Four-Year Follow-Up of Long-Stay Patients Settled in the Community After Closure of Italy's Psychiatric Hospitals
This study provides an account of the final phase of the long process of closing Italy's psychiatric hospitals that began in 1978 ( 1 , 2 ). By 1998 the hospitals housed only patients who were particularly difficult to resettle for social and psychological reasons and whose discharge was considered impossible by hospital staff. In addition, these patients had become accustomed to long-term residence in a hospital. Thus definitive closure of hospitals and discharge of remaining patients into community-based facilities providing various degrees of care and supervision, as specifically required by Italian law in 1996, was full of uncertainty and opposed by many of the hospitals' residential staff as well as by many psychiatrists. The principal criticism was that the stress and trauma resulting from "uprooting" patients who had become adapted to institutional life would increase morbidity and mortality.
This lack of consensus is considered one of the main difficulties in the deinstitutionalization process ( 3 ). Moreover, in countries that implement a large-scale reduction in the number of psychiatric hospital beds rather than a definitive closure of hospitals, discharge of all patients is simply an option ( 4 ) and thus some patients remain hospitalized ( 5 ). Mainstream opinion suggests that even if the general psychological condition of long-stay hospital patients who are transferred to community-based facilities does not worsen, any improvement is related only to satisfaction with the place of residence, quality of life, and social functioning ( 6 , 7 , 8 ).
The purpose of this study was to contribute to the knowledge base related to reduction—and even elimination—of large institutions and similar settings for housing the most difficult-to-treat patients, and in some cases the longest-staying patients, with severe mental illness.
Methods
Design
The longitudinal study focused on the final patients discharged from the psychiatric hospitals of Collegno and Grugliasco, which are situated near Turin, Italy. Because the hospitals were in the process of closing and no new admissions were permitted, it was impossible to select patients remaining in the hospitals as a control group. For this reason, the study analyzed the condition of a single group as it evolved over time.
Unlike other studies on community placement of long-stay patients ( 6 , 9 ), this study had a methodological design that comprised no fewer than seven assessments over a four-year period. These periodic assessments enabled evaluation of overall trends in the resettling process—that is, it was not a single snapshot of the condition of patients at a specific time after discharge. Data were collected by the medical team, which included some of the authors, that oversaw the transition process in the Turin area, chiefly by setting goals and monitoring patients' clinical and functional outcomes ( 10 ).
Some of the tools currently in use to assess clinical and functional conditions of patients with mental disorders have been found to be difficult to use with long-stay psychiatric patients ( 11 ). Evaluation of such patients should include an assessment of their lifestyle vis a vis acculturation to the institutional setting, which has a strong influence on both the pathological aspects and "healthy" aspects of patients' makeup. Thus some scales of commonly used data collection inventories were altered for this study, leaving them with unknown psychometric properties. For this reason, a fresh evaluation of the validity and reliability of these measurements in the context of this study was necessary.
Patient assessments were conducted in December 1998, when the final wave of discharges from the psychiatric hospital was implemented, and they continued until December 2002. Intermediate assessments were made at three months, six months, and one year after discharge and in December 2000 and December 2001, for a total of six follow-up assessments. Institutional review board approval was obtained for the study.
Participants
The final wave of discharges from the psychiatric hospitals of Collegno and Grugliasco involved 356 patients. Before discharge, a commission independent of the caregiver team identified patients whose symptoms were mostly attributable to aging. These 180 patients entered a community-based nonpsychiatric program of socialization and care and were thus not included in this study, which focused on the remaining 176 patients, who were classified as psychiatric patients. After complete description of the study to the participants, written informed consent was obtained.
Measures
Participants were assessed in three areas: psychological condition, autonomy, and relational skills. Psychological condition was evaluated with the 18-item Brief Psychiatric Rating Scale (BPRS) ( 12 , 13 , 14 ). An overall score (the sum of scores for individual items) was calculated, as well as five subscores, with the solution proposed by Guy ( 15 ): thought disturbance, anergia, anxiety-depression, activation, and hostile-suspiciousness.
