Portland Identification and Early Referral: A Community-Based System for Identifying and Treating Youths at High Risk of Psychosis
Psychotic disorders represent a major and continuing burden to public health and society, often imposing disability for a lifetime. Early identification and treatment of psychosis may be necessary to prevent deterioration and treatment resistance ( 1 ).
Results of early intervention trials and improvements in identification methods indicate that treatment during the period preceding frank psychosis may prevent severe outcomes ( 2 ). Four clinical trials have found that onset of psychosis can be limited to less than half the expected rate with antipsychotic medication, family psychoeducation, and assertive community treatment or cognitive therapy ( 3 , 4 , 5 , 6 ). Across the four samples, 37 first episodes occurred among 110 untreated persons in control groups (34%), whereas 16 occurred among 134 persons who received treatment (12%). The National Prodromal Longitudinal Study recently demonstrated that selected clinical criteria and family history can predict onset of psychosis in 34% to 81% of cases ( 7 ).
In 2000 the Portland Identification and Early Referral (PIER) program undertook systematic early detection, intervention, and prevention of psychosis within a defined catchment area. The intent was to reduce the incidence of psychotic disorders by indicated (secondary) prevention—that is, by providing treatment during the period of illness before manifest onset of psychosis. Established in Portland, Maine, the identification, assessment, and treatment program built on features developed in Buckingham, United Kingdom ( 8 ), and refined in Melbourne, Australia ( 4 ); four sites in North America ( 3 ); Stavanger, Norway ( 9 ); and Denmark ( 6 ). This report describes the community education and identification methods, as well as identification and referral rates, during the first six years of operations, from 2001 to 2007.
Methods
This initiative attempted to identify and treat all consenting persons with prodromal psychosis in the greater Portland community who were between 12 and 35 years old. To identify those at risk early enough to prevent onset, the PIER program developed, educated, and trained a wide referral network, implemented a public education campaign, and operated a special multidisciplinary team to treat young people at high risk of psychosis. Unlike most other psychosis prevention programs, the initial focus of the PIER team's effort was on educating and training counseling and health care professionals working in schools and colleges, community-based primary care and pediatric physicians, mental health clinicians, and clinic and agency staff serving youths and young adults. In May 2001, the team began to assess, accept, and treat individuals referred from those sources.
The experimental catchment area included 25 towns surrounding and including the city of Portland, a relatively stable and largely homogeneous population, with recent immigrants adding a degree of cultural diversity. The target population numbered 333,000 by 2007. Outreach, education, and training by the PIER staff was intended to reduce stigma, share information about current concepts of brain function in psychotic disorders, convey knowledge of the key signs of prodromal psychosis, and establish willingness and procedures for rapid referral. To those ends, the PIER clinical staff spent much of the first year making on-site visits with professional groups most likely to observe prodromal symptoms among youths early enough to avert onset. Outreach and education continued during the study reported here. Standardized educational material for each professional sector was developed with the assistance of a social marketing and design agency. Engagement with each referring group required tailored, sometimes multipronged, approaches. In addition to presentations in professionals' offices, professional educational sessions were held for groups of 50 to 200 (for example, grand rounds presentations or meetings of public school professionals).
A public education campaign conducted in parallel focused on parents, other relatives, and friends of young people to ensure that they would better understand mental illness, recognize its early symptoms, and seek treatment. It used commercial and public service radio and television announcements, participation in local radio and television talk shows, and the creation and distribution directly to youths of easy-to-read bookmarks, brochures, and flyers. Two PIER Web sites were established to provide information anonymously, one for youths and the general public ( www.preventmentalillness.org ) and one for professionals ( www.stopmentalillness.com ). The PIER program's research design and procedures were approved by the Maine Medical Center Institutional Review Board.
The PIER clinical team was available for consultation and rapid response to requests for assessment and treatment. Anonymous telephone consultations were encouraged to avoid delays and to reduce barriers to referral and early intervention. Clinical contacts with the young person or family could occur at locations deemed acceptable by the participants, such as the office of the general practitioner or school guidance counselor, the family home, or the PIER clinic. Identification of the PIER clinic as a mental health service was explicitly avoided.
