Recent Changes in the Prevalence of Psychiatric Disorders Among VA Nursing Home Residents
Despite the recognition that nursing homes serve many residents with mental illness, surprisingly little is known about longitudinal changes in the prevalence rates of psychiatric disorders in nursing homes. Better information about the changing mental health needs of the nursing home population is critical for understanding the effect of policy changes, projecting future needs, and ensuring adequate care.
The prevalence of psychiatric disorders in nursing homes is responsive to such factors as the population's age structure, the age structure of psychiatric disorders, and the availability and financing of care. To better understand these factors, several time-dependent effects can be distinguished.
Age effects are associated with developmental processes. Age effects are clear for dementia, which increases with age in incidence and prevalence ( 1 , 2 , 3 ). Age effects are less clear for other psychiatric disorders. For example, in cross-sectional comparisons, older adults report fewer substance use problems than younger adults, but controversy persists as to whether this reflects reduced alcohol consumption with aging or birth cohort and period effects ( 4 , 5 , 6 ).
Period effects result from changing conditions that act across age groups, such as bed availability and financing of care. Deinstitutionalization resulted in some individuals with chronic mental illness being shifted from psychiatric hospitals to nursing homes ( 7 ). Efforts to reduce hospital stays have shifted some post-acute care patients, who are likely to have lower rates of mental health problems, into nursing homes ( 8 ).
Birth cohort effects arise from experiences, such as wartime military service, commonly shared by individuals born within the same time period. Generational effects related to the availability of social support (for example, divorce rates and numbers of children) have an impact on the risk of nursing home admission and, consequently, on residents' mental health profile. Birth cohort and period effects often interact ( 6 ). For example, alcohol availability varies historically (period effect) but may have the greatest impact on young adults' use patterns.
A few longitudinal comparisons have examined levels of psychiatric disorders among nursing home residents. One comparison found that the prevalence of any mental illness among community nursing home residents increased from 44% in 1985 to 58% in 1995, largely as a result of increased dementia and depression, but it also found that nursing homes cared for fewer patients with serious mental illness ( 9 ). A replication of this study methodology found a decline in the prevalence of psychiatric disorders to 53% in 1999 ( 10 ). Another comparison found that the numbers and proportions of first-time nursing home admissions with mental illness increased between 1999 and 2005, largely attributable to increased rates of depression. Rates of anxiety, schizophrenia, and bipolar disorders remained relatively stable, and dementia rates declined over this period ( 8 ).
The Department of Veterans Affairs (VA) operates approximately 130 nursing homes, in which residents are tracked through the use of uniform electronic medical records. Characteristics of VA nursing home residents are strongly influenced by period and cohort effects. Wars and military draft policies help define the age distribution and disability pattern of persons eligible for VA nursing home care. For example, among VA primary care patients seen in fiscal year (FY) 1999, individuals who were aged 45 to 64 (born between approximately 1935 and 1954) were most likely to meet criteria for psychiatric disorders, followed by the younger age group. Those older than 64 years were least likely to meet criteria for most psychiatric disorders ( 11 , 12 ). Thus, as the large Vietnam-era cohort ages and replaces World War II veterans, observers predict consequent shifts in the VA patient profile ( 13 ).
Changes in health care policies act as period effects and influence the characteristics of VA nursing home residents. As in the wider community, the VA moved to reduce inpatient psychiatric beds and hospital length of stay during the 1990s. Coincident with VA inpatient bed reductions, more VA psychiatric patients were discharged to VA nursing homes ( 14 ). VA nursing home surveys found that the proportions of residents with psychiatric disorders were 71% in 1990 and 75% in 1994; rates of dementia, anxiety disorders, and alcohol use disorders were stable, and the prevalence of depressive disorders, schizophrenia and other psychoses, and drug use disorders increased slightly ( 15 ). Other recent changes include increased proportions of VA nursing home residents with short stays ( 16 ) and improved primary care screening for depression ( 17 ), substance use disorders ( 18 ), and posttraumatic stress disorder (PTSD) ( 19 ).