Autonomy and relational skills are two domains commonly used by psychiatric services in Italy to develop therapeutic programs. Autonomy concerns the basic skills of understanding, communication, and management of day-to-day life. Relational skills entail to the ability to express needs (volition) and to interact adequately with others. Because scales to assess the two domains were specifically constructed to meet clinical requirements for this study, their psychometric properties are unknown. Therefore, before data were analyzed, exploratory factor analysis was performed to check the applicability and validity of each dimension of the two tools used for the study. The total explained variance was 57% for the autonomy scale and 49% for the relational scale. Cronbach's alpha coefficients were then calculated to measure the reliability of each dimension in terms of internal consistency. Coefficients ranged from .76 to .94, with a mean of .86. Finally, the scales thus obtained were used with patients whose clinical condition was similar to that of study participants but who had no history of long stays in a psychiatric hospital. Interrater reliability was evaluated by calculating the Pearson correlation coefficient between scores attributed independently by two different raters to a sample of 50 patients. The mean correlation coefficient was .86. The two psychiatrists who used the two scales to assess patients in this study had participated in a training program aimed at maximizing uniformity of scores; on completion of training, intraclass correlation coefficients were .80 or better for these two scales and the BPRS.
Autonomy skills were measured on a scale comprising 30 items subdivided into four subscales: communication, autonomy in activities of daily living, cognitive skills, and social contacts. Each item was evaluated on a scale from 1 to 4, with 1 indicating maximum dysfunction and 4 indicating minimum dysfunction. The items were selected on the basis of factor analysis of an inventory comprising 46 items inspired by the Instrumental Activities of Daily Living Scale ( 16 ) and by the Index of Autonomy in ADL ( 17 ). Both had been used for clinical purposes in assessing patients in the psychiatric hospital. Relational skills were assessed on a scale of 14 items that were subdivided on the basis of factor analysis into two dimensions: volition and aggression. Each item was scored on a scale from 1 to 4, with 1 indicating maximum dysfunction and 4 indicating minimum dysfunction. [An appendix with examples of items from scales used to assess the two domains is available as an online supplement to this article at ps.psychiatryonline.org .]
Data analysis
Only participants for whom data were complete on every scale item were included in analysis of data from that scale. Thus some analyses involved fewer than the 118 patients who completed the final follow-up assessment. This was especially the case with the BPRS, which contains items that are sometimes impossible for the psychiatrist to administer to long-stay patients. The distribution of missing data was not random; thus insertion procedures could not be applied. No particularly striking patterns emerged. However, we identified a subgroup characterized by missing data for scale items that required the respondent to describe feelings he or she had experienced. The patients in this subgroup nonetheless showed an improvement similar to that of the rest of the study sample in terms of other measurable variables.
Data were analyzed with SPSS, version 11.5. The trend of scores on each scale was evaluated by analysis of variance for repeated measures, in the GLM procedure of the SPSS package, taking various administration times as the intraindividual factor. Post hoc comparisons were produced with the Bonferroni correction for multiple comparisons ( 18 ).
Results
Patient characteristics
All 176 participants were Caucasian; 109 were men, and 67 were women. The mean±SD age of participants was 63.0±9.9 (range 43–87 years). The patients were not categorized on the basis of length of stay, because the most recent admissions occurred in the late 1970s. The median stay was 37 years. Thus all participants had experienced very long stays. Most participants had a high level of disability and comorbid general medical disorders. A total of 128 patients (73%) had a diagnosis of schizophrenia or another psychotic disorder. The remaining diagnoses were mood disorder (N=18, 10%), personality disorders (N=9, 5%), and mild or moderate mental retardation (N=21, 12%).
Patients were resettled in three types of community-based facilities: 101 in sheltered communities with staff on site 24 hours a day, 24 in supported apartments with daily support ( 19 , 20 ), and 49 in residential health care facilities. Two patients returned to the home that they had occupied before their hospitalization. Pharmacological treatment was continued for all patients.