Referrals were screened by PIER clinical staff, usually by telephone, for basic demographic and clinical criteria—residence in the catchment area, aged between 12 and 35, no prior psychotic episode, and evidence of prodromal psychotic symptoms. All referrals were tracked, and information was recorded by intake clinicians to identify the sector of the referring person (for example, educational, medical, or mental health), the town of origin of the referral, the age and gender of the referred individual, and disposition after screening. Individuals who met criteria for psychosis were excluded from the study and referred directly to clinical services in the community, which rarely included hospitalization. Those who were judged to need clinical intervention for other disorders were referred to community clinicians.
If PIER staff agreed that an individual seemed to be at high risk, he or she received a formal assessment with the Structured Interview for Prodromal Syndromes (SIPS) ( 10 ) after informed consent was obtained from all participating family members. Those at risk met one of two criteria sets: either they had attenuated psychotic symptoms as determined by the Symptoms of the Prodromal Syndrome scale (SOPS) or they met DSM-IV schizotypal personality criteria or had a first- or second-degree relative with a psychotic disorder along with a 30% decrease in the Global Assessment of Functioning score. This method has been found to adequately predict risk of onset of psychosis within 30 months after assessment ( 7 , 11 ). Agreement with a criterion rater for presence of the prodromal syndrome among all interviewers was 88% ( κ =.778, p<.001).
The goal of intervention was to prevent the onset of psychosis. The treatment approach, a prodromal version of Family-aided Assertive Community Treatment, was provided for two years ( 12 , 13 ). It comprised family psychoeducation, supported employment and education, key elements of assertive community treatment, and psychiatric medication—all evidence-based practices for schizophrenia and other psychotic disorders. Antipsychotic medication was prescribed only for persistent or increasingly severe prodromal psychotic symptoms.
Outcome measures specific to outreach efforts included the number of educational events and number of professionals who received education and training, number of referrals, association between number of professionals who received education in a given quarter-year with number of referrals in subsequent quarters, and number and proportion of persons referred who consented, were formally assessed, and met criteria for being at risk. To test the association between training effort and referrals, the number of training events and the number of referrals were aggregated within quarter-years and analyzed for associations by using zero-order correlations. Lagged regression analysis was used to test whether training events at one point in time affected future referral rates.
Results
During the six-year study period, 7,270 key professionals and students attended 325 separate events (approximately one event one per week). Training sessions were held at all of the public and private high schools, all colleges and universities, and all public middle schools; at most sites sessions were held at least twice to address staff turnover. A total of 944 contacts were made with medical professionals via office visits, grand rounds presentations, and local medical conferences. Other groups that received training included the medical and mental health staff of military bases, youth and adult correction facility staff, police with special mental health training, family law judges, legal assistants, foster care social workers, and some local clergy and rabbis. Altogether, 74% of the participants in the professional education effort were from outside the mental health and tertiary medical sectors. More than 100 events and 1,896 contacts involved mental health professionals.
Figure 1 illustrates the distribution and disposition of all contacts with PIER intake staff from May 7, 2001, to September 1, 2007. A total of 1,103 individuals were referred. Almost all were screened by telephone. Reflecting the rank order of effort in terms of community educational venues and audiences, the category that accounted for the largest proportion of referrals was mental health sources (N=204, 26%), followed by the families category (N=185, 24%) and schools category (N=158, 20%). Most of the family referrals were from schools. More than half of the referrals (N=408, 52%) were from persons outside the mental health system: family members, education professionals, general medical personnel, and self-referred. Other referring groups included the medical staff of military bases, youth correction facility staff, police with special mental health training, family law judges, foster care social workers, and clergy.
