Daily Functioning and Information-Processing Skills Among Persons With Schizophrenia
People with schizophrenia consistently report some impairment in their performance of daily activities ( 1 , 2 ). They often complain about the effects of cognitive difficulties, such as attention and memory problems, on their daily life ( 3 ). Many perceive that being involved in daily activities supports a sense of competence and pleasure ( 4 ) and that this influences their quality of life ( 5 , 6 ). Consequently, independent living and ability to perform daily activities are identified as treatment outcome priorities by persons with schizophrenia and are major criteria for recovery from this disorder ( 7 , 8 ).
Studies using performance-based assessments of functional capacity, such as the Test of Adaptive Behavior in Schizophrenia ( 9 ) and the UCSD Performance-Based Skills Assessment ( 10 ) and its brief version ( 11 ), have found that functional capacity is associated with other global measures of functional outcome and predicts residential independence ( 9 , 10 , 11 ). If performance of daily activities is important for residential independence and the quality of life of persons with schizophrenia, then more specific information on the limitations that impede their performance is needed.
Unfortunately, the small number of studies that have focused on functional limitations provide insufficient information on the observable behaviors affecting the mastery and competence of daily activities. This gap can be partly attributed to the daily-activities assessments used for global indictors of performance ( 12 , 13 , 14 , 15 , 16 ). When more specific information was obtained with these assessments, methodological limitations restricted the generalizability of results ( 17 ). These studies are therefore limited in their usefulness to guide rehabilitation interventions for persons with schizophrenia.
To establish appropriate treatment goals and interventions for these clients, it is mandatory not only to identify the functional limitations that have the most impact on performance of daily tasks but also to gain an understanding of the variability of functional limitations within a group of persons with similar psychiatric diagnoses ( 18 ). Taking these considerations and the limitations of previous studies into account, we were guided for this study by two main questions. First, in daily task performance, what are the functional limitations among persons with schizophrenia? Second, do subgroups of participants have similar profiles based on the functional limitations revealed during the performance of a daily task?
Methods
Participants
For this descriptive study, two psychiatric outpatient clinics were designated as recruitment centers in the Montreal area of Quebec. Between January 2006 and February 2007, a total of 82 persons with schizophrenia, referred by their mental health teams, agreed to participate in this study. Inclusion criteria included having a DSM-IV diagnosis of schizophrenia or schizoaffective disorder confirmed by a treating psychiatrist, being between 18 and 60 years old, living in the community, being familiar with meal preparation, speaking French, and displaying a stable state without any major medication change for at least two months before the study. Persons presenting with a major physical disability, a current substance abuse problem, cognitive deficits of organic origin (such as dementia), or mental retardation were excluded. This study was approved by the ethics committees of the hospitals where it took place. After complete description of this study to the participants, written informed consent was obtained. Participants were remunerated $30 for their expenses.
Measures
Clinical assessment. The Positive and Negative Syndrome Scale (PANSS) ( 19 ) was used to assess the severity of symptoms.
Cognitive functioning assessments. Four subtests that came from the Cambridge Neuropsychological Test Automated Battery (CANTAB) ( 20 ), with CANTAB Eclipse version 2.0, were administered, and specific indexes were used: motor screening, which measures visuomotor coordination by mean latency time; the paired-associates learning task (PAL),where recall is measured with the first-trial memory score and learning is measured by the total errors adjusted score; Stockings of Cambridge (SOC), which measures planning with the number of problems solved in minimum moves; spatial working memory, which measures visuospatial working memory with the number of errors made between searches as well as with a strategy score that indicates the use of a more systematic strategy. The interference score of the Stroop Color-Word Test (Golden version) was used to assess selective attention ( 21 ).
Community functioning assessments. We used the Independent Living Skills Survey ( 22 ) interview format of the French self-report version of the questionnaire ( 23 ). The Multnomah Community Ability Scale was completed by the clinician ( 24 ). The French version of this tool was used ( 25 ).