Success of follow-up
As Table 1 shows, 118 of the 176 participants assessed at discharge completed all six follow-up assessments. Between discharge and the final assessment, 34 patients died and 24 were transferred to facilities for the elderly because disability resulting from age-related decline was more salient than that resulting from psychiatric symptoms. Patients who were successfully followed up thus constituted 83% of those alive in December 2002—or 100% of those who were alive and continued to meet inclusion criteria for the study.
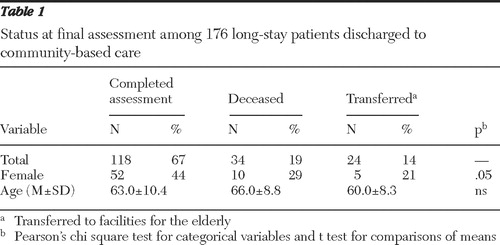 |
The mean age did not significantly differ between the 118 patients who completed the assessments and the 58 who did not. Although there was a higher proportion of men in the group who did not complete the assessments, this result was apparently not closely connected to a difference in mean age, because at the beginning of the study the mean age of women was 65 years, compared with 63 years for the men. The mortality rate, which was approximately 20% for the four years, is not significantly different from findings previously reported in studies of institutionalized psychiatric patients, whether discharged or not ( 21 ).
Clinical outcome
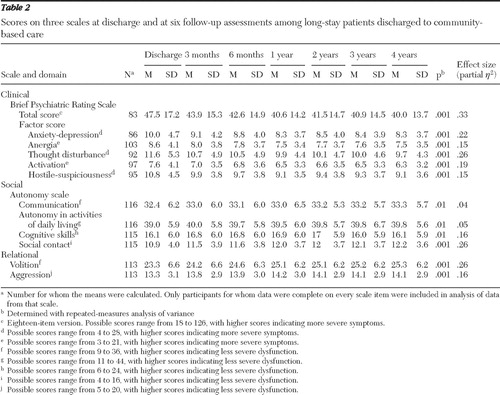
As Table 2 shows, total scores on the BPRS and on all five BPRS subscales indicated improvement, although to differing extents. The total score improved significantly as the assessments progressed, with an effect size of .33. From the first follow-up, a significant variation (p<.001) emerged from the post hoc comparisons. The most marked improvements in subscale scores were for thought disturbance (effect size=.26) and anxiety-depression (effect size=.22), and the improvements also were evident from the first follow-up (p<.001 in both cases). The other subscale scores indicated less marked improvements, although the changes were statistically significant.
 |
Social outcome
Autonomy scale. As shown in Table 2 , slight improvements were seen in communication, autonomy in activities of daily living, and cognitive skills. Although the improvements were statistically significant, in concrete terms they would appear to indicate stability of these skills over time.
The score for social contact indicated a more marked improvement (effect size=.26). A significant improvement was evident at the three-month follow-up (p=.001); the social contact score stabilized in the subsequent interval, with no significant improvement at the six-month follow-up; it again rose significantly at the assessment one year after discharge (p< .001). The remaining assessments indicated a slight but steady nonsignificant improvement.
Relational scale. An improvement was evident on both subscales—volition and aggression—but only for volition was the effect size (.26) significant ( Table 2 ). The improvement in volition was steady and significant from discharge to the first follow-up (p=.007) and for all intervals, except for that between the one- and two-year follow-ups. Improvement of scores on the aggression subscale indicated a moderate effect size, with stability and slow but steady progress.
Discussion
This study evaluated discharge from a psychiatric hospital of a final group of institutionalized patients. Therefore, the results do not apply to the initial phase of hospital closure but only to the final step in the process. The final phase had two main features. First, the process had to respect deadlines set by Italian law, which imposed definitive closure of all psychiatric hospitals as the conclusion of a discharge process begun in the late 1970s. Second, a heated debate ensued among psychiatric hospital staff about whether it was appropriate to carry out the law's requirements. In the minds of the professionals involved in this phase, there were real fears that discharge would amount to uprooting the patients from their home, with dramatic negative outcomes.
