Collaborative Care for Depressed Patients With Chronic Medical Conditions: A Randomized Trial in Puerto Rico
Major depression, one of the most common mental disorders worldwide, is associated with substantial disability, reduced quality of life, and increased mortality ( 1 , 2 ). Individuals living with depression often have comorbid general medical conditions ( 3 , 4 ). The World Health Organization (WHO) World Health Survey found that although the prevalence of depression among participants without chronic general medical conditions was 3.2%, the prevalence among those with such co-occurring conditions ranged from 9.3% for people with one condition to up to 23% for those with two or more chronic conditions ( 5 ). Furthermore, the worst health status was experienced by individuals with comorbid depression and chronic general medical conditions. These findings indicate that depression contributes to the burden of disease worldwide, and they highlight the importance of addressing depression as a public health priority ( 5 ).
Despite the major impact of depression, most of those in need of treatment do not receive care. Although depressed individuals tend to be high users of primary care services, few cases are recognized at this critical point of entry into the health system ( 6 ). Even among those who received a diagnosis, rates of adequate treatment are low ( 7 , 8 ). Improving the management of depression in primary care is fundamental to the WHO global policy for mental health ( 7 ). Recently, WHO issued a report calling for action to scale up the integration of mental health into primary care systems around the world. This population-based strategy is considered to be essential to reach the large number of depressed individuals who are managed solely in primary care.
Over the past decades, a variety of approaches to improve the recognition and management of depression in primary care have been implemented ( 9 ). Initial interventions focused on clinician educational strategies such as individual and group-based teaching, dissemination of guidelines, and use of local opinion leaders. A synthesis report that examined the effectiveness of these capacity-building strategies concluded that they were largely ineffective in improving patient recognition or outcomes when provided alone ( 10 ). In recent years, a substantial number of rigorous studies have focused on evaluating the impact of collaborative care interventions. Particular attention has been directed toward high-risk groups, such as patients with coexisting general medical illnesses ( 11 , 12 , 13 , 14 , 15 ).
Gilbody and colleagues ( 16 ) conducted a formal meta-analysis of studies that met the criteria for collaborative care. Collaborative care was defined as a comprehensive intervention in which at least two out of three types of professional (care manager, primary care physician, and mental health specialist) worked collaboratively in a primary care setting. Strategies common to most models included a redesign of the delivery of services to include screening, training, and routine follow-up of patients during and after treatment. The results of this review overwhelmingly supported the effectiveness of collaborative care models in improving patient adherence to treatment and clinical outcomes. The authors concluded that in the United States sufficient evidence had emerged by 2000 to demonstrate the effectiveness of collaborative care models. However, they noted that further research was needed to examine whether these findings could be replicated in health settings other than in the United States.
The past several years have shown an increased interest in improving collaboration between the mental health and general health care systems in Puerto Rico, for several reasons. Approximately 1.5 million residents, or 38% of Puerto Rico's population, are enrolled in public insurance programs where mental health services are provided by carve-out specialty groups ( 17 ). The Health Evaluation Commission, appointed in 2005 by the governor of Puerto Rico to assess the status of the health care system, noted that mental health care is fragmented and disjointed, lacking a comprehensive response to the nature and scope of existing mental health problems ( 18 ). The commission concluded that the existing model of health services delivery needed to be changed and called for integrated general medical and mental health programs focused on the delivery of services in a unified and holistic manner.
An important step in paving the way for the integration of services in Puerto Rico is to identify models for managing depression that contribute to improved treatment outcomes in the general health care system. The randomized controlled trial reported here was designed to examine whether a collaborative care model for depression would improve clinical and functional outcomes for depressed primary care patients with chronic medical conditions in Puerto Rico. We focused on patients with comorbid conditions because they have been shown to have increased use of health services ( 19 , 20 , 21 ) and worse depression treatment outcomes ( 22 ). We hypothesized that patients with comorbid conditions in the collaborative care model would have fewer depression symptoms and higher levels of functioning compared with patients in usual care.