Performance-based assessment. The Perceive, Recall, Plan and Perform (PRPP)System of Task Analysis is a standardized, criterion-referenced assessment ( 26 ) and was administered for the assessment of information-processing skills during daily activity performance. In stage 1 of the PRPP System, errors of accuracy, omission, repetition, and timing are identified during performance. In stage 2 of the PRPP system, which is the focus of this article, cognitive task analysis is used to determine the efficiency of information-processing skills underlying the performance of tasks. These information-processing skills are categorized into four quadrants: perceive, recall, plan, and perform. Each quadrant is divided into three subquadrants, containing either two or three "descriptors" or skills. A total of 34 observable behavioral skills are considered individually or cumulatively to identify processing strengths and deficits and are scored on a 3-point rating scale. A global PRPP system processing score and specific PRPP system quadrant scores are calculated. For the purpose of this study, functional limitations were defined as problematic information-processing skills. This performance-based assessment has demonstrated its utility in the assessment of persons with schizophrenia, and a more complete description of the tool and its psychometric properties appears in two recent studies ( 27 , 28 ).
Procedure
All cognitive assessments were administered by trained evaluators. The daily task performance assessment was completed by either of two occupational therapists with experience in psychiatry who were located in two outpatient clinics and trained in the use of the PRPP system. Both therapists observed and rated participants during the meal preparation task, which included the preparation of meat, potatoes, and a cake and instructions that all dishes be ready at the same time ( 27 ). A maximum delay of ten minutes between completion of the first and last dishes was considered acceptable, but participants were not aware of this criterion. All participants were met in the occupational therapy department kitchen in the hospital where they were recruited. Each participant answered a brief questionnaire created for this study, the "familiarity with the meal preparation task questionnaire," which was used in evaluating the participant's level of familiarity with each dish. The scale ranges from 0, "never used the kitchen or cooked this dish," to 3, "cooks this dish regularly (every month or more often)."
Data analysis
To answer the first research question, about functional limitations, descriptive statistics, including means, frequencies, and standard deviations, were calculated for all sociodemographic, clinical, cognitive, and functional variables. PRPP system descriptors with mean scores below 2, indicating that the descriptor behavior negatively affects task performance, were defined as problematic PRPP system descriptors. To answer the second research question, about specific profiles among subgroups, the sample was divided according to the score obtained on the PRPP system. Participants with a score equal to or higher than 85% of the PRPP system maximum total score (≥86.7 out of 102) were considered highly efficient, and those with a score lower than 85% of the PRPP system maximum total score (<86.7 out of 102) were considered to have low efficiency. The cutoff was thought to represent a level of mastery, with the allowance that mastery does not exclude the presence of minor performance errors. A cutoff score for mastery level at 85% has been generally accepted in the criterion-referenced assessment literature ( 29 , 30 ). Both groups were compared on functional, cognitive, clinical, and sociodemographic variables with t tests and Pearson's chi square. Because these analyses were still at the exploratory level, statistical significance was set at p≤.05.
Results
Fifty-two (63%) participants were men, with a mean±SD age of 41.70±9.90 years. Fifty-seven (69%) were unemployed, and 40 (49%) were living independently, alone in either an apartment or a room. The average number of years of education was 11.71±2.90 years. Seventy-five participants (91%) were Caucasian, one (1%) was Asian, two (2%) were Haitian, and four (5%) were African.
Functional limitations in the group of participants
The PRPP system revealed a number of errors committed by the participants at stage 1 of this assessment. The most common errors were accuracy errors (13.71±5.82 errors). These were noted when an attempt to complete a step in the meal preparation became problematic or when the quality of the outcome was questionable. Other types of errors were less frequent (repetition errors, .52±.87; omission errors, 1.68±1.59; and timing errors, .73±1.27). Having the dishes ready at the same time was problematic for 32 (39%) participants, who took longer than the acceptable delay, and 37 (45%) participants did not choose to start the task with the dish that took the longest to prepare (the cake).
When these errors were analyzed in stage 2 of the PRPP system, difficulties in the plan and perceive quadrant descriptors, as well as in a number of recall quadrant descriptors, were most significant ( Table 1 ). Descriptors such as "modulates," "searches," and "recalls steps," to name a few, obtained mean scores below 2 out of a maximum score of 3.
 |
Subgroups with similar profiles of functional limitations
The high-efficiency group included 36 participants, and the low-efficiency group included 46 participants. Results from the comparison of these two groups on main variables are presented in Table 2 . The high-efficiency group differed significantly from the low-efficiency group on all functional variables. Both groups also differed on the proportion of persons living independently: significantly more persons were independent in their housing in the high-efficiency group (25 independent versus 11 dependent; 69% of group independent) than in the low-efficiency group (15 independent versus 31 dependent; 33% of group independent) ( χ2 =10.96, df=1, p=.001).