The successful outcome of the change to care in the community was not a foregone conclusion for three main reasons. The patients had been involved for years in resocialization treatment during their hospitalization, and at no point had they been deemed eligible for discharge to the community. In addition, the psychiatric hospital had been their home—in many cases for more than 30 years—and there was a risk that such a radical change would harm them. Also, the patients in the final discharge wave were those most difficult to resettle and had previously been excluded from the discharge process. It is doubtful whether such a step would have taken place without a fixed legislative deadline.
Clinical outcome
The results indicate that discharge led to a positive general trend, as evaluated by clinical and functional scales. The improvement appeared to be stable and progressive over time, although obviously a patient's age may have influenced this trend. Indeed, preconceptions of some psychiatric hospital staff about the chronicity of illness of these patients might have led them to treat some long-stay patients as geriatric rather than psychiatric cases. It is noteworthy that improvement was most marked in the BPRS domain of thought disturbance, because many patients had this clinical condition. The decrease in symptoms related to anxiety and depression may have been a consequence of the improvement in psychotic symptoms ( 22 ). This hypothesis, which warrants targeted research, stems from the reasonable assumption that such a radical change in living arrangements would in itself raise anxiety levels among these former patients, along with levels of depression and regression. The reduction in psychotic symptoms, on the other hand, might decrease the effects of such a potentially traumatic transition, inducing an improvement in other psychological spheres, including anxiety and depression.
Autonomy and relational outcome
Among skills connected with patients' autonomy, the socializing aspect in particular substantially improved over time, which has been found in other studies ( 7 ). Improvements in social contacts may be partly due to the difference in approaches to rehabilitation between professionals in the community and those in the hospital. Patients do not appear simply to be spectators in regard to their larger social networks; rather, the increase in social contacts underlies a true personal change. Patients develop skills connected with the management of relationships, taking advantage of opportunities offered them in the new context.
This hypothesis is supported by the assessment of relational outcomes, where evidence of improvement was found in the area of volition. The improvement in this sphere, which concerns the dimensions of personal initiative and of willingness to share one's experiences and collaborate with staff and other patients to achieve common goals, demonstrates the effects of the change in setting that are the most transforming for the patient. This finding suggests that interventions able to further the resocialization process are effective.
Limitations
Analyses showed that the two scales used to measure autonomy and relational skills may be considered valid and reliable. However, one of the limits of this study is the choice of tools used for data collection, which were designed for clinical use rather than research purposes. The study design makes it impossible to rule out the possibility that factors other than those connected with hospital discharge may have had an influence during the four years of the study. Nor are precise data available on the degree of satisfaction expressed by patients in regard to such a significant life change.
Conclusions
The few empirically based studies of the process of closing psychiatric hospitals in Italy have examined it from various viewpoints: in terms of access to other types of facility ( 20 ), in more general terms than those described in this study ( 6 ), and in regard to patients who remained in the hospitals ( 23 ). The findings justify moderate optimism in regard to the possibility that a radical change in living environment can modify certain patient characteristics that are typical of institutionalization.
Although a recent U.S. study showed a trend toward increased rates of admission to psychiatric hospitals ( 24 ), our findings strengthen the conviction of many individuals that discharge from psychiatric hospitals to community-based facilities can be a positive opportunity for patients. Patients in Italy who had very long institutional stays showed an ability, through a change in setting, to increase their psychological and relational resources. Our results suggest that the community setting gives rise to an improvement in patients' mental health because of the reduced degree of institutionalization and the consequent increase in relational networks.
Acknowledgments and disclosures
The authors report no competing interests.