Methods
Participants
Participants were recruited from a pool of patients who presented for general medical treatment at participating clinics. Patients were eligible if they were aged 18 or older, met criteria for major depression, were willing to provide informed consent, and had any of the following health conditions: diabetes, hypothyroidism, asthma, hypertension, chronic bronchitis, arthritis, heart disease, high cholesterol, or stroke. We did not include patients with serious suicidal risk or terminal illness or patients who had a history of bipolar or psychotic disorder or who were abusing drugs or alcohol. Patients had to be Spanish speaking and to have stated an intention to use the clinic as their main source of care in the next six-month period. Those receiving mental health treatment or applying for disability benefits were also excluded.
A nonconsecutive convenience sample of patients was drawn from 14 internal medicine or primary care clinics from four diverse health care organizations, including independent provider associations, health maintenance organizations, a regional health insurance plan, and academically affiliated practices. They were located in the greater metropolitan area of San Juan, Puerto Rico, and most served primarily low-income patients. Before study implementation a meeting was held with clinic personnel to discuss strategies to facilitate the integration of study procedures into the clinic workflow. Trained research assistants approached patients who were in clinic waiting rooms. Patients were approached on the basis of availability at the moment. Those who gave written informed consent were assessed for the presence and severity of major depression with the nine-item depression module of the Patient Health Questionnaire (PHQ-9) ( 23 , 24 , 25 ) and the depression scale of the Hopkins Symptom Checklist (HSCL-20) ( 26 ). Interviews were conducted in private offices to encourage participation and ensure confidentiality.
Out of 2,516 patients screened, 307 patients who met DSM-IV criteria for major depression based on their PHQ-9 score and who had a mean item score higher than 1.0 on the HSCL-20 were invited for baseline screening approximately one week after the initial screening interview. To determine whether patients were eligible for random assignment, we used a two-stage screening process that required them to maintain a mean item score higher than 1.0 on the HSCL-20 at the second interview. A total of 227 (74%) of the 307 patients who met initial eligibility criteria completed baseline screening, and among these 208 met criteria for random assignment to a study condition. Eighty-six percent of eligible patients (N=179) agreed to participate.
The 179 patients who met study criteria were assigned to either collaborative care (N=89) or usual care (N=90) according to a random number sequence developed with a computerized random number generator. Sequences were set up in blocks of 20, printed on cards, and placed in consecutively numbered opaque envelopes by data analysts assisting with the study. To obtain random assignment information for each patient, research assistants contacted a data analyst at the central office. The analyst selected the next sealed envelope corresponding to the assigned treatment condition and notified the research assistant. Study participants were enrolled between March 2005 and October 2007. Of the 179 patients enrolled, the following number of patients completed eight-, 16-, and 24-week assessments: week 8 assessment, 85 (96%) collaborative care patients and 78 (87%) usual care patients; week 16 assessment, 83 (93%) collaborative care patients and 80 (89%) usual care patients; and week 24 assessment, 83 (93%) collaborative care patients and 84 (93%) usual care patients. A total of 81 collaborative care patients (91%) and 74 usual care patients (82%) completed all three assessments. No significant differences were found between participants with complete data and those with only one or two assessments. Written informed consent was obtained after we completely described the study to participants. The study protocol was approved by the institutional review board at the Medical Sciences Campus of the University of Puerto Rico.
Treatment conditions
Collaborative care. Collaborative care involved a multicomponent intervention, including program oversight and teamwork among physicians, mental health specialists, and care managers. Patients assigned to this group were provided education about depression and two evidence-based options that they could choose as an initial treatment—antidepressant medication or cognitive-behavioral therapy (CBT). Costs for both treatments were covered by the study. The care manager participated in the coordination of treatment initiation, as well as monitoring treatment adherence, side effects, and clinical response. Care managers contacted patients in person or by phone at least every two weeks initially and then monthly, for up to six months. Additional contacts could be scheduled as needed to help patients overcome barriers and provide treatment adherence support.
Care managers were master's-level counselors or psychologists. They received 12 hours of training and weekly supervision. They held a main role in facilitating communication between the patient, general medical clinician, and mental health specialist. In the medication treatment option, weekly sessions were scheduled with the consulting psychiatrist. The care manager presented new patients and provided follow-up for ongoing cases based on the depression severity tracking conducted during patient encounters. The psychiatrist recommended initial medication and dosage, as well as changes in medication or combined medication treatment if a patient showed limited response. The care manager forwarded the psychiatrist's recommendations for consideration by the patient's physician. Before study implementation, physicians were provided a one-hour training session on the recognition and treatment of major depression. Patients were prescribed selective serotonin reuptake inhibitors, and most received sertraline. The average dosage of sertraline in this study was 50 mg per day. In psychotherapy treatment, patients were provided 13 CBT sessions delivered in the primary care setting. CBT was provided by psychologists with master's or doctoral degrees. They received 24 hours of CBT training and weekly clinical supervision. Medication was considered for patients whose symptoms did not improve after eight weeks of CBT. The care manager provided mental health specialists a progress report for each CBT patient.
