A Case-Control Study of Factors Associated With Multiple Psychiatric Readmissions
The beneficial aspects of reforms in the structure and delivery of psychiatric care, especially deinstitutionalization, have long been recognized, as have their drawbacks ( 1 ). After nearly five decades of intense psychiatric reform activity in several countries, it has become clear that deinstitutionalized individuals who have severe mental illness or who have difficulty accessing outpatient psychiatric services are prone to frequent hospital readmissions, and such trends have been observed in a multitude of contexts ( 2 , 3 , 4 , 5 , 6 , 7 , 8 ).
Psychiatric readmissions are a consequence of a complex combination of factors that go beyond the severity of the psychiatric disease and include availability of services, quality and continuity of care, and family and social support, among others. Several studies have identified strong predictors of readmission, such as poor treatment adherence ( 9 , 10 , 11 , 12 , 13 ), low level of education ( 11 , 14 ), deficient follow-up after hospital discharge ( 14 ), involuntary admission ( 3 , 15 ), lack of social or family support ( 11 , 16 ), and diagnoses of schizophrenia ( 17 ) and substance use disorders ( 10 , 18 ).
Even though the negative consequences of multiple psychiatric admissions have been well documented ( 19 ), readmission rates have been increasing worldwide ( 14 , 16 , 20 ). The same phenomenon has been observed in Brazil, where readmission rates range between 30% and 59% during the first four months after discharge ( 21 , 22 ). Mental health care reform in Brazil has attempted to reduce the separation of mental health care from general medical care by reducing the number of tertiary hospitals, increasing (not proportionally) the number of psychiatric beds in general hospitals, and creating community-based services that collaborate with primary care units and coordinate treatment, referrals, and social support. Community Psychosocial Care Centers (Centros de Atençäo Psicosocial, or CAPS) were created to play these roles and also to act as substitutes for psychiatric beds. These centers provide intensive day hospital care ( 23 , 24 ).
A better understanding of factors that reduce the likelihood of multiple psychiatric admissions is needed. Such knowledge can help planners to set priorities and to make appropriate services and resources available to patients and their families after hospital discharge. Given the gap in knowledge, the objective of this study was to investigate factors associated with multiple psychiatric admissions among adults age 18 and over. Specifically, our study focused on the role of service-related factors, such as registration with the primary care unit after discharge and use of community mental health services, and individual-level factors, such as treatment and medication adherence.
Methods
Study design and setting
This case-control study selected incident (as opposed to prevalent) cases from the two major public psychiatric hospitals in Porto Alegre, southern Brazil, during a 12-month period from January through December 2006. These hospitals, which receive public funds to cover admissions and serve mainly the greater Porto Alegre area, have a combined capacity for 310 inpatients. In a pilot study we observed that rates of readmission to the two hospitals were comparable and ranged between 40% and 60% in the five months before the study.
We calculated that a sample size of 300 in the case group and 300 in the control group was needed to permit detection of a relative rate of 1.5, with an alpha of .05 and a beta of .80. Cases were defined on the basis of number of admissions during the data collection phase; that is, individuals who had three or more psychiatric admissions in the two years before the current admission (N=307) were included. Given the recurrent nature of psychiatric admissions, a concurrent case-control design was adopted with the objective of estimating the relative rate of admission for the "exposures" under study. The case-control design allowed individuals in the case group to return to the population at risk after hospital discharge.
Individuals who had their first inpatient readmission during the study period (N=354) constituted the control group. Individuals in both the case group and the control group who had a previous admission that lasted more than six months were excluded, because exposure to the risk factors for readmission may not have been comparable for these patients. Only readmissions that occurred more than 48 hours after a discharge were counted as a readmission. Data for a subgroup of 41 individuals in the control group who had one or more readmissions in 2006 (subsequent to the index admission) were included in analyses for both groups and were also analyzed separately. Written informed consent was obtained after a complete description of the study to the participants.