The research objectives of this study were to identify differences in the prevalence of psychiatric disorders among VA nursing home residents overall and in different age groups and birth cohorts and to explore possible age, birth cohort, and period effects that may help account for these differences. Although VA nursing homes differ from community nursing homes in their policies, financial pressures, and resident population (for example, largely men and a younger population), analysis of VA data can identify common trends across settings and serve as a model for studying other care settings.
Methods
This research received institutional review board approval; informed consent was not required. Patients treated in VA nursing homes in FYs 1998, 2002, and 2006 were identified in the VA's National Patient Care Database. To ensure comprehensive information on mental health conditions, residents' diagnoses were obtained from inpatient, outpatient, and extended care records for a three-year period, ending with the year of VA nursing home stay. All ICD-9 codes were considered (up to 13 diagnoses per treatment episode).
Census samples
In order to identify longer-term changes in residents' characteristics, we extended the approach used for the 1990 and 1994 Surveys of VA Nursing Homes (SVANH), which was based on a 20% sample of residents and drew diagnostic information from medical records ( 15 ). We selected census samples for 1998, 2002, and 2006 (residents of the VA nursing homes on the last day of the FY) and used the SVANH psychiatric disorder categories: dementia, schizophrenia, depressive disorders, and alcohol and drug use disorders. We compared psychiatric disorder prevalence in these years and with findings from the 1990 and 1994 SVANH.
Admission samples
We also used administrative data to track changes over time in psychiatric disorder prevalence in VA nursing home admissions. Admissions in 1998 and 2006 were selected from the treated population (the most recent admission was used if there were multiple admissions). Residents in the admission sample are likely to have more complete diagnostic information from inpatient and outpatient care preceding admission, data that are not available for long-stay patients in the census sample. The admission sample also is less heavily weighted than the census sample by long-term residents; it is thus less conservative and more readily reflects changing characteristics of a nursing home population.
These particular time points were selected to provide the maximum span of time encompassing high-quality electronic medical data. In order to compare age groups and birth cohorts over time, we classified residents into six birth cohorts, each having an eight-year birth-date span (mirroring the eight-year difference between the comparison years), with the exception of the open-ended youngest and oldest groups. The oldest cohort was born before 1918; the remaining cohorts were born 1918–1925, 1926–1933, 1934–1941, 1942–1949, and after 1950.
We focused on broad categories of psychiatric disorders: dementia (Alzheimer's and other forms of dementia), depressive disorders (major depression and dysthymia), serious mental illness (schizophrenia, other psychoses, and bipolar and manic disorders), PTSD, alcohol use disorders (abuse, dependence, and alcohol-induced psychoses), and drug use disorders (abuse, dependence, and drug-induced psychoses, not including tobacco use disorder). We compared the prevalence of psychiatric disorders across age groups in both 1998 and 2006, in birth cohorts across the eight-year span, and in particular age groups across the two time points.
This repeated cross-sectional design cannot completely disentangle age, birth cohort, and period effects, but it can provide evidence consistent with one or more of these possible effects. For example, if age effects are present for dementia, we would expect increases in dementia prevalence with increasing age in cross-sectional comparisons (for example, higher dementia rates among persons aged 73 to 80 years than among those aged 65 to 72) and increases in dementia for birth cohorts that have aged in sequential comparisons (for example, higher dementia rates as the 65- to 72-year-old birth cohort ages eight years). If sequential birth cohort comparisons do not mirror cross-sectional age group comparisons, birth cohort or period effects are likely present. Period effects tend to affect all age groups and birth cohorts similarly, whereas birth cohort effects (or cohort and period effects in combination) selectively have an impact on some birth cohorts.
Results
Residents in the census samples
Table 1 summarizes characteristics of residents in the census samples; for comparison purposes, the table includes SVANH data ( 15 ). The VA nursing home census grew between 1990 and 1998 and declined thereafter to a level comparable to 1990. Although residents' average age has remained relatively stable, the proportions of younger (under age 65) and older (age 85 and older) residents declined from 1990 through 1998 and increased from 1998 through 2006. Most residents were men (96% to 97%); the proportion of married residents fluctuated between 35% and 41%.