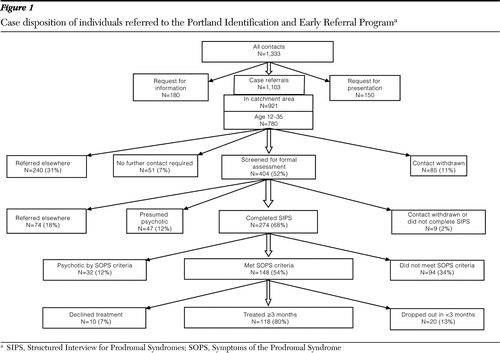
As shown in Figure 1 , of 780 individuals who met eligibility criteria, 52% were recommended for formal assessment or for rapid referral because of the presence of psychosis. Of those, 68% were assessed, and of those assessed, 54% met SOPS criteria for having a prodromal syndrome. Thus 37% of the presumed prodromal youths who were identified and referred to the PIER program and screened by PIER staff met prodromal criteria by the SIPS and SOPS structured interview and scoring system. The mean±SD age of the 148 youths was 16.5±3.1 years; 78 (53%) were males, and 70 (47%) were females. Nine (.6%) were African American, three (2%) were Asian American, three (2%) were Latino American, one (1%) was Native American, three (2%) were from other racial-ethnic groups, and 129 (87%) were European American. Of the 148 youths, ten declined treatment after giving informed consent.
As a measure of the efficiency of early identification, nearly two of five youths (37%) referred to PIER and screened by PIER staff were found to be at risk of psychosis. The screening process identified a substantial number (N=79, 20%) who had untreated or early psychosis, and they were quickly referred for treatment, usually without hospitalization. Therefore, the overall efficiency of the process was 57%—youths found to have early psychosis and those who met prodromal criteria. When those referred for treatment of nonpsychotic disorders were included, the efficiency ratio was 75%.
Finally, we tested whether the number of outreach events at a given point in time was associated with the number of referrals received. A regression model with number of events lagged by two quarters explained a significant amount of variance in future referrals (F=5.36, df=2 and 21, p=.013). The number of events two quarters earlier had a positive effect on the number of referrals (b=.971, t=5.61, df=1, p<.02). The number of referrals two quarters earlier was also negatively associated with the number of later referrals (b=–.429, t=–2.29, df=1, p<.04), suggesting a referral pattern that is seasonal, which confirms clinical experience.
Discussion
The PIER program is a public health initiative that implemented an indicated strategy to prevent psychosis in its earliest phase. Over six years, we educated a large proportion of professionals who were in frequent contact with the population at highest risk of a psychotic disorder. The PIER staff consulted with them about specific young people and assessed and treated those found to be at risk. The results of the education and identification components of the PIER system support the conclusion that such an approach is at least feasible in an ordinary urban context. Intakes began in May 2001, after an initial community education and training campaign. Fifty-seven percent of referred youths either met criteria for being at high risk of psychosis or were found to be in a very early stage of frank psychosis. More than half of those who made referrals were not mental health professionals. PIER community and professional education had a lagged effect on referrals of about six months. Thus early interventionists should anticipate this lag for outreach activities to be effective, with substantial seasonal variation.
To our knowledge there is no standard of efficiency for indicated prevention programs. However, the PIER program's rate of 37% confirmed prodromal cases—57% when youths with early psychosis are included and 75% when those likely to have other psychiatric disorders are added—is comparable to another recent prevention initiative. In a recent study at 23 schools, 72% of 530 students who were initially assessed by trained school professionals were confirmed to be at risk of a mental health problem ( 14 ). In the ÆSOP study of psychosis incidence (Aetiology and Ethnicity of Schizophrenia and Other Psychoses), the rate in Bristol, England, for those under age 35 was 15.4 per 100,000 persons ( 15 ). Our findings indicate that the comparable rate in Portland for prodromal and early psychotic cases combined was 10.8 per 100,000 persons. Thus the PIER program identified 70% of those expected to have an onset of psychosis and 46% during the prodromal period.
The ability of professionals with no formal mental health training to identify early signs of psychosis was tested. They achieved 45% to 50% accuracy. Unlike mental health professionals, those in the education, medical, clerical, and military sectors observe youth longitudinally during the age of risk. Thus they are likely to be more accurate in their estimation of key variables—gradual deterioration in occupational and social functioning and increasing severity of subtle psychotic symptoms.
A limitation of the study is that the outcome measure was confirmation of risk status by a research instrument and criteria (SIPS), which does not necessarily indicate the imminent onset of major psychosis. However, at least a third of individuals identified with this instrument have gone on to develop a psychosis ( 7 ). Some who met these criteria but were not found to be at risk of psychosis had a less serious disorder and were able to receive early treatment.
