A Literature Review of Studies of Depression and Treatment Outcomes Among U.S. College Students Since 1990
According to the fall 2007 American College Health Association-National College Health Assessment ( 1 ), a national survey of approximately 20,500 college students on 39 campuses, 43.2% of the students reported "feeling so depressed it was difficult to function" at least once in the past 12 months. More than 3,200 university students reported being diagnosed as having depression, with 39.2% of those students diagnosed in the past 12 months, 24.2% currently in therapy for depression, and 35.8% taking antidepressant medication. Among the students surveyed, 10.3% admitted "seriously considering attempting suicide" within the past 12 months and 1.9% actually attempted suicide during that period.
Although the above data may seem surprising to some, it is not to most mental health clinicians and administrators at U.S. colleges. According to the 2008 National Survey of Counseling Center Directors, 95% of respondents believe that there has been a trend in recent years of an increase in the number of students with serious psychological problems. In 2008 an estimated 26% of counseling center clients were taking psychiatric medication, up from 20% in 2003, 17% in 2000, and 9% in 1994 ( 2 ). And although the rate of suicide among college students may have decreased in recent decades ( 3 ), suicide remains the third leading cause of death among adolescents and young adults ( 4 ).
Many college administrators have begun to appreciate the effect that a student's depression can have on overall functioning in the college community. Depression has been linked to academic difficulties as well as interpersonal problems at school, with more severe depression correlated with higher levels of impairment ( 5 ). The treatment of depression among college students has been associated with a protective effect on these students' grade point averages ( 6 ). In an effort to diagnose and treat early and effectively, and thus decrease the excess morbidity and risk of suicide associated with depression, some U.S. colleges have even begun to screen students for depression in the primary care setting ( 7 ).
There are unique challenges of providing treatment to college students. These challenges include significant academic pressure in semester-based cycles, extensive semester breaks that result in discontinuities of care, and heavy reliance on community supports that can be inconsistent. Given the prevalence and impact of depression on college campuses and the varying services offered by university mental health centers throughout the United States, there is a significant need to evaluate successful models of treatment and their related outcomes.
Methods
The databases PsycINFO, MEDLINE, and CINAHL were searched for studies related to depression among U.S. college students and treatment outcome by using the following terms: "depression," "college or university or graduate or junior college or community college students," "colleges," "community colleges," "treatment and prevention," "empirical study," and "peer reviewed journal." Initially, no limitation was placed on years included in the search. Eighteen relevant publications were read and analyzed closely for method and content, with particular focus on location and inclusion criteria of study participants. Studies were eliminated if participants were students at colleges outside of the United States, if the studies did not have specific depression criteria for inclusion, or if the students included were at risk of depression but did not meet criteria for having depression. Nine remaining articles were reviewed further, and it was decided that the five studies published before 1990 had decreased relevance and would be excluded from this review in light of the growing availability of selective serotonin reuptake inhibitor medications since 1990, which substantially changed the treatment of depression among college students. In addition, the demographic characteristics of U.S. college students may have changed since the early 1990s, with many college counseling center directors noting a trend in recent years of an increase in students with serious psychological problems ( 2 ). Only four articles ( 8 , 9 , 10 , 11 ) remained for this review of depression and treatment outcomes of U.S. college students.
Results
Table 1 summarizes the four studies on depression and treatment outcomes that were reviewed in this study.
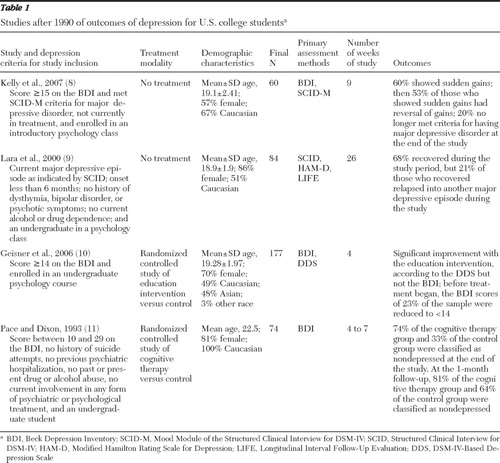 |
In 2007 Kelly and colleagues ( 8 ) conducted a nonexperimental study that recruited from introductory psychology classes university students with depression who were not currently in treatment, offering both financial compensation and class credit for research involvement. Sixty college students (66% Caucasian, 57% female) with major depression were followed for nine weeks without any treatment to assess for sudden gains (that is, precipitous improvements in depressive symptomatology), remission of depressive symptoms, and reversal of improvements. The authors found that 60% of the college students with major depression experienced sudden gains over the nine weeks of not receiving treatment. However, before the end of the nine-week observation period, more than half of these sudden gains reversed. At the end of the period of not receiving treatment, depression was in remission for 20% of the students. The authors concluded that sudden gains may be part of the natural course of depression for some college students, irrespective of treatment, and that self-evaluation processes may play an important role in recovery.