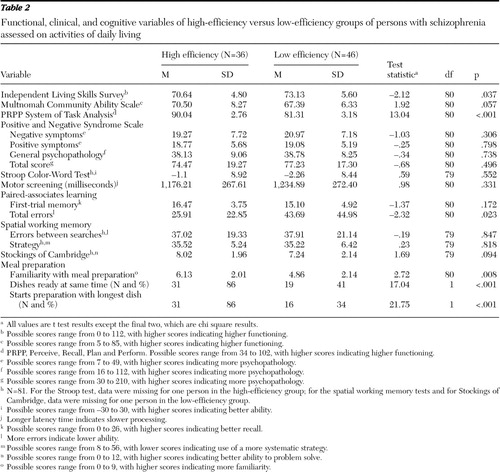 |
The high- and low-efficiency groups differed significantly on the PAL visual memory test, specifically on the learning scores (total errors). There were no significant differences between these two groups on the severity of symptoms, gender proportions, age, years of education, and time to psychiatric follow-up.
Because familiarity with meal preparation was significantly different for both groups, and familiarity was thought to possibly affect performance on this daily task, a generalized linear model was tested to control for the effect of familiarity on PRPP system scores. High-efficiency group scores were still significantly different from low-efficiency group scores on PRPP system total scores ( χ2 =114.05, df=1, p<.001) and on the perceive ( χ2 =23.93, df=1, p<.001), recall ( χ2 =86.77, df=1, p<.001), plan ( χ2 =89.24, df=1, p<.001), and perform quadrants ( χ2 =45.68, df=1, p<.001).
Discussion
This study was designed to explore functional limitations in the context of task performance by persons with schizophrenia and whether different profiles are defined by these functional limitations. This study was different from previous studies of functional capacity of persons with schizophrenia—some of which also included a cooking task ( 9 , 14 , 16 , 17 )—in that the description of limitations included specific information-processing skills. This level of detail was made possible with the use of a performance-based assessment that is skill oriented, the PRPP system of task analysis, which uses a cognitive task analysis. Moreover, results from this study suggest that the information obtained about these limitations closely reflects real-world functioning. Participants who belonged to the high-efficiency group retained residential independence for the most part and had more autonomous community tenure than participants who belonged to the low-efficiency group. Hence, this performance-based assessment captured the "here and now" level of capacity, notwithstanding practice or experience with this meal preparation task.
Not unexpectedly, the participants had difficulties in the different stages of information processing. Limitations in skills such as searching, locating, recalling steps, and identifying obstacles had an impact on the execution of steps in the meal preparation task. Selective attention and visual search deficits have been consistently reported among persons with schizophrenia undergoing neuropsychological testing ( 31 , 32 , 33 ). Behaviors related to decision-making, problem-solving, and error-monitoring abilities have been reported to be deficient among persons with schizophrenia ( 34 , 35 , 36 ). Findings in this study suggest that functional limitations identified during a performance-based assessment may present a more ecological perspective of the difficulties encountered by these persons.
Problems in the perform quadrant of the PRPP were less frequent and less severe than in the other quadrants for this sample. The group had less difficulty to start (initiate), continue, and persist in the task, and we observed almost no perseverative behaviors (problems with "stop"). It is possible that this type of structured task, with specific instructions and with a given level of complexity, did not elicit problems related to initiation, effort, motivation, and persistence that are known to be problematic for some people with schizophrenia ( 9 , 37 , 38 ).
The results regarding the differences between the high- and low-efficiency groups highlight the importance of one specific cognitive characteristic. Only one neuropsychological test, the visuospatial associative learning test, differentiated the high-efficiency group from the low-efficiency group, with the high-efficiency group having better scores on this test. These results suggest that the capacity to memorize and to learn is one of the key characteristics of functional capacity and that a greater capacity to retain information may increase the chances for better community tenure. These findings are in line with the research literature on cognition and community functioning that emphasizes the importance of assessing long-term memory and learning potential, which evaluates learning as it occurs within the assessment session, for community functioning ( 39 ).