Usual care. Patients randomly assigned to receive usual care were informed of their diagnosis of depression and the mental health resources available with their insurance. The care manager encouraged patients to discuss depression treatment options with their provider. A note was placed in the patient's medical record to notify providers. Usual care practices across sites were highly uniform because most patients had health care plans that carve out behavioral health. Routine physician practice was to refer patients to mental health specialists when needed. Usual care patients could also self-refer to mental health specialists. Treatment provided in the specialized sector usually involved prescription of antidepressants or psychotherapy.
Study measures
Assessments were administered at baseline and eight, 16, and 24 weeks after randomization by interviewers blind to intervention status. Because a high proportion of patients had not completed high school and could have had difficulty reading, assessments were administered orally in a computer-assisted personal interview. Our primary outcome was change in depression symptoms as assessed by the 20-item depression scale of the HSCL-20. The Spanish-translated HSCL-20 measures a concept of depression that is statistically similar to that in the English version and can be used comparably to detect and measure severity of depression in primary care ( 27 , 28 ). Possible scores range from 0 to 4, with higher scores indicating more severe depression. Response to treatment at six months was defined as 50% or greater reduction in the HSCL-20 depression score. Our secondary outcome, health-related social functioning status, was assessed with the social functioning (SF) subscale of the 36-item Short-Form Health Survey ( 29 ). The Spanish version of this measure is valid and reliable and has adequate sensitivity to detect differences in patients' functional status ( 30 ). Possible scores range from 0 to 100, with higher scores indicating better functioning. Data on demographic characteristics, health services utilization, and behavioral factors also were collected.
Analyses
We examined whether demographic and clinical characteristics of patients in collaborative care and usual care were equivalent at baseline by using t tests for continuous data and chi square analyses for categorical data. To evaluate the effect of the collaborative care intervention on changes in clinical and functional longitudinal outcomes relative to usual care, we used mixed-effects regression analysis. This method is consistent with intent-to-treat principles because data from all randomly assigned participants are included in the analyses, whether their data are complete or not. In these analyses we specified an unstructured covariance matrix to account for the within-patient correlation among repeated assessments. We first evaluated a model specifying only a random intercept for the error term and then a model specifying both a random intercept and a random time (weeks) variable. For all analyses the model using both a random intercept and a random time effect provided a better fit to the data, so we used the random intercept and time to estimate our error term. Treatment effects were tested primarily through the group-by-time interactions. We used a p value of <.05 to detect statistically significant differences. All analyses were conducted with SAS software, version 9.1.
Results
Baseline patient characteristics
Demographic and clinical baseline characteristics of the sample are shown in Table 1 . There were no significant differences between patients randomly assigned to the intervention or usual care group. The mean age of participants was 55 (range 21–87 years), 76% were women, and 44% were married or cohabiting. Twenty-three percent of the patients were employed, and half had not completed high school. Participants reported that they were experiencing on average 2.54 of the seven comorbid chronic health conditions assessed. The mean±SD HSCL-20 depression score was 2.28±.56, indicating severe depression. Social functioning was moderately impaired, as illustrated by a mean score of 34.43±24.81 on the SF scale.
 |
Treatment received
Collaborative care patients had an average1.4(range 0–6) in-person contacts with the care manager and 8.2(range 0–23) telephone contacts with the care manager. The average length of contacts from the care manager was 11.7 minutes (range 4.3–34.5 minutes). At six months, 97% (N=86) of the patients in collaborative care had received depression treatment. Approximately half (N=47) received CBT, 40% (N=36) took antidepressant medications, 3% (N=3) received medication and CBT, and 3% (N=3) did not receive treatment. Of the patients who received antidepressants, 69% (N=27) completed treatment through month 6. Of the 47 patients who received CBT, one-third (N=16) completed all 13 treatment sessions, 79% (N=37) completed eight sessions, and 91% (N=43) completed six. The average number of CBT sessions was 10.1. Of 90 patients assigned to usual care, at six months 57% (N=51) reported that they had received depression treatment. Approximately half (N=25) took antidepressants, 37% (N=19) received psychotherapy, and 14% (N=7) received both medication and psychotherapy. Over 40% (N=39) of usual care patients indicated that they did not receive depression treatment.
