness of police to complaints about deviant behavior—by mentally ill neighbors.
Discussion
The study's findings of an association between age, arrest history, and recidivism are consistent with those of previous research on factors affecting the arrest of persons with mental illness (1,3,14,15,17,22). The unique finding of this study is the identification of a significant association between the quantity of case management services received and a reduction in recidivism, which previous research (22) did not find.
Continuity of care
The study found a strong relationship between receiving jail-based case management services and receiving community case management services. Failing to receive jail-based case management ensured that a mentally ill jail inmate would not receive community-based case management.
The finding that probation or parole supervision did not increase the probability of receiving community case management is troubling. The circumstances under which mentally ill parolees and probationers are likely to get this service should be explored in future studies.
Reduction of recidivism
The relationship between receipt of jail-based case management and a reduction in recidivism appears to be indirect. To receive community case management, subjects must first have received jail case management; subjects who received community case management were less likely to be rearrested than those who did not. Furthermore, recipients of community case management remained in the community longer before rearrest than those who received no case management. These findings support a policy of expanding the availability of jail- and community-based case management.
The relationship between the amount of community case management services received and the probability of recidivism was not linear. Although receipt of some community case management was associated with a significant reduction in recidivism, receipt of the greatest intensity of case management was not.
Interpretive considerations
Jail inmates with the most severe mental disorders—those most in need of mental health treatment—were more likely to receive community case management, and to receive more of it. This finding is reassuring: subjects with the greatest need were most likely to get services. However, this fact was troublesome to the analysis, because it did not permit us to definitively test the effect of case management across all levels of disability. The most needy subjects were more likely to get services, but they were also more likely to have problems in living, some of which result in criminal recidivism. Although the study showed a clear association between receipt of case management and a reduction in recidivism, the research design did not permit a causal inference from this association.
Conclusions
Focusing on the quantity of case management services provided to mentally ill jail inmates has revealed an important aspect of how case management affects their lives. Although further research is clearly needed, this study found hopeful signs that expanding access to case management, both inside and outside jail, will help mentally ill people live in their communities and stay out of jail.
Journal Seeks Short Items About Novel Programs
Psychiatric Servicesinvites short contributions for Innovations, a new column to feature programs or activities that are novel or creative approaches to mental health problems. Submissions should be between 350 and 750 words. The name and address of a contact person who can provide further information for readers must be listed.
A maximum of three authors, including the contact person, can be listed. References, tables, and figures are not used. Any statements about program effectiveness must be accompanied by supporting data within the text.
Material to be considered for Innovations should be sent to the column editor, Francine Cournos, M.D., at the New York State Psychiatric Institute, 1051 Riverside Drive, Unit 112, New York, New York 10032. Dr. Cournos is director of the institute's Washington Heights Community Service.
Acknowledgment
The study was funded by the Ohio Department of Mental Health.
Dr. Ventura is director of inmate services at the Lucas County Sheriff's Office, 1622 Spielbusch Avenue, Toledo, Ohio 43624. Dr. Cassel is clinical director of Harbor Behavioral Health Care in Toledo. Dr. Jacoby is associate professor in the department of sociology at Bowling Green State University in Bowling Green, Ohio. Dr. Huang is research associate with the Social Research Development Group of the School of Social Work at the University of Washington in Seattle. Results of the study were presented at a conference on state mental health agency services research and program evaluation held February 11-13, 1996, in Arlington, Virginia.