Similar results were obtained in another study. Stip and collaborators ( 40 ) used neuropsychological tests of attention, memory, and executive function to compare persons with schizophrenia, who were grouped on the basis of their performance on daily tasks and on their level of residential autonomy. As in our study, they found that only the long-term memory test differentiated the groups and that no significant differences were apparent between the groups on the executive function tests. The authors suggested that the most autonomous persons may have developed specific mnemonics and strategies to help them negotiate day-to-day problems, as could have been the case in this investigation.
Findings from this study should be considered in regard to further development of rehabilitation interventions and strategies. If this performance-based assessment is helpful in capturing how limitations affect task performance, then it may be useful to target these specific problematic skills in rehabilitation interventions. Moreover, interventions could be developed to further support the generalization of these skills to a variety of tasks. For example, teaching and training of processing skills such as "searches and locates" could be integrated into actual or new strategies for daily living skills. Findings from this study tend to support the importance of learning ability relative to functional capacity and real-world outcomes, such as the greater degree of residential independence in the community. Authors have suggested specific approaches that take into account the impact of these types of deficits on the design of procedures to enhance learning, such as errorless learning strategies and modeling ( 41 ). Recently, learning potential has been recognized as contributing to the prediction of rehabilitation outcome ( 42 ) and to work skills acquisition ( 43 ).
One limitation of this study is the relatively high number of comparisons and tests, which creates an elevated risk of type I error. Our study was considered to be at the exploratory level; therefore, the analyses for which the significance level was relatively low may be best viewed as needing further exploration and research. At one of the sites, the occupational therapist conducted the cognitive and functional assessments with some participants because other evaluators were unavailable, because of room scheduling, or to accommodate participants' availability. However, the occupational therapist was aware of the potential risk of bias; also, the computerized cognitive assessment was thought to diminish the risk of bias because results were calculated by the computer program and were not known before the end of data collection. As for functional assessment, the PRPP system task analysis grid developed for this study was, therefore, especially useful to avoid bias.
Not surprisingly, the classification into high and low efficiency according to the PRPP system scores did not perfectly discriminate between persons who lived dependently versus independently. Although performance efficiency in meal preparation was helpful to differentiate the level of housing independence of the participants, obviously more daily tasks should be assessed before determining the need for supervision and the level of within-community functioning of persons with schizophrenia. Also, different types of supervision are offered by health services organizations, therefore enabling more dependent persons to live on their own. Other problems, such as substance abuse, nonadherence to treatment, and absence of family members or social network, may be reasons for requiring a more structured environment.
Conclusions
Skill-oriented assessments are needed to better evaluate functional capacity in behavioral and measurable terms ( 44 ). Moreover, Bellack and colleagues ( 45 ) have suggested that rehabilitation should focus on improving functional skills rather than cognitive capacities. Findings of this study suggest that a performance-based assessment, the PRPP system of task analysis, was useful to identify limitations in a number of information-processing skills during performance of a daily task. These findings add an ecological perspective to the body of research literature on cognition and function in schizophrenia that is mainly based on neuropsychological testing results. Toward the development of rehabilitation interventions, these findings underline the role of learning ability as a determinant of independent functioning, supporting the current research focus on learning potential. Different strategies should therefore be developed for the teaching and training of these functional skills to persons with schizophrenia.
Acknowledgments and disclosures
This study was supported by a grant from the Fonds de la Recherche en Santé du Québec.
The authors report no competing interests.