1. Piccinelli M, Politi P, Barale F: Focus on psychiatry in Italy. British Journal of Psychiatry 181: 538–544, 2002Google Scholar
2. De Girolamo G, Cozza M: The Italian psychiatric reform: a 20-year perspective. International Journal of Law and Psychiatry 23:197–214, 2000Google Scholar
3. Talbott JA: Deinstitutionalization: avoiding the disasters of the past. Psychiatric Services 55:1112–1115, 2004Google Scholar
4. Fisher WH, Barreira PJ, Geller JL, et al: Long-stay patients in state psychiatric hospitals at the end of the 20th century. Psychiatric Services 52:1051–1056, 2001Google Scholar
5. Räsänen S, Hakko H, Herva A, et al: Community placement of long-stay psychiatric patients in Northern Finland. Psychiatric Services 51:383–385, 2000Google Scholar
6. Barbato A, D'Avanzo B, Rocca G, et al: A study of long-stay patients resettled in the community after closure of a psychiatric hospital in Italy. Psychiatric Services 55:67–70, 2004Google Scholar
7. Leff J, Trieman N: Long-stay patients discharged from psychiatric hospitals: social and clinical outcomes after five years in the community: the TAPS Project 46. British Journal of Psychiatry 176:217–223, 2000Google Scholar
8. Thornicroft G, Bebbington P, Leff J: Outcomes for long-term patients one year after discharge from a psychiatric hospital. Psychiatric Services 56:1416–1422, 2005Google Scholar
9. Rothbard AB, Kuno E: The success of deinstitutionalization: empirical finding from case studies on state hospital closures. International Journal of Law and Psychiatry 23:329–344, 2002Google Scholar
10. Rigby M, Lindmark J, Furlan PM: The importance of developing an informatics framework for mental health. Health Policy 45:57–67, 1998Google Scholar
11. Dunn M, O'Driscoll C, Dayson D, et al: The TAPS Project: 4. an observational study of the social life of long-stay patients. British Journal of Psychiatry 157:842–848, 1990Google Scholar
12. Overall JE, Gorham DR: The Brief Psychiatric Rating Scale. Psychological Reports 10:799–812, 1962Google Scholar
13. Lukoff D, Nuechterlein KH, Ventura J: Manual for expanded Brief Psychiatric Rating Scale (BPRS). Schizophrenia Bulletin 12:594–602, 1986Google Scholar
14. Morosini P, Casacchia M: Italian translation of the expanded Brief Psychiatric Rating Scale (BPRS 4.0) [in Italian]. Rivista di Riabilitazione Psichiatrica e Psicosociale 3:199–228, 1995Google Scholar
15. Guy W: ECDEU Assessment Manual for Psychopharmacology. Rockville, Md, US Department of Health, Education, and Welfare, 1976Google Scholar
16. Lawton MP, Brody EM: Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist 9(3):179–186, 1969Google Scholar
17. Katz S, Downs TD, Cash HR, et al: Progress in development of the index of ADL. Gerontologist 10(1):20–30, 1970Google Scholar
18. Diggle PJ, Heagerty PJ, Liang K: The Analysis of Longitudinal Data. New York, Oxford University Press, 2002Google Scholar
19. Tibaldi G, Munizza C, Pasian S, et al: Indicators predicting use of mental health services in Piedmont, Italy. Journal of Mental Health Policy and Economics 8:95–106, 2005Google Scholar
20. De Girolamo G, Picardi A, Micciolo, et al: Residential care in Italy: national survey of non-hospital facilities. British Journal of Psychiatry 181:220–225, 2002Google Scholar
21. Valenti M, Necozione S, Busellu G, et al: Mortality in psychiatric hospital patients: a cohort analysis of prognostic factors. International Journal of Epidemiology 26:1227–1235, 1997Google Scholar
22. Furlan PM, Picci RL: Alcohol, Alcoholics, and Alcoholism [in Italian]. Torino, Bollati e Boringhieri, 1990Google Scholar
23. Mastroeni A, Bellotti C, Pellegrini E, et al: Clinical and social outcomes five years after closing a mental hospital: a trial of cognitive behavioural interventions. Clinical Practice and Epidemiology in Mental Health 1:25, 2005Google Scholar
24. Manderscheid RW, Atay JE, Crider RA: Changing trends in state psychiatric hospital use from 2002 to 2005. Psychiatric Services 60:29–34, 2009Google Scholar