Variables
Sociodemographic factors included age group (18–29, 30–49, and 50–69 years), gender, ethnicity (white or nonwhite), socioeconomic status-adjusted quintiles of the National Wealth Score ( 25 ), marital status (married or not married), employment (employed versus unemployed, retired, or receiving a disability pension), and living arrangement (with or without family). Factors related to psychiatric admission history were age at first admission (in years), length of first admission (in days), number of lifetime admissions, type of first admission or the earliest admission for which data were available (voluntary or involuntary), and diagnostic group (mood or anxiety disorders, substance use disorders, and schizophrenia or psychotic symptoms). Factors related to treatment after the most recent discharge (that is, the discharge preceding the current admission) included treatment adherence (outpatient visits and medication), use of subsidized or free medication, use of psychotherapy, distance from the place of residence to the hospital (in the same city, in the same metropolitan area, or outside the metropolitan area), type of outpatient services used (CAPS or usual care), and attending or being registered with the hospital's primary care unit after discharge.
Data sources and measurement
Data were collected in the same way for individuals in the case and control groups. Sociodemographic information was obtained during patient interviews by use of a precoded, structured questionnaire. Characteristics of previous psychiatric admissions, ICD-10 diagnosis, and treatment were abstracted from hospital records. The research team made daily visits to the hospitals to identify patients who were readmitted. After patients gave written informed consent, interviews were conducted and chart information was abstracted. For individuals who had previous admissions to hospitals other than the study hospitals, the research team abstracted data from the other charts.
Data analysis
After descriptive statistical analysis, multivariate analysis was conducted according to a predefined conceptual model. The model included four hierarchical levels or blocks of variables. The first (distal) level included all socioeconomic variables; the second level included psychiatric diagnosis and comorbid substance use disorder; the third level included psychiatric admission history and details of previous hospital admissions; the fourth (proximal) level contained the variables related to postdischarge events, such as adherence to medication, adherence to other forms of treatment, contact with the primary care unit, and distance from place of residence to the hospital.
For univariate and multivariate analyses, the variable sex was kept in the model and variance estimates were adjusted for hospital clustering. Poisson regression was used to estimate the relative rate of exposure for the case and control groups. Only variables with a p value of ≤.05 in the univariate analyses were included in the subsequent modeling procedures, defined as an intralevel multivariate analysis. The variables that had a p value of ≤.05 after adjustment in the intralevel phase of the multivariate analysis were entered into the hierarchical analysis. As defined in the conceptual framework, the variables from the distal level entered the hierarchical model first, followed by those from the second, third, and fourth levels. To report the effect of distal-level variables, the estimate of each variable was obtained before introduction of variables from the next level. Similarly, for each subsequent level, estimates were obtained before the introduction of the next group of variables. Variables in the multivariate model within each level and variables at the proximal level in the final model were kept in the model when the corresponding p value was ≤.05. All analyses were conducted with the Stata statistical package, version 10.0.
The protocol of this study was approved by the research ethics boards of both hospitals, according to national recommendations for scientific studies involving human subjects.
Results
Of the 307 patients in the case group and 354 in the control group, most were white and nonmarried ( Table 1 ). The mean±SD age of the overall sample was 35.9±11.1 years. There were 214 males (69%) in the case group and 231 males (65%) in the control group. Individuals in the case group were relatively younger at first admission than those in the control group (27.3±9.6 years and 30.7±11 years, respectively; p<.001). The first admission was also longer for those in the case group compared with the control group (33.2±22.5 and 30.7±22.3 days, respectively), but the difference was not statistically significant.
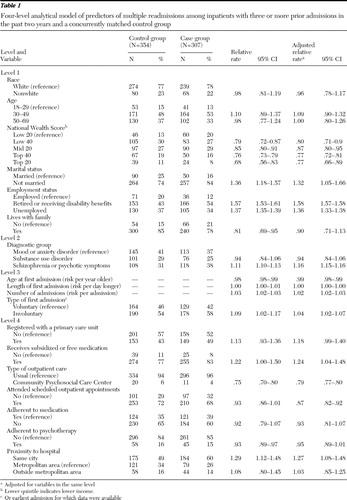 |
As shown in Table 1 , the univariate analysis found an inverse association between wealth and multiple readmissions. Patients in the highest wealth quintile had lower odds of multiple readmissions (adjusted relative rate [ARR]=.77) than those in the lowest quintile). Patients with multiple readmissions were more likely to be unmarried and unemployed, retired, or receiving a disability pension, even after intralevel adjustments. Patients with schizophrenia or psychotic symptoms were more likely than patients with mood or anxiety disorders to have multiple readmissions (ARR=1.16).