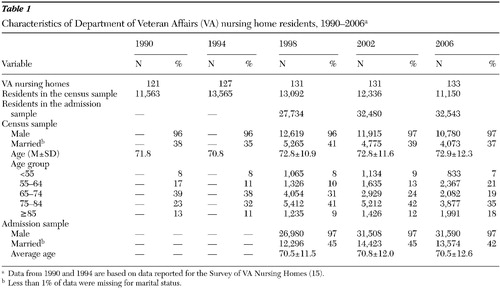 |
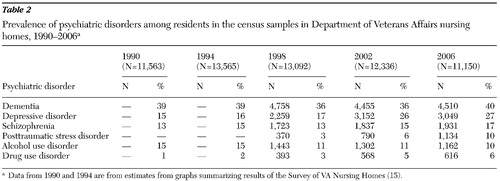
Table 2 presents prevalence data from the SVANH for 1990 and 1994 and for residents in the census samples in 1998, 2002, and 2006. Dementia and schizophrenia showed moderate variation in prevalence across the 16-year period. In contrast, the prevalence of depressive disorders was stable at about 16% from 1990 through 1998 and then jumped to 26% in 2002. Alcohol use disorder prevalence was lower in 1998 to 2006 than it was in the SVANH, but the percentage of residents with drug use disorders increased steadily over the 16-year period.
 |
Residents in the admission samples
In contrast with declining census numbers, the number of residents admitted to VA nursing homes increased from 1998 to 2006 ( Table 1 ). On average, admission residents were about two years younger than residents in the census samples and slightly more likely to be married. The proportions of men among census and admission residents were similar.
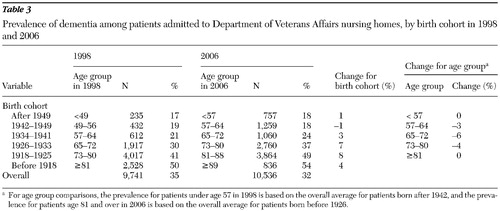
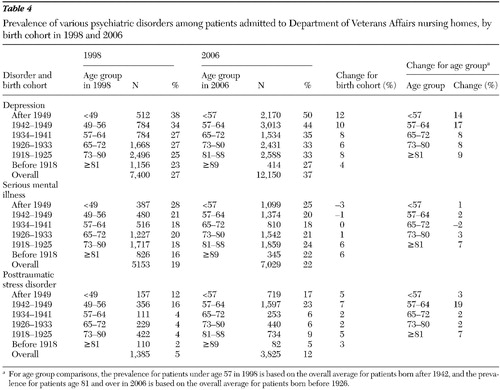
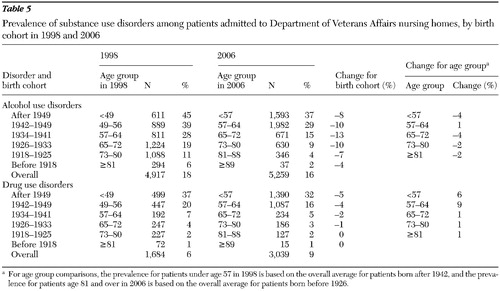
The prevalence of psychiatric disorders for residents in the admission sample in 1998 and 2006 are reported in Tables 3 , 4 , and 5 . These tables permit age-group comparisons within each of these years, as well as comparisons of equivalent age groups and the same birth cohorts across years.
 |
 |
 |
Consistent with expectations, the prevalence of dementia was higher among older residents in both 1998 and 2006, particularly after age 65 ( Table 3 ). Similarly, the prevalence of dementia increased in most birth cohorts from 1998 to 2006. In contrast, all but the youngest and oldest age groups saw slight declines in dementia prevalence between 1998 and 2006. For example, dementia prevalence for 65- to 72-year-olds declined from 30% to 24%.