Clinical outcomes
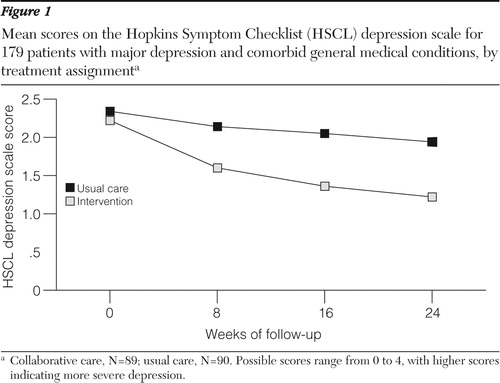
The collaborative care intervention significantly reduced depression symptoms in comparison to usual care. As Figure 1 shows, the two treatment groups had similar baseline mean±SE HSCL-20 scores (collaborative care, 2.22±.06; usual care, 2.34±.06). At six months, depression symptoms decreased for both groups of patients. However, the decrease was greater for patients in collaborative care. Mean scores on the HSCL-20 depression scale in the collaborative care group improved from the severe-to-moderate range at baseline to the mild range at six-month follow-up, whereas mean scores for usual care patients remained at the same level. We ran mixed-effects regression models using HSCL-20 data from baseline and eight-, 16-, and 24-week follow-ups. Table 2 shows statistically significant main effects for assessment time and treatment group, as well as for the interaction between time and treatment.
 |
Next, we compared the proportion of patients showing clinical recovery or improvement, predefined as at least a 50% decrease in the HSCL-20 score at the six-month follow-up. Statistically significant differences were found for both groups ( χ2 =17.11, df =1, p<.001). Almost 50% (N=41) of the collaborative care group showed an improvement at six months, compared with 19% (N=16) for the usual care group. Patients in collaborative care were 4.04 times as likely as those in usual care to show a response to treatment at six months (95% confidence interval=2.01–8.31).
The collaborative care intervention was also more effective than usual care in improving social functioning. Mixed-effects regression estimates for the SF scale yielded a significant result for the time-by-group interaction (F=10.33, p<.001) ( Table 2 ). No significant main effects were observed by assessment period and treatment group. As shown in Figure 2 , patients who received collaborative care had higher mean scores at follow-up, showing a steady increase in social functioning over time, whereas no significant difference in social functioning was observed for patients in usual care. Social functioning was better for patients in collaborative care than for patients in usual care at all follow-up time points (p<.05 at week 8, p<.01 at week 16, and p<.001 at week 24).

Discussion
Our findings support the usefulness of the collaborative care model for the treatment of depression in primary care. We found that depressed patients with chronic general medical illnesses reported a significant reduction in depression symptoms and improved functioning when offered evidence-based antidepressant treatment or CBT within a collaborative care model that included case management, patient and provider education, and psychiatric consultation. These results were achieved even though the interaction of depression and comorbid chronic medical conditions is associated with poor treatment outcomes ( 22 ). Furthermore, our data show that when depressed patients with chronic health conditions were given the opportunity to receive treatment for depression in primary health settings their use of depression care significantly increased.
To our knowledge, this randomized controlled trial is the first in Puerto Rico to test the effects of a collaborative care intervention for primary care patients with major depression. Our study took the prior research on collaborative care a step further by examining this model in a different health care system and patient population. Our results suggest that collaborative care can contribute to overcoming access barriers to mental health services and improve clinical and functioning outcomes of depressed patients with chronic general medical conditions in primary care practices in Puerto Rico. These findings are consistent with a large body of evidence showing that collaborative care practices improve the management of depression in primary care practices in the United States ( 15 , 16 , 31 , 32 , 33 , 34 , 35 , 36 ). Our findings are particularly important because they provide evidence for the benefits of collaborative care for depressed Latino patients in primary care practices in Puerto Rico, a group for which there is very limited mental health services research.