Several factors related to first psychiatric admission were associated with multiple subsequent readmissions ( Table 1 ). Age at first admission was inversely associated with multiple readmissions; patients who were younger at first admission were more likely to experience multiple readmissions, even after adjustment for current age. Those whose first admission was involuntary had higher odds of multiple readmissions than those with an involuntary first admission (or the first admission for which data were available).
Patients who received subsidized or free medication (that is, distributed by the government or a health service provider) were more likely than those who did not receive it to have multiple readmissions, even after adjustment for the wealth index (ARR=1.24). Individuals who had been referred to CAPS after the previous discharge were about 20% less likely than those referred to usual care to experience multiple readmissions (ARR=.79). Those who attended scheduled outpatient psychiatric appointments after the previous discharge had a lower likelihood of multiple readmissions than those who did not attend; however, adherence to medication was not a significant predictor of readmission. Individuals who lived in the same city as the hospital had a higher likelihood of readmission than those who lived in the greater metropolitan area (ARR= 1.27) ( Table 1 ).
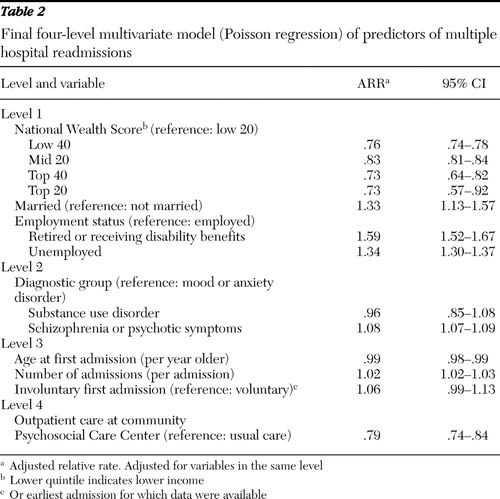
The final multivariate hierarchical analysis is presented in Table 2 . Even after adjustment for sociodemographic characteristics (level 1), a diagnosis of schizophrenia or psychotic symptoms was associated with multiple readmissions, as was age at first admission and number of previous admissions. Individuals who were referred to CAPS after the most recent hospital discharge were 20% less likely than those referred to usual care to have multiple readmissions, even after adjustment for sociodemographic characteristics, diagnosis, and factors related to the first psychiatric admission.
 |
Discussion
In Brazil, where this study was conducted, psychiatric and general medical care is funded through universal public coverage. Users of private care were thus not included in the sample, which limits the generalizability of our findings. To compare patients with a high number of readmissions and those with a low number, we used a conservative method of selecting patients for the control group, which should also be taken into account when interpreting these results because this selection method may have reduced the strength of the associations.
Results from this case-control study confirm previous findings of an association between multiple readmissions and age at first admission, number of previous admissions ( 26 , 27 ), type of first admission (involuntary) ( 28 ), lower socioeconomic status ( 15 ), and a diagnosis of severe mental illness (schizophrenia and psychotic symptoms) ( 14 , 26 , 27 ). Level of education was not associated with hospital readmission in this study. One previous study found such an association ( 14 ), whereas others did not ( 10 , 29 , 30 ). The lack of association may be a function of the limited variation in level of education in this sample.
Disease progression, and the greater frequency of hospital admissions that may accompany progression, are likely to reduce the probability of maintaining employment, which explains the association between lack of employment and multiple readmissions. Similar findings in regard to employment were reported in 1996 by Wieselgren and Lindstrom ( 31 ) and were attributed to disease progression. The relationship between multiple admissions and not being married is also consistent with previous findings ( 20 , 22 , 32 ). However, reverse causality may explain both associations, which indicates that studies with different designs are necessary to elucidate this relationship.