In 2000 Lara and colleagues ( 9 ) conducted a nonexperimental study in which undergraduate students taking psychology classes who had a recent-onset major depressive episode were paid or received course credit for their research participation. Eighty-four students (51% Caucasian, 86% female) were followed for 26 weeks to assess whether various psychosocial factors predicted the short-term course of major depression. The authors found that within the 26-week period of no treatment, 68% of the college students who were initially depressed recovered. Among those who recovered, 21% relapsed by the end of the 26-week period into another major depressive episode. Lara and colleagues concluded that college students with depression may sometimes spontaneously recover and relapse and that harsh discipline in childhood was significantly associated with higher mean levels of depression at follow-up and relapse but not with recovery.
In 2006 Geisner and colleagues ( 10 ) conducted a four-week randomized controlled trial of depression treatment and recruited undergraduates with depression who were enrolled in psychology courses to participate for course credit. The study enrolled 177 students with depression (49% Caucasian and 48% Asian, 70% female) who were randomly assigned either to an intervention group that received personalized mailed feedback or to a control group. The authors found that depressive symptoms improved for both the intervention and control groups, but in the intervention condition there was a significantly greater improvement of depressive symptoms, as measured by the DSM-IV-Based Depression Scale. There was no significant difference between the intervention and control groups on symptoms measured by the Beck Depression Inventory (BDI). Geisner and colleagues concluded that an intervention using personalized mailed feedback may be useful for reducing depressive symptoms among college students.
In 1993 Pace and Dixon ( 11 ) conducted a four- to seven-week randomized controlled trial to assess the treatment effectiveness of individual cognitive therapy for college students with depressive symptoms. Participating undergraduate students earned course credit for their research involvement. Seventy-four students (100% Caucasian, 81% female) who met strict criteria for study inclusion were randomly assigned to either a group that received individual cognitive therapy or a control condition where participants did not receive treatment and were put on a waiting list for cognitive therapy. Pace and Dixon found that 74% of participants in the cognitive therapy group (versus 33% in control group) were classified as nondepressed with BDI scores of less than 10 after four to seven weeks of treatment. At the one-month follow-up, 81% of participants in the cognitive therapy group (versus 64% of control group) were classified as nondepressed. Outcomes at both time points were statistically significant in favor of cognitive therapy. The authors concluded that brief individual cognitive therapy may effectively reduce mild to moderate depressive symptoms as well as depressive self-schemata among college students.
Discussion
The current body of literature on depression and treatment outcomes among U.S. college students is sparse, and for the four studies we found, varying inclusion and exclusion criteria, assessment methods, and lengths of treatment make the interpretation of results difficult. Whereas Kelly and colleagues ( 8 ) and Lara and colleagues ( 9 ) used the Structured Clinical Interview for DSM-IV to diagnose participants with major depressive disorder, Geisner and colleagues ( 10 ) and Pace and Dixon ( 11 ) used self-report scales to measure depressive symptoms for study inclusion and Pace and Dixon excluded students with severe levels of depressive symptoms. All four studies recruited students who were not seeking treatment and who were offered course credit for participating, a reward that might have influenced the degree of improvement in outcomes. There was no consistent standard used across studies to define a student with depression, even when using the same assessment tool. In terms of length of treatment, only two of the four reviewed studies followed students for more than nine weeks. The length of time over which students are assessed is especially critical for the college population, where time is defined by a semester calendar, moods are often influenced by exam schedules, and treatments are adjusted to accommodate upcoming vacations ( 12 ). Today's college mental health services tend to employ short-term models of care (eight to 16 sessions), with referral to outside clinicians if longer-term treatment is necessary ( 13 ). Given these dynamics, future research in college mental health will need to establish quality standards for ongoing monitoring and follow-up of students' treatment outcomes.