Conclusions
Depending on the consistency and accuracy of the community response, early signs of an encroaching psychotic disorder can be safely detected by educated professionals and family members. The key is access to well-trained specialists using empirically tested methods for confirming at-risk status and for safe and effective treatment. Further success may lead to the inclusion of psychotic disorders among those that can be prevented by early intervention.
Acknowledgments and disclosures
This study was partially supported by grant R01-MH065367 from the National Institute of Mental Health and grants from the Robert Wood Johnson Foundation, Center for Mental Health Services of the Substance Abuse and Mental Health Services Administration, American Psychiatric Foundation, Maine Health Access Foundation, Francis Hollis Brain Foundation, Betterment Fund, Bingham Program, UNUM Foundation, Wrendy Haines Fund, and the State of Maine. Susan Winslow, R.N., and Mary Ellen Thoma, M.H.A., contributed substantially to the development of the PIER Program.
The authors report no competing interests.
1. McGlashan TH, Johannessen JO: Early detection and intervention with schizophrenia: rationale. Schizophrenia Bulletin 22:201–222, 1996Google Scholar
2. Haroun N, Dunn L, Haroun A, et al: Risk and protection in prodromal schizophrenia: ethical implications for clinical practice and future research. Schizophrenia Bulletin 32:166–178, 2005Google Scholar
3. McGlashan TH, Zipurksy RB, Perkins D, et al: Randomized, double-blind trial of olanzapine versus placebo in patients prodromally symptomatic for psychosis. American Journal of Psychiatry 163:790–799, 2006Google Scholar
4. McGorry P, Yung A, Phillips L, et al: Randomized controlled trial of interventions designed to reduce the risk of progression to first-episode psychosis in a clinical sample with subthreshold symptoms. Archives of General Psychiatry 59:921–928, 2002Google Scholar
5. Morrison AP, French P, Walford L, et al: Cognitive therapy for the prevention of psychosis in people at ultra-high risk: randomised controlled trial. British Journal of Psychiatry 185:291–297, 2004Google Scholar
6. Nordentoft M, Thorup A, Petersen L, et al: Transition rates from schizotypal disorder to psychotic disorder for first-contact patients included in the OPUS trial: a randomized clinical trial of integrated treatment and standard treatment. Schizophrenia Research 83:29–40, 2006Google Scholar
7. Cannon TD, Cadenhead K, Cornblatt B, et al: Prediction of psychosis in youth at high clinical risk. Archives of General Psychiatry 65:28–37, 2008Google Scholar
8. Falloon IRH: Early intervention for first episodes of schizophrenia: a preliminary exploration. Psychiatry 55:4–15, 1992Google Scholar
9. Johannessen J, McGlashan T, Larsen T, et al: Early detection strategies for untreated first-episode psychosis. Schizophrenia Research 51:39–46, 2001Google Scholar
10. McGlashan TH, Miller T, Woods S, et al: Structured Interview for Prodromal Syndromes. New Haven, Conn, Yale School of Medicine, 2003Google Scholar
11. Miller TJ, McGlashan TH, Rosen JL, et al: Prodromal assessment with the Structured Interview for Prodromal Syndromes and the Scale of Prodromal Symptoms: predictive validity, interrater reliability and training to reliability. Schizophrenia Bulletin 29:703–715, 2003Google Scholar
12. McFarlane WR, Dushay RA, Stastny P, et al: A comparison of two levels of family-aided assertive community treatment. Psychiatric Services 47:744–750, 1996Google Scholar
13. McFarlane WR, Dushay RA, Deakins SM, et al: Employment outcomes in family-aided assertive community treatment. American Journal of Orthopsychiatry 70:203–214, 2000Google Scholar
14. Nemeroff R, Levitt JM, Faul L, et al: Establishing ongoing, early identification programs for mental health problems in our schools: a feasibility study. Journal of the American Academy of Child and Adolescent Psychiatry 47:328–338, 2008Google Scholar
15. Kirkbride JB, Fearon P, Morgan C, et al: Heterogeneity in incidence rates of schizophrenia and other psychotic syndromes: findings from the 3-center ÆSOP study. Archives of General Psychiatry 63:250–258, 2006Google Scholar