Lower socioeconomic status was a strong predictor of multiple hospital admissions. Individuals in the highest wealth quintile were almost 20% less likely to be readmitted to the hospital than those in the lowest quintile, although this association has been questioned in previous studies ( 22 ). We attribute our ability to identify such an association to use of a validated wealth score that is based on assets and calculated by taking into account the large geographical variation in socioeconomic status observed in Brazil ( 25 ).
We found no association between adherence to medication and multiple psychiatric admissions, although an inverse association has been reported in the literature. The absence of such findings may be a consequence of the study design, in which some individuals in the control group also experienced multiple readmissions (in the study year). Other possible explanations are that adherence to medication was self-reported by the patient or family members and that it may be a proxy for severity of the psychiatric illness. When analyses excluded data for individuals in the control group who had multiple admissions in the study year (that is, after the index admission), the results were not altered. However, when the analysis was limited to patients with schizophrenia or psychotic symptoms, adherence to medication was associated with a significantly lower likelihood of experiencing multiple admissions (data not shown).
A diagnosis of schizophrenia was not as strongly associated with multiple readmissions as in previous studies ( 28 ). The type of first admission was associated with multiple readmissions only before the analysis adjusted for socioeconomic status and psychiatric diagnosis. This association has been observed in previous studies ( 3 , 4 , 10 , 15 , 17 ) but has been deemed less important than psychiatric diagnosis ( 28 ). Although involuntary admission may be linked to a greater likelihood of noncompliance with treatment after discharge, which would lead to hospital readmission ( 33 ), this hypothesis is not supported by our findings.
Our results suggest that CAPS played an important and beneficial role in reducing psychiatric readmissions. Patients referred to these units were less likely to be readmitted than those referred to usual outpatient services, such as primary care units or hospital-based outpatient clinics. This association was significant even after adjustment for adherence to medication and other treatment and to receipt of subsidized medication ( Table 1 ). The finding that referral to CAPS seems to have prevented readmission for two out of ten psychiatric patients is of great interest and should be further explored. The importance of improving social support and providing psychosocial care to reduce the use of inpatient services has been previously demonstrated ( 34 , 35 , 36 ). The services provided by these centers address several social gaps facing patients, and center staff serve as case managers. However, CAPS are limited in their ability to accept new patients; the CAPS network is being rapidly scaled up, but it still falls short of the current demand.
CAPS, which are funded by the federal government, offer specialized mental health services that provide outpatient care as day or night treatment ( 24 ). These were created as part of the psychiatric reform program implemented in Brazil after the adoption of the Caracas Declaration ( 37 ) in the early 1990s. Although the network of these services has been expanded since then, and now includes two newly developed, specialized services targeting children and individuals with substance use disorders, little research has been conducted to evaluate the impact of CAPS, to describe the model, or to understand its cost-effectiveness. A recent review of the distribution of CAPS in Brazil found that 848 CAPS were registered as of June 2006 ( 22 ). The authors observed that the distribution of CAPS was uneven within the country and that the density was .9 CAPS per 200,000 population. Nevertheless, the progress of the implementation of these initiatives varies widely in Brazil and is still insufficient ( 22 ). Brazil's public health system provides treatment and access to psychotropic medication through municipal allocation of federal funds, and there has been a clear shift from hospital to community psychiatric care. Nevertheless, access to and coverage of community mental health services are deficient, and public investment in mental health has not been a priority of psychiatric reform efforts ( 1 ).
Our conservative choice of the concurrent case-control design allowed us to estimate the relative rate while also taking into account the possibility of multiple admissions because cases return to the population at risk after discharge ( 38 ). Our method of choosing patients for the control group is supported by previous studies of psychiatric readmission ( 20 , 21 ). However, some of the patients in the control group subsequently had multiple readmissions during the study year; the associations we found may have been stronger if the control group consisted only of patients who were not readmitted during the study year.