The prevalence of depression declined with increasing age in both 1998 and 2006 ( Table 4 ). In contrast, the prevalence increased between 1998 and 2006 for each birth cohort and age group, especially for the 57- to 64-year-olds (increase from 27% to 44%).
In 1998 the prevalence of serious mental illness was highest among the youngest residents. Between 1998 and 2006 rates of serious mental illness declined slightly for younger birth cohorts but increased substantially for older birth cohorts. In comparisons of age groups at different points in time, the prevalence of serious mental illness has been relatively stable for younger residents but has increased for those over age 80.
In both 1998 and 2006, PTSD rates were highest for those born after 1941. The prevalence of PTSD was higher in 2006 than in 1998 for each birth cohort and age group, particularly for those born between 1918 and 1925 (mainly World War II veterans) and those born after 1941 (mainly Vietnam-era veterans).
The prevalence of alcohol use disorder was lower among older than among younger residents in both 1998 and 2006 ( Table 5 ). Similarly, prevalence declined for every birth cohort over time. The decline was particularly pronounced among those who were 57 to 64 years old in 1998. The prevalence of alcohol use disorder was lower in 2006 than in 1998 for all age groups except the 57- to 64-year-olds, resulting in a reduced level overall.
The prevalence of drug use disorder also declined with increased age in both years, and prevalence declined between 1998 and 2006 for all except the earliest birth cohorts, who had very low levels initially. Unlike the prevalence of alcohol use disorders, however, the prevalence of drug use disorders increased overall between 1998 and 2006 because of large prevalence increases among younger age groups.
Discussion
Results of the analyses presented here illustrate the complexity of changing patterns of psychiatric disorder prevalence in VA nursing homes. Multiple factors influence prevalence, including procedures for detecting and documenting mental health problems, the age distribution of VA patients, the varying natural history of different mental disorders, differential mortality and the availability of alternative treatment settings that may selectively remove some individuals from those seeking VA nursing home care, the balance of short versus long stays, and the effect of particular historical experiences. Some factors may offset each other, making it difficult to discern their effects. Nevertheless, the approach presented here, which examines prevalence among age groups and birth cohorts, may offer planners additional information on which to base projections of residents' future mental health needs.
Detection of psychiatric disorders
One problem in sorting out time-related trends in prevalence data is the changing definition and assessment of disorders across studies and over time. For example, estimates of depression prevalence in a sample of nursing home residents varied from 17.7% to 61.4%, depending on which database was used ( 10 ). Even when comparable measures are used, the issue of true difference versus measurement difference arises.
Our data suggest that increased awareness and improved screening may have influenced prevalence figures for several psychiatric disorders. Among VA primary care patients, depression diagnoses increased steadily after the 1998 initiative to improve psychiatric disorder screening ( 17 ). Consistent with this trend, residents in the census samples showed a jump in depression diagnoses between 1998 and 2002, and all age groups and birth cohorts showed increased depression prevalence between 1998 and 2006. A similar pattern of increased depression prevalence has been found for Medicare participants ( 20 ) and for newly admitted community nursing home residents ( 8 ), which may reflect overall improved awareness concerning depression in the older population.
Although comparable improvements in VA primary care screening for alcohol use disorders have been documented ( 18 ), our data do not show the same across-the-board increases in the prevalence of alcohol use disorders. Rather, over the eight-year period the prevalence of alcohol use disorders among residents in the census samples remained stable, and all birth cohorts and most age groups experienced declines in the prevalence of alcohol use disorders. It is possible that the effects of improved screening for alcohol use disorders were offset by a decline over time in the prevalence of alcohol use disorders.
We found increased PTSD prevalence among residents in the census samples and for all birth cohorts, particularly the Vietnam-era cohort. Heightened awareness of PTSD, reflected in discussion of PTSD in popular media and professional journals and the recommendation of universal screening for PTSD in VA primary care ( 19 ), may have resulted in increased numbers of veterans (especially Vietnam-era veterans) seeking and receiving delayed compensation for PTSD ( 21 ) and increased the likelihood of PTSD diagnosis among VA nursing home residents.