Several limitations should be noted in interpreting these results. First, recruiters of patients in primary care reception rooms did not systematically select patients for screening; this may subject the data to some selection bias. Second, several components of the intervention, including care manager, specialized mental health professionals, and antidepressant medication, were provided by the research project. Third, the data presented here were collected mainly from clinics providing care to socioeconomically disadvantaged patients, and the success of the intervention may or may not be supported with patients from other socioeconomic groups. Overall, these limitations may reduce the generalizability of the findings. They also suggest future directions for further study. Important aspects to address in future research are the organizational and financial factors relevant for the successful implementation of this model in primary care practices in Puerto Rico. In addition, future investigations should analyze the sustainability and cost-effectiveness of this approach over time. Although further study is needed to confirm and expand our findings, the emerging data from this study underscore the potential benefit of the collaborative care model for the management of depression within primary health practices in Puerto Rico.
Conclusions
Collaborative care significantly improved clinical symptoms and functional status of depressed patients with coexisting chronic medical conditions receiving treatment in primary care practices in Puerto Rico. These findings highlight the promise of the collaborative care model for strengthening the relationship between mental health and primary care services in Puerto Rico, a goal consistent with the WHO global policy for mental health.
Acknowledgments and disclosures
This project was supported by grant S06-GM-008224 from the National Institute of General Medical Sciences, grant WS297211 from Pfizer, Inc., and grant P20-RR11126 from the National Center for Research Resources.
The authors report no competing interests.
1. Mathers CD, Loncar D: Projections of global mortality and burden of disease from 2002 to 2030. PLoS Medicine 3:e442, 2006Google Scholar
2. Murray CJL, Lopez AD (eds): Global Burden of Disease: A Comprehensive Assessment of Mortality and Disability From Diseases, Injuries, and Risk Factors in 1990 and Projected to 2020. Cambridge, Mass, Harvard University Press, 1996Google Scholar
3. Anderson RJ, Freedland KE, Clouse RE, et al: The prevalence of comorbid depression in adults with diabetes: a meta-analysis. Diabetes Care 24:1069–1078, 2001Google Scholar
4. Jonas BS, Mussolino ME: Symptoms of depression as a prospective risk factor for stroke. Psychosomatic Medicine 62:463–471, 2000Google Scholar
5. Moussavi S, Chatterji S, Verdes E, et al: Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet 370:851–858, 2007Google Scholar
6. Wang PS, Aguilar-Gaxiola S, Alonso J, et al: Use of mental health services for anxiety, mood, and substance disorders in 17 countries in the WHO World Mental Health Surveys. Lancet 370:841–850, 2007Google Scholar
7. Mental Health: New Understanding, New Hope. World Health Report. Geneva, World Health Organization, 2001Google Scholar
8. Von Korff M, Goldberg D: Improving outcomes in depression: the whole process of care needs to be enhanced. British Medical Journal 323:948–949, 2001Google Scholar
9. Kates N, Mach M: Chronic disease management for depression in primary care: a summary of the current literature and implications for practice. Canadian Journal of Psychiatry 52:77–85, 2007Google Scholar
10. Gilbody S: What Is the Evidence on Effectiveness of Capacity Building of Primary Health Care Professionals in the Detection, Management and Outcome of Depression? Geneva, World Health Organization Regional Office for Europe, 2004. Available at www.euro.who.int?Document/E85243.pdf Google Scholar
11. Bogner HR, de Vries HF: Integration of depression and hypertension treatment: a pilot randomized controlled trial. Annals of Family Medicine 6:295–301, 2008Google Scholar
12. Ell K, Xie B, Quon B, et al: Randomized controlled trial of collaborative care management of depression among low-income patients with cancer. Journal of Clinical Oncology 26:4488–4496, 2008Google Scholar
13. Gilmer TP, Walker C, Johnson ED, et al: Improving treatment of depression among Latinos with diabetes using project Dulce and IMPACT. Diabetes Care 31:1324–1326, 2008Google Scholar