Conclusions
In light of our findings, the model of care offered by community mental health services should be further explored to identify the specific components responsible for the reduction of psychiatric readmissions.
Acknowledgments and disclosures
The authors report no competing interests.
1. Andreoli SB, Almeida-Filho N, Martin D, et al: Is psychiatric reform a strategy for reducing the mental health budget? The case of Brazil. Revista Brasileira de Psiquiatria. 29:43–46, 2007Google Scholar
2. Lay B, Lauber C, Rossler W: Prediction of in-patient use in first-admitted patients with psychosis. European Psychiatry 21:401–409, 2006Google Scholar
3. Feigon S, Hays JR: Prediction of readmission of psychiatric inpatients. Psychological Reports 93:816–818, 2003Google Scholar
4. Bernardo AC, Forchuk C: Factors associated with readmission to a psychiatric facility. Psychiatric Services 52:1100–1102, 2001Google Scholar
5. Druss BG, Bruce ML, Jacobs SC, et al: Trends over a decade for a general hospital psychiatry unit. Administration and Policy in Mental Health 25:427–435, 1998Google Scholar
6. O'Leary DA, Lee AS: Seven year prognosis in depression: mortality and readmission risk in the Nottingham ECT cohort. British Journal of Psychiatry 169:423–429, 1996Google Scholar
7. Goodpastor WA, Hare BK: Factors associated with multiple readmissions to an urban public psychiatric hospital. Hospital and Community Psychiatry 42:85–87, 1991Google Scholar
8. Marsh A, Glick M, Zigler E: Premorbid social competence and the revolving door phenomenon in psychiatric hospitalization. Journal of Nervous and Mental Disease 169:315–319, 1981Google Scholar
9. D'Ercole A, Struening E, Curtis JL, et al: Effects of diagnosis, demographic characteristics, and case management on rehospitalization. Psychiatric Services 48:682–688, 1997Google Scholar
10. Haywood TW, Kravitz HM, Grossman LS, et al: Predicting the "revolving door" phenomenon among patients with schizophrenic, schizoaffective, and affective disorders. American Journal of Psychiatry 152:856–861, 1995Google Scholar
11. Suzuki Y, Yasumura S, Fukao A, et al: Associated factors of rehospitalization among schizophrenic patients. Psychiatry and Clinical Neurosciences 57:555–561, 2003Google Scholar
12. Ucok A, Polat A, Cakir S, et al: One year outcome in first episode schizophrenia: predictors of relapse. European Archives of Psychiatry and Clinical Neuroscience 256:37–43, 2006Google Scholar
13. Weiden PJ, Kozma C, Grogg A, et al: Partial compliance and risk of rehospitalization among California Medicaid patients with schizophrenia. Psychiatric Services 55:886–891, 2004Google Scholar
14. Thompson EE, Neighbors HW, Munday C, et al: Length of stay, referral to aftercare, and rehospitalization among psychiatric inpatients. Psychiatric Services 54:1271–1276, 2003Google Scholar
15. Munk-Jorgensen P, Mortensen PB, Machon RA: Hospitalization patterns in schizophrenia: a 13-year follow-up. Schizophrenia Research 4:1–9, 1991Google Scholar
16. Hendryx MS, Russo JE, Stegner B, et al: Predicting rehospitalization and outpatient services from administration and clinical databases. Journal of Behavioral Health Services and Research 30:342–351, 2003Google Scholar
17. Cuffel BJ, Held M, Goldman W: Predictive models and the effectiveness of strategies for improving outpatient follow-up under managed care. Psychiatric Services 53:1438–1443, 2002Google Scholar
18. Miller DJ, Beck NC, Fraps C: Predicting rehospitalization at a community mental health center: a "double-crossed" validation. Journal of Clinical Psychology 40:35–39, 1984Google Scholar
19. Sullivan G, Wells KB, Morgenstern H, et al: Identifying modifiable risk factors for rehospitalization: a case-control study of seriously mental ill persons in Mississippi. American Journal of Psychiatry 152:1749–1756, 1995Google Scholar