Age and cohort effects
Our findings point to age and cohort effects in the prevalence of psychiatric disorders among VA nursing home residents. Aging is accompanied by an increased risk of dementia ( 1 , 2 , 3 ), manifested here in higher rates of dementia for older than for younger admissions in 1998 and 2006 and in higher rates for most birth cohorts over time. In the general population, dementia prevalence is estimated to double for every four to six years of increased age ( 1 ). Among VA nursing home residents, at least a 16-year age difference was required for the prevalence rate to double (for example, for 57- to 64-year-olds versus 73- to 80-year-olds) in both years examined.
In VA nursing home admissions, dementia prevalence declined over time for most age groups, resulting in an overall decline from 35% to 32%. During this period, dementia prevalence increased from 36% to 40% among residents in the census samples, the total number of admissions increased from 27,734 to 32,543, and the total number of admissions with a dementia diagnosis also increased. Increased admissions in the absence of a census increase implies more short-term admissions, continuing a trend that saw a doubling in the percentage of short-term VA nursing home residents between 1995 and 2001 ( 16 ). These short-term admissions appear to have diluted the proportions of admissions with dementia. A similar decline in dementia prevalence has been found for first-time community nursing homes admissions between 1999 and 2005 ( 8 ).
Depression prevalence declined with increasing age at both points in time, consistent with patterns seen in cross-sectional community comparisons ( 22 ). This pattern may reflect a birth cohort effect as well as an age effect. It is consistent with previous findings that veterans born after about 1935 had three times the prevalence of major depression as those born before then ( 11 ). In the data presented here, birth cohorts born after 1941 had particularly large increases in depression prevalence from 1998 to 2006.
The role of nursing homes in the care of residents with serious mental illness appears relatively unchanged over time, except among the oldest residents, for whom the prevalence of serious mental illnesses increased substantially. These increases may reflect ongoing shifts in placement options for older veterans with serious mental illness, such as specialized care offered in VA psychogeriatric units and designated psychogeriatric nursing home beds ( 23 ), which have been increasingly emphasized.
The findings for PTSD confirm a strong association between Vietnam-era military service and PTSD shown by other researchers ( 11 , 12 ). As Vietnam-era veterans age, they carry elevated levels of PTSD into new age groups. In 2006 the cohort of World War II veterans also showed an elevated PTSD prevalence rate. In addition to better detection, the increased PTSD prevalence among the oldest nursing home residents may reflect the reawakening of PTSD symptoms as defenses are diminished by aging and illness ( 24 ).
Much like cross-sectional community samples ( 4 ), VA nursing home admissions showed reduced alcohol use disorder prevalence with increasing age in both 1998 and 2006. Furthermore, birth cohorts showed quite sizeable declines in the prevalence of alcohol use disorders between 1998 and 2006, particularly among the oldest residents (those born between 1926 and 1941). Over this period, all age groups except the 57- to 64-year olds experienced declines in the prevalence of alcohol use disorders, suggesting a downward trend over time in alcohol use problems, which is particularly striking in light of improved screening and diagnosis in VA primary care during this period.
As with the prevalence of alcohol use disorders, the prevalence of drug use disorders declined with increased age in both years and for birth cohorts over time. Thus, with aging, prevalence rates for substance use disorders appear to decline through such processes as premature mortality and remission. In contrast with the pattern for alcohol use disorders, however, overall prevalence of drug use disorders increased between 1998 and 2006. Younger age groups have experienced striking increases in the prevalence of drug use disorders that outweigh the age-related declines. These results are consistent with the literature showing higher drug use among the baby-boom generation ( 25 ). Because the prevalence increase is not present for all age groups, it appears unlikely to reflect improved screening alone. At ages 57 to 64 in 2006, the Vietnam-era veteran cohort had rates of drug use disorder nearly double that of the cohort of the interwar period and the Korean War at the same age in 1998. Thus we can predict a continuing increase in the prevalence of drug use disorders as cohorts with historically higher levels of drug use constitute more of the VA nursing home population. Prevalence may tend to stabilize or decline as Vietnam-era veterans dominate the VA nursing home population and experience declining drug use problems as they age.