14. Katon WJ, Von Korff M, Lin EH, et al: The Pathways Study: a randomized trial of collaborative care in patients with diabetes and depression. Archives of General Psychiatry 61:1042–1049, 2004Google Scholar
15. Unützer J, Katon W, Callahan CM, et al: Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. JAMA 288:2836–2845, 2002Google Scholar
16. Gilbody S, Bower P, Fletcher J, et al: Collaborative care for depression: a cumulative meta-analysis and review of longer-term outcomes. Archives of Internal Medicine 166:2314–2321, 2006Google Scholar
17. Puerto Rico Health Insurance Administration: Data and Statistics of Puerto Rico Municipalities, 2005 [in Spanish]. Available at www.tendenciaspr.com/salud/planes_medicos_reforma_salud.htm Google Scholar
18. Health Systems Profile of Puerto Rico: Monitoring and Analysis of Health Systems Change/Reform. Washington, DC, Pan American Health Organization, 2007Google Scholar
19. Egede LE, Zheng D, Simpson K: Comorbid depression is associated with increased health care use and expenditures in individuals with diabetes. Diabetes Care 25:464–470, 2002Google Scholar
20. Simon GE, Von Korff M, Barlow W: Health care costs of primary care patients with recognized depression. Archives of General Psychiatry 52:850–856, 1995Google Scholar
21. Unützer J, Patrick DL, Simon G, et al: Depressive symptoms and the cost of health services in HMO patients aged 65 years and older: a 4-year prospective study. JAMA 277:1618–1623, 1997Google Scholar
22. Ford DE: Optimizing outcomes for patients with depression and chronic medical illnesses. American Journal of Medicine 121:S38–S44, 2008Google Scholar
23. Kroenke K, Spitzer RL, Williams JB: The PHQ-9: validity of a brief depression severity measure. Journal of General Internal Medicine 16:606–613, 2001Google Scholar
24. Spitzer RL, Kroenke K, Williams JB: Validation and utility of a self-report version of PRIME-MD: the PHQ Primary Care Study: Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA 282:1737–1744, 1999Google Scholar
25. Wulsin L, Somoza E, Heck J: The Feasibility of Using the Spanish PHQ-9 to Screen for Depression in Primary Care in Honduras. Primary Care Companion Journal of Clinical Psychiatry 4:191–195, 2002Google Scholar
26. Derogatis LR, Lipman RS, Rickels K, et al: The Hopkins Symptom Checklist (HSCL): a self-report symptom inventory. Behavioral Science 19:1–15, 1974Google Scholar
27. Bernal Cercos A, Fuest Vallverdu R, Urbieta Solana R, et al: Relaxation therapy in patients with anxiety and somatoform disorders in primary care [in Spanish]. Atencion Primaria 15:499–504, 1995Google Scholar
28. Bonicatto S, Dew MA, Soria JJ, et al: Validity and reliability of Symptom Checklist 90 (SCL90) in an Argentine population sample. Social Psychiatry and Psychiatric Epidemiology 32:332–338, 1997Google Scholar
29. Ware JE, Sherbourne CD: The MOS 36-item Short-Form Health Survey (SF-36): I. conceptual framework and item selection. Medical Care 30:473–483, 1992Google Scholar
30. Arocho R, McMillan CA, Sutton-Wallace P: Construct validation of the USA-Spanish version of the SF-36 health survey in a Cuban-American population with benign prostatic hyperplasia. Quality of Life Research 7:121–126, 1998Google Scholar
31. Hunkeler EM, Katon W, Tang L, et al: Long term outcomes from the IMPACT randomised trial for depressed elderly patients in primary care. British Medical Journal 332:259–263, 2006Google Scholar
32. Katon W, Robinson P, Von Korff M, et al: A multifaceted intervention to improve treatment of depression in primary care. Archives of General Psychiatry 53:924–932, 1996Google Scholar
33. Miranda J, Green BL, Krupnick JL, et al: One-year outcomes of a randomized clinical trial treating depression in low-income minority women. Journal of Consulting and Clinical Psychology 74:99–111, 2006Google Scholar
34. Miranda J, Schoenbaum M, Sherbourne C, et al: Effects of primary care depression treatment on minority patients' clinical status and employment. Archives of General Psychiatry 61:827–834, 2004Google Scholar
35. Rost K, Nutting P, Smith JL, et al: Managing depression as a chronic disease: a randomized trial of ongoing treatment in primary care. British Medical Journal 325:934, 2002Google Scholar
36. Wells KB, Stewart A, Hays RD, et al: The functioning and well-being of depressed patients: results from the Medical Outcomes Study. JAMA 262:914–919, 1989Google Scholar