1. Walkup J, Gallagher S: Schizophrenia and the life course: national findings on gender differences in disability and service use. International Journal of Aging and Human Development 49:79–105, 1999Google Scholar
2. Ivarsson A-B, Carlsson M, Sidenvall B: Performance of occupations in daily life among individuals with severe mental disorders. Occupational Therapy in Mental Health 20:33–50, 2004Google Scholar
3. Prouteau A, Verdoux H, Briand C, et al: Self-assessed cognitive dysfunction and objective performance in outpatients with schizophrenia participating in a rehabilitation program. Schizophrenia Research 69: 85–91, 2004Google Scholar
4. Aubin G, Hachey R, Mercier C: The significance of daily activities in persons with severe mental disorders [in French]. Canadian Journal of Occupational Therapy 69:218–228, 2002Google Scholar
5. Aubin G, Hachey R, Mercier C: Meaning of daily activities and subjective quality of life in people with severe mental illness. Scandinavian Journal of Occupational Therapy 6:53–62, 1999Google Scholar
6. Haertl K, Minato M: Daily occupations of persons with mental illness: themes from Japan and America. Occupational Therapy in Mental Health 22:19–32, 2006Google Scholar
7. Fischer E, Shumway M, Owen R: Priorities of consumers, providers, and family members in the treatment of schizophrenia. Psychiatric Services 53:724–729, 2002Google Scholar
8. Liberman RP, Kopelowicz A, Ventura J, et al: Operational criteria and factors associated to recovery from schizophrenia. International Review of Psychiatry 14:256–272, 2002Google Scholar
9. Velligan D, Diamond P, Glahn D, et al: The reliability and validity of the Test of Adaptive Behavior in Schizophrenia (TABS). Psychiatry Research 151:55–66, 2007Google Scholar
10. Patterson T, Goldman S, McKibbin C, et al: UCSD Performance-Based Skills Assessment: development of a new measure of everyday functioning for severely mentally ill adults. Schizophrenia Bulletin 27:235–245, 2001Google Scholar
11. Mausbach B, Harvey P, Goldman S, et al: Development of a brief scale of everyday functioning in persons with serious mental illness. Schizophrenia Bulletin 33:1364–1372, 2007Google Scholar
12. Rempfer M: Independent living skills in people with schizophrenia: influence of clinical symptoms and cognitive functioning. Doctoral dissertation, University of Kansas, Department of Psychology, 1999Google Scholar
13. Hamera E, Brown C: Developing a context-based performance measure for persons with schizophrenia: the Test of Grocery Shopping Skills. American Journal of Occupational Therapy 54:20–25, 2000Google Scholar
14. Semkovska M, Bédard M, Godbout L, et al: Assessment of executive dysfunction during activities of daily living in schizophrenia. Schizophrenia Research 69:289–300, 2004Google Scholar
15. Semkovska M, Stip E, Godbout L, et al: Behavioral disorganisation in schizophrenia during a daily activity: the Kitchen Behavioral Scoring Scale. Brain and Cognition 48:546–553, 2002Google Scholar
16. Godbout L, Limoges F, Allard I, et al: Neuropsychological and activity of daily living script performance in patients with positive or negative schizophrenia. Comprehensive Psychiatry 48:293–302, 2007Google Scholar
17. Knight M: Cognitive function and food preparation ability in schizophrenia. Doctoral dissertation, University of Rhode Island, Department of Nursing, 2000Google Scholar
18. Girard C, Fisher A, Short M, et al: Occupational performance differences between psychiatric groups. Scandinavian Journal of Occupational Therapy 6:119–126, 1999Google Scholar
19. Kay SR, Fiszbein A, Opler LA: The Positive and Negative Syndrome Scale (PANSS) for schizophrenia. Schizophrenia Bulletin 13: 261–276, 1987Google Scholar
20. Levaux M-N, Potvin S, Sepehry A, et al: Computerized assessment of cognition in schizophrenia: promises and pitfalls of CANTAB. European Psychiatry 22:104–115, 2007Google Scholar
21. Golden CJ: Stroop Color and Word Test: A Manual for Clinical and Experimental Uses. Wood Dale, Ill, Stoelting, 1978Google Scholar
22. Wallace C: Functional assessment in rehabilitation. Schizophrenia Bulletin 12:604–624, 1986Google Scholar