Limitations
Although these interpretations of prevalence patterns reflect intuitive and parsimonious explanations of these data, there is no definitive way to disentangle age, birth cohort, and period effects. Furthermore, these comparisons are based on diagnoses recorded in administrative records and may not reflect true changes in disorder prevalence. The marked increase in depression prevalence between 1998 and 2006 is a clear example of the impact of changes in recognition of a disorder. Many residents with diagnosable depression were likely overlooked before the change in screening that began in 1998. Similarly, the comparisons we have made with results from the SVANH must be interpreted with caution, because diagnostic practices and the specific methods for determining prevalence differed somewhat between the SVANH and the analyses presented here. Although we have noted a number of ways in which our findings parallel results obtained for community nursing homes, wholesale generalization is unwarranted. VA nursing homes serve a limited segment of the population who use community nursing homes, and they function under different financial and policy constraints.
Conclusions
Our findings suggest that changes in the mental health needs of the VA nursing home population are a function of complex factors; they inject a note of caution into projections of future changes. Nevertheless, these findings may help planners anticipate residents' treatment needs and changes that may result from proposed policy decisions. For example, over the past decade, increasing proportions of the VA nursing home census population have had a dementia diagnosis, although increases in short-stay residents have diluted their proportions among nursing home admissions. Anticipated changes in the age distribution of the nursing home population will likely have an impact on dementia prevalence. As the World War II veteran cohort dies and the Vietnam-era cohort begins to dominate the VA nursing home population, nursing homes are likely to have fewer extremely old residents and more 65- to 74-year-olds, with a consequent decrease in dementia prevalence. As this birth cohort ages into their mid-70s around 2020, VA nursing homes will likely experience a significant increase in the demand for long-term care of dementia residents. Changes in factors such as the availability and financing of home-based care will also have an impact on these patterns. Shifts in the birth cohort profile of VA nursing home residents also are likely to result in increased prevalence of drug use disorders and PTSD, which will challenge staff in new ways.
In 2006, 67% of residents admitted to VA nursing homes had a psychiatric diagnosis, and 71% of residents in the census sample had at least one psychiatric diagnosis, consistent with overall rates of 71% and 75% in the 1990 and 1994 SVANH. These rates underline the continuing importance of training VA nursing home staff to work effectively with residents whose medical problems are accompanied by significant mental health needs.
Acknowledgments and disclosures
This research was supported in part by grant IIR 03-243 from the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development Health Services Research and Development Service (HSR&D). The findings and conclusions are those of the authors and do not necessarily represent those of the Department of Veterans Affairs or HSR&D. The authors thank Kathy Fung, M.S., and Kirsten Unger-Hu, M.S., for their valuable contributions to data management and analyses.
The authors report no competing interests.