Unfortunately, the results from these four studies may not be fully applicable to college students today or in the future, particularly in light of the changing demographic characteristics of those attending universities as well as the rapidly evolving role of pharmacology in the treatment of depression. Only two of the four studies reviewed offered any active treatment for depression, and none of the studies included any form of pharmacological treatment. Consistent with current medical literature and best practices, many treatment-seeking college students diagnosed as having depression currently receive psychotherapy and psychopharmacological treatment ( 1 ). Because major depression can be a chronic recurring condition, future research needs to evaluate the effectiveness of the various treatment modalities used to treat college students with depression. This is particularly important in light of the recent addition of a black-box warning for the use of antidepressant medications among young adults aged 18 to 24 years, which recommends the close monitoring of patients taking antidepressant medication for clinical worsening, suicidality, or unusual changes in behavior.
Conclusions
In light of the high prevalence of depression among college students today and the risks and sequelae this illness poses if not diagnosed and treated early and effectively, it is imperative that research funding be increased for both naturalistic and intervention studies of depression and treatment outcomes in the college health setting. First, research documenting depression and treatment outcomes in this cohort should be identified in order to evaluate the adequacy of current care. Second, research should be directed to assessing specific short-term or semester-based interventions for students with depression. Models that explore the effectiveness of integration with primary care, care management, medication, and short-term psychotherapy are all important targets for future study. By conducting such research, effective treatment models and benchmarks of treatment outcome in the college population can be developed and integrated into college mental health practice.
Acknowledgments and disclosures
The authors thank Michael Klein, Ph.D., for his assistance in the development of this brief report.
Dr. Chung has served on advisory boards for Takeda Pharmaceuticals and Lundbeck Pharmaceuticals and has served as a speaker for Pfizer and Jazz Pharmaceuticals. Dr. Miller reports no competing interests.
1. American College Health Association-National College Health Assessment: Reference Group Report, Fall 2007. Baltimore, American College Health Association, 2008. Available at www.acha-ncha.org/reports_ACHA-NCHAoriginal.html Google Scholar
2. Gallagher R: National Survey of Counseling Center Directors, Alexandria, Va, International Association of Counseling Services, 2008. Available at www.iacsinc.org Google Scholar
3. Schwartz A: Four eras of study of college student suicide in the United States: 1920–2004. Journal of American College Health 54:353–366, 2006Google Scholar
4. National Center for Injury Prevention and Control: Web-based Injury Statistics Query and Reporting System (WISQARS). Atlanta, Ga, Centers for Disease Control and Prevention, 2005. Available at www.cdc.gov/injury/wisqars/index.html Google Scholar
5. Heiligenstein E, Guenther G, Hsu K, et al: Depression and academic impairment in college students. Journal of American College Health 45:59–64, 1996Google Scholar
6. Hysenbegasi A, Hass S, Rowland C: The impact of depression on the academic productivity of university students. Journal of Mental Health Policy and Economics 8:145–151, 2005Google Scholar
7. Chung H, Klein M: Improving identification and treatment of depression in college health. Student Health Spectrum, June 2007, pp 13–19Google Scholar
8. Kelly M, Roberts J, Bottonari K: Non-treatment related sudden gains in depression: the role of self-evaluation. Behaviour Research and Therapy 45:737–747, 2007Google Scholar
9. Lara ME, Klein DN, Kasch KL: Psychosocial predictors of the short-term course and outcome of major depression: a longitudinal study of a nonclinical sample with recent-onset episodes. Journal of Abnormal Psychology 109:644–650, 2000Google Scholar
10. Geisner I, Neighbors C, Larimer M: A randomized clinical trial of a brief, mailed intervention for symptoms of depression. Journal of Consulting and Clinical Psychology 74:393–399, 2006Google Scholar
11. Pace T, Dixon D: Changes in depressive self-schemata and depressive symptoms following cognitive therapy. Journal of Counseling Psychology 40:288–294, 1993Google Scholar
12. Lee C: Evidenced-based treatment of depression in the college population. Journal of College Student Psychotherapy 20:23–31, 2005Google Scholar
13. Stone G, McMichael J: Thinking about mental health policy in university and college counseling centers. Journal of College Student Psychotherapy 10:3–28, 1996Google Scholar