23. Cyr M, Toupin J, Lesage A, et al: Assessment of independent living skills for psychotic patients: further validity and reliability. Journal of Nervous and Mental Disease 182:91–97, 1994Google Scholar
24. Barker S, Barron N, McFarland B, et al: A community ability scale for chronically mentally ill consumers: part I. reliability and validity. Community Mental Health Journal 30:363–379, 1994Google Scholar
25. Corbière M, Crocker A, Lesage A, et al: Factor structure of the Multnomah Community Ability Scale. Journal of Nervous and Mental Disease 190:399–406, 2002Google Scholar
26. Chapparo C, Ranka J: The PRPP System of Task Analysis: User's Training Manual. Lidcombe, New South Wales, Australia, University of Sydney, 2005Google Scholar
27. Aubin G, Chapparo C, Gélinas I, et al: Use of the Perceive, Recall, Plan and Perform System of Task Analysis for persons with schizophrenia: a preliminary study. Australian Occupational Therapy Journal, 2008. doi: 10.1111/j.1440-1630.2007.00725Google Scholar
28. Aubin G, Stip E, Gélinas I, et al: Daily activities, cognition and community functioning in persons with schizophrenia. Schizophrenia Research, 107:313–318, 2009Google Scholar
29. Millman J: Passing scores and test lengths for domain-references measures. Review of Educational Research 43:205–216, 1973Google Scholar
30. Watkins M, Kush J: Assessment of academic skills of learning disabled students with classroom microcomputer. School Psychology Review 17:81–88, 1988Google Scholar
31. Gold J, Fuller R, Robinson B, et al: Impaired top-down control of visual search in schizophrenia. Schizophrenia Research 94: 148–155, 2007Google Scholar
32. Lussier I, Stip E: Selective attention and schizophrenia before neuroleptic administration [in French]. L'Encéphale 25:576–583, 1999Google Scholar
33. Velligan D, Bow-Thomas C: Executive function in schizophrenia. Seminars in Clinical Neuropsychiatry 4:24–33, 1999Google Scholar
34. Carter C, MacDonald AW, Ross LL, et al: Anterior cingulate cortex activity and impaired self-monitoring of performance in patients with schizophrenia: an event-related fMRI study. American Journal of Psychiatry 158:1423–1428, 2001Google Scholar
35. Hutton SB, Murphy FC, Joyce EM, et al: Decision making deficits in patients with first-episode and chronic schizophrenia. Schizophrenia Research 55:249–257, 2002Google Scholar
36. Evans J, Chua S, McKenna P, et al: Assessment of dysexecutive syndrome in schizophrenia. Psychological Medicine 27:635–646, 1997Google Scholar
37. Carpenter W, Heinrichs D, Wagman A: Deficit and non-deficit forms of schizophrenia: the concept. American Journal of Psychiatry 145:578–583, 1988Google Scholar
38. Buchanan R: Persistent negative symptoms in schizophrenia: an overview. Schizophrenia Bulletin 33:1013–1022, 2007Google Scholar
39. Green M, Kern R, Braff D, et al: Neurocognitive deficits and functional outcome in schizophrenia: are we measuring the "right stuff"? Schizophrenia Bulletin 26:119–136, 2000Google Scholar
40. Stip E, Sablier J, Sepehry A, et al: Kitchen and schizophrenia: a crossroad activity of an ecological, occupational and neuropsychological assessment [in French]. Santé Mentale au Québec 32:159–179, 2007Google Scholar
41. Gold J, Bish J, Iannone V, et al: Effects of contextual processing on visual conditional associative learning in schizophrenia. Biological Psychiatry 48:406–414, 2000Google Scholar
42. Watzke S, Brieger P, Kuss O, et al: A longitudinal study of learning potential and rehabilitation outcome in schizophrenia. Psychiatric Services 59:248–255, 2008Google Scholar
43. Sergi M, Kern R, Mintz J, et al: Learning potential and the prediction of work skill acquisition in schizophrenia. Schizophrenia Bulletin 31:67–72, 2005Google Scholar
44. MacDonald-Wilson K, Nemec P, Anthony W, et al: Assessment in psychiatric rehabilitation, in Handbook of Measurement and Evaluation in Rehabilitation, 3rd ed. Edited by Boulton B. Baltimore, Brookes Publishing, 2002Google Scholar
45. Bellack A, Gold J, Buchanan R: Cognitive rehabilitation for schizophrenia: problems, prospects, and strategies. Schizophrenia Bulletin 25:257–274, 1999Google Scholar