20. Olfson M, Mechanic D, Boyer CA, et al: Assessing clinical predictions of early rehospitalization in schizophrenia. Journal of Nervous and Mental Disease 187:721–729, 1999Google Scholar
21. Amaral MA: Mental health care in health centers: study of the efficacy of the care given [in Portuguese]. Revista de Saúde Pública 31:288–295, 1997Google Scholar
22. Gastal FL, Andreoli SB, Quintana MI, et al: Predicting the revolving door phenomenon among patients with schizophrenia, affective disorders and non-organic psychoses. Revista de Saúde Pública 34:280–285, 2000Google Scholar
23. Mateus MD, Mari JJ, Delgado PG, et al: The mental health system in Brazil: policies and future challenges. International Journal of Mental Health Systems, 2:12, 2008Google Scholar
24. Jacob KS, Sharan P, Mirza I, et al: Mental health systems in countries: where are we now? Lancet 370:1061–1077, 2007Google Scholar
25. Barros AJD, Victora CG: A nationwide wealth score based on the 2000 Brazilian demographic census. Revista de Saúde Pública 39:523–529, 2005Google Scholar
26. Klinkenberg WD, Calsyn RJ: Predictors of receipt of aftercare and recidivism among persons with severe mental illness: a review. Psychiatric Services 47:487–496, 1996Google Scholar
27. Roick C, Heider D, Kilian R, et al: Factors contributing to frequent use of psychiatric inpatient services by schizophrenia patients. Social Psychiatry and Psychiatric Epidemiology 39:744–751, 2004Google Scholar
28. Rosca P, Bauer A, Grinshpoon A, et al: Rehospitalizations among psychiatric patients whose first admission was involuntary: a 10-year follow-up. Israel Journal of Psychiatry and Related Sciences 43:57–64, 2006Google Scholar
29. Hoffman H: Age and others factors relevant to the rehospitalization of schizophrenic outpatients. Acta Psychiatrica Scandinavica 89:205–210, 1994Google Scholar
30. Lewis T, Joyce PR: The new revolving-door patients: results from a national cohort of first admissions. Acta Psychiatrica Scandinavica 82:130–135, 1990Google Scholar
31. Wieselgren IM, Lindstrom LH: A prospective 1–5 year outcome study in first-admitted and readmitted schizophrenic patients; relationship to heredity, premorbid adjustment, duration of disease and education level at index admission and neuroleptic treatment. Acta Psychiatrica Scandinavica 93:9–19, 1996Google Scholar
32. Miettunen J, Lauronen E, Veijola J, et al: Socio-demographic and clinical predictors of occupational status in schizophrenic psychoses: follow-up within the Northern Finland 1966 birth cohort. Psychiatry Research 150:217–225, 2007Google Scholar
33. Fennig S, Rabinowitz J: Involuntary first admission of patients with schizophrenia as a predictor of future admissions. Psychiatric Services 50:1049–1052, 1999Google Scholar
34. Kent S, Fogarty M, Yellowlees P: Heavy utilization of inpatient and outpatient services in a public mental health service. Psychiatric Services 46:1254–1257, 1995Google Scholar
35. Kent S, Fogarty M, Yellowlees P: A review of studies of heavy users of psychiatric services. Psychiatric Services 46:1247–1253, 1995Google Scholar
36. Kent S, Yellowlees P: The relationship between social factors and frequent use of psychiatric services. Australian and New Zealand Journal of Psychiatry 29:403–408, 1995Google Scholar
37. Levav I, Restrepo H, Guerra de Macedo C: The restructuring of psychiatric care in Latin America: a new policy for mental health services. Journal of Public Health Policy 15:71–85, 1994Google Scholar
38. Rodrigues L, Kirkwood BR: Case-control design in the study of common disease: update on the demise of the rare disease assumption and choice of sampling scheme for controls. Journal of Epidemiology 19:205–213, 1990Google Scholar