1. Jorm AF, Jolley D: The incidence of dementia: a meta-analysis. Neurology 51:728–733, 1998Google Scholar
2. Martens PJ, Fransoo R, et al: Prevalence of mental illness and its impact on the use of home care and nursing homes: a population-based study of older adults in Manitoba. Canadian Journal of Psychiatry 52:581–590, 2007Google Scholar
3. Skoog I: Psychiatric epidemiology of old age: the H70 study—the NAPE Lecture 2003. Acta Psychiatrica Scandinavica 109:4–18, 2004Google Scholar
4. Karlamangla A, Zhou K, Reuben D, et al: Longitudinal trajectories of heavy drinking in adults in the United States of America. Addiction 101:91–99, 2005Google Scholar
5. Moore AA, Gould R, Reuben DB, et al: Longitudinal patterns and predictors of alcohol consumption in the United States. American Journal of Public Health 95:458–465, 2005Google Scholar
6. Rice JP, Neuman RJ, Saccone NL, et al: Age and birth cohort effects on rates of alcohol dependence. Alcoholism: Clinical and Experimental Research 27:93–99, 2003Google Scholar
7. Sherrell K, Anderson R, Buckwalter K: Invisible residents: the chronically mentally ill elderly in nursing homes. Archives of Psychiatric Nursing 12:131–139, 1998Google Scholar
8. Fullerton CA, McGuire TG, Feng Z, et al: Trends in mental health admissions to nursing homes, 1999–2005. Psychiatric Services 60:965–971, 2009Google Scholar
9. Mechanic D, Alpine DD: Use of nursing homes in the care of persons with severe mental illness: 1985 to 1995. Psychiatric Services 51:354–358, 2000Google Scholar
10. Bagchi AD, Verdier JM, Simon SE: How many nursing home residents live with a mental illness? Psychiatric Services 60:958–964, 2009Google Scholar
11. Frueh BC, Grubaugh AL, Acierno R, et al: Age differences in posttraumatic stress disorder, psychiatric disorders, and healthcare service use among veterans in Veterans Affairs primary care clinics. American Journal of Geriatric Psychiatry 15:660–672, 2007Google Scholar
12. Villa VM, Harada ND, Washington D, et al: Health and functioning among four war eras of US veterans: examining the impact of war cohort membership, socioeconomic status, mental health, and disease prevalence. Military Medicine 167:783–789, 2002Google Scholar
13. Hughes JS: Can the Veterans Affairs health care system continue to care for the poor and vulnerable? Journal of Ambulatory Care Management 26:344–348, 2003Google Scholar
14. Desai MM, Rosenheck, RA: Trends in discharge disposition, mortality, and service use among long-stay psychiatric residents in the 1990s. Psychiatric Services 54:542–548, 2003Google Scholar
15. Stockford D, Kelly J, Seitz K: Report on the 1990 and 1994 Surveys of VA NHs (SR-008-95-6). Washington, DC, Department of Veterans Affairs, National Center for Veteran Analysis and Statistics, 1995Google Scholar
16. Gardner J, Hendricks A: Forecasting Trends in VA Long-Term Care in the Absence of the Millennium Act Through Fiscal Year 2002. HCFE data brief no 2005-02. Boston, VA Boston Health Care System Research and Development, Health Care Financing and Economics, 2005Google Scholar
17. Kirchner JE, Curran GM, Aikens J: Detecting depression in VA primary care clinics. Psychiatric Services 55:350, 2004Google Scholar
18. Curran GM, Kirchner JE, Allee E, et al: Detection of substance use disorders in Veterans Affairs primary care clinics. Psychiatric Services 54:1326, 2003Google Scholar
19. Ouimette P, Wade M, Prins A, et al: Identifying PTSD in primary care: comparison of the Primary Care-PTSD screen (PC-PTSD) and the General Health Questionnaire-12 (GHQ). Journal of Anxiety Disorders 22:337–343, 2008Google Scholar
20. Crystal S, Sambamoorthi U, Walkup JT, et al: Diagnosis and treatment of depression in the elderly Medicare population: predictors, disparities, and trends. Journal of the American Geriatrics Society 51:1718–1728, 2003Google Scholar
21. Wilson JF: Posttraumatic stress disorder needs to be recognized in primary care. Annals of Internal Medicine 146:617–620, 2007Google Scholar
22. Gallo JJ, Lebowitz BD: The epidemiology of common late-life mental disorders in the community: themes for the new century. Psychiatric Services 50:1158–1166, 1999Google Scholar
23. Kim KY, Jones E, Goldstein MZ: Mental health services for older veterans in the VA system. Psychiatric Services 52:765–768, 2001Google Scholar
24. Buffum MD, Wolfe NS: Posttraumatic stress disorder and the World War II veteran. Geriatric Nursing 16:264–270, 1995Google Scholar
25. Colliver JD, Compton WM, Gfroerer JC, et al: Projecting drug use among aging baby boomers in 2020. Annals of Epidemiology 16:257–265, 2006Google Scholar



