Datapoints: HIV Infection Linked to Substance Use Among Hospitalized Patients With Severe Mental Illness
Last June the National Institute of Mental Health adopted new priorities to address the AIDS epidemic among people with severe mental illness. Besides prevention and treatment, the priorities emphasize the need for a fuller understanding of the extent and social organization of sexual and drug use behavior, the nationwide prevalence of HIV, and the nature of causality between mental illness and HIV infection (1).
Eleven studies of 2,873 predominantly hospital-based psychiatric patients in New York City, Baltimore, and Columbia, South Carolina, indicate the average HIV infection rate among adults with severe mental illness is 7.8 percent (2), nearly 20 times the rate of .4 percent estimated for the general population (3). Across studies, psychiatric patients with identified comorbid alcohol or other drug use disorders have a significantly higher rate of infection than those without (χ2 =47.56, df=9, p<.001) (see Figure 1). Among patients treated on dual diagnosis units, HIV seroprevalence is significantly related to type of substance used (χ2 =8.82, df=2, p<.03) (see Figure 2).
Drug injection confers the highest risk, but even use of noninjected drugs or alcohol alone resulted in rates of infection substantially higher than the average rate. Patients with alcohol or other drug use disorders may be members of social networks where sex and drugs combine to create vulnerability to sexually transmitted HIV infection.
Mental health care providers are often in the best position to assess patients' sexual and drug use behaviors. Only by asking can providers learn their patients' HIV-related risks and service needs and appropriately address them to reduce the human and economic costs of the AIDS epidemic.
Acknowledgments
This work was supported by the New York State Office of Mental Health and the Center for Mental Health Services.
The authors are affiliated with the department of psychiatry at Columbia University College of Physicians and Surgeons and the New York State Psychiatric Institute. Send correspondence to Ms. McKinnon at 722 West 168 Street, Unit 112, New York, New York 10032 (e-mail [email protected]). Harold Alan Pincus, M.D., and Terri L. Tanielian, M.A., are coeditors of this column.
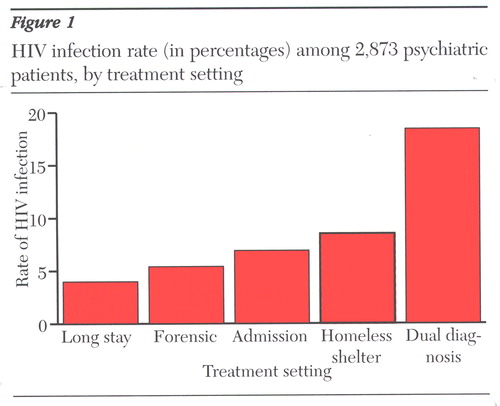
Figure 1. HIV infection rate (in percentages) among 2,873 psychiatric patients, by treatment setting
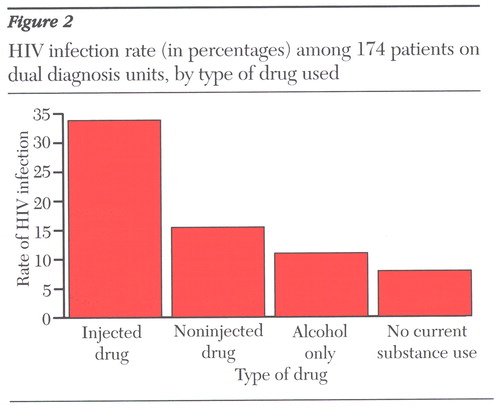
Figure 2. HIV infection rate (in percentages) among 174 patients on dual diagnosis units, by type of drug used
1. McKinnon K, Carey MP, Cournos F: Research on HIV, AIDS, and severe mental illness: recommendations from the NIMH national conference. Clinical Psychology Review 17:259-269, 1997 Crossref, Medline, Google Scholar
2. Cournos F, McKinnon K: HIV seroprevalence among people with severe mental illness in the United States: a critical review. Clinical Psychology Review 17:259-269, 1997 Crossref, Medline, Google Scholar
3. Steele FR: A moving target: CDC still trying to estimate HIV-1 prevalence. Journal of NIH Research 6:25-26, 1994 Google Scholar