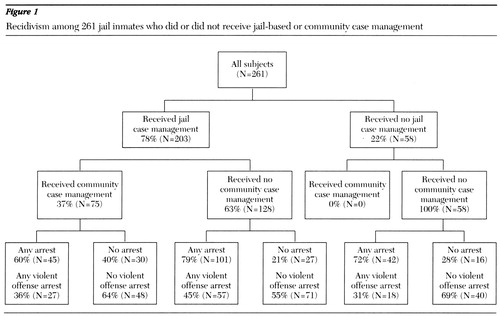
Figure 1. Recividism among 261 jail inmates who did or did not recieved jail-based or community case management
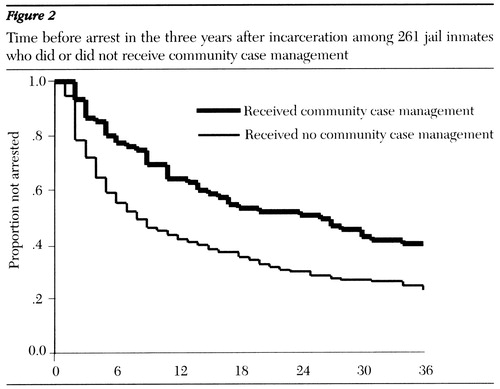
Figure 2. Time before arrest in the three years after incarceration among 261 jail inmates who did or did not receive community case management
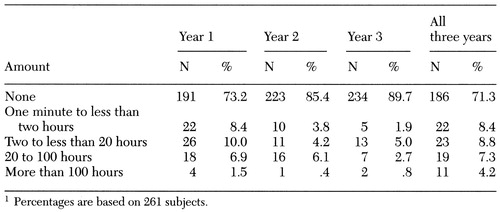 |
Table 1. Recipients of community case management and total amount of case management received among 261 jail inmates in the three years after release from incarceration1
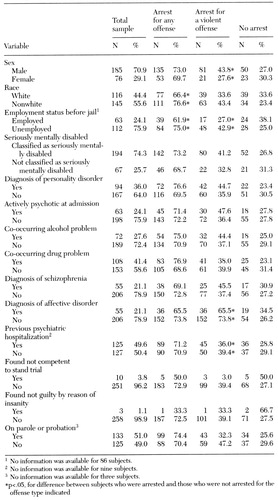 |
Table 2. Recidivism among 261 jail inmates in the three years after release from incarceration by demographic and clinical variables
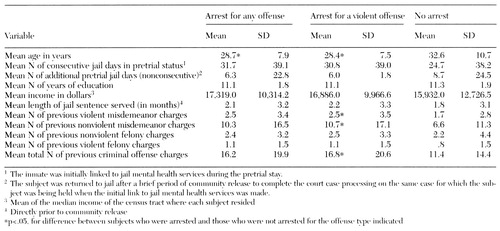 |
Table 3. Recidivism among 261 jail inmates in the three years after release from incarceration, by age and by criminal history variables
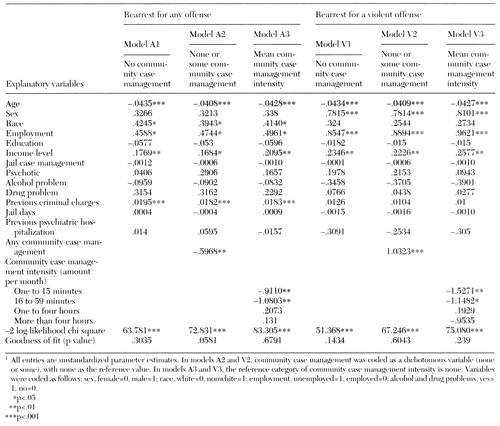 |
Table 4. Event history models of likelihood of rearrest for any offense and for a violent offense among 261 jail inmates in the three years after release from incarceration
1. Draine J, Solomon P, Meyerson A: Predictors of reincarceration among patients who received psychiatric services in jail. Hospital and Community Psychiatry 45:163-167, 1994Abstract, Google Scholar
2. Guy E, Sauer R, White V: Mental health status of prisoners in an urban jail. Criminal Justice and Behavior 12:29-53, 1985Crossref, Google Scholar
3. Holcomb W, Ahr P: Arrest rates among young psychiatric patients treated in inpatient and outpatient settings. Hospital and Community Psychiatry 39:52-57, 1974Google Scholar
4. McFarland B, Faulkner J, Bloom J, et al: Chronic mental illness and the criminal justice system. Hospital and Community Psychiatry 40:718-723, 1989Abstract, Google Scholar
5. Morgan C: Developing mental health services for local jails. Criminal Justice and Behavior 8:259-274, 1981Crossref, Google Scholar
6. Teplin LA: Mental Health and Criminal Justice. Beverly Hills, Calif, Sage, 1984Google Scholar
7. Teplin LA: Detecting disorder: the treatment of mental illness among jail detainees. Journal of Consulting and Clinical Psychology 58:233-236, 1990Crossref, Medline, Google Scholar
8. Steadman H, McCarty D, Morrisey J: The Mentally Ill in Jail. New York, Guilford, 1989Google Scholar
9. Abramson M: The criminalization of mentally disordered behavior: possible side effects of a new mental health law. Hospital and Community Psychiatry 23:13-17, 1972Medline, Google Scholar
10. Adler F: Jails as a repository for former mental patients. International Journal of Offender Therapy and Contemporary Criminology 30:225-236, 1986Crossref, Google Scholar
11. Belcher J: Are jails replacing mental health systems for the homeless and mentally ill? Community Mental Health Journal 23:185-195, 1988Google Scholar
12. Whitmer G: From hospital to jails: the fate of California's deinstitutionalized mentally ill. American Journal of Orthopsychiatry 50:65-75, 1980Crossref, Medline, Google Scholar
13. Torrey EF, Stieber J, Ezekiel J, et al: Criminalizing the Seriously Mentally Ill. Washington, DC, Public Citizen's Health Research Group and the National Alliance for the Mentally Ill, 1992Google Scholar
14. Harry B, Steadman H: Arrest rates of patients treated at a community mental health center. Hospital and Community Psychiatry 39:862-866, 1988Abstract, Google Scholar
15. Sosowsky L: Explaining the increased arrest rate among mental patients. American Journal of Psychiatry 137:1602-1605, 1980Link, Google Scholar
16. Schellenberg GE, Wasylenki D, Webster CD: A review of arrests among psychiatric patients. International Journal of Law and Psychiatry 15:251-264, 1992Crossref, Medline, Google Scholar
17. Solomon P, Draine J, Meyerson A: Jail recidivism and receipt of community mental health services. Hospital and Community Psychiatry 45:793-797, 1994Abstract, Google Scholar
18. Finn-Will H, Turner P, Ventura LA: Mental health case management services in a correctional setting. Jail Suicide/Mental Health Update 6(3):16-18, 1996Google Scholar
19. Diagnostic and Statistical Manual of Mental Disorders, 3rd ed, rev. Washington, DC, American Psychiatric Association, 1987Google Scholar
20. Allison PD: Event History Analysis: Regression for Longitudinal Event Data. Beverly Hills, Calif, Sage, 1984Google Scholar
21. Yamaguchi K: Event History Analysis. Newbury Park, Calif, Sage, 1991Google Scholar
22. Draine J, Solomon P: Jail recidivism and the intensity of case management services among homeless persons with mental illness leaving jail. Journal of Psychiatry and Law 22:245-261, 1994Crossref, Google Scholar



