Prevalence of Serious Mental Illness Among Jail Inmates
According to the Bureau of Justice Statistics, during the 12 months ending at midyear 2007, there were 13 million admissions to local jails in the United States ( 1 ). At midyear 2007, local jails held 673,697 adult males and 100,047 adult females—figures that represent increases of 24.0% and 42.1%, respectively, since midyear 2000. The majority of these jail inmates were pretrial detainees ( 1 ).
Prisoners have a constitutional right to adequate health care, including mental health treatment ( 2 , 3 , 4 ), and the growth of local correctional populations has strained the limited capacity of jails to respond to the health needs of inmates ( 5 ). The situation is particularly challenging in the case of inmates with serious mental illnesses, who require specialized treatment and services ( 6 ). There has been consistent evidence that persons with mental illnesses are overrepresented in jails, and determining the extent of these higher rates is a first step to improved jail management and the development of alternatives to incarceration.
Prevalence estimates of mental illnesses in U.S. jails have varied widely depending on methodology and setting. Using survey methodology, a 1999 report from the Bureau of Justice Statistics (BJS) estimated that 16.3% of jail inmates reported either a "mental condition" or an overnight stay in a mental hospital during their lifetime ( 7 ). In 2006 BJS reported that 64% of jail inmates had a recent "mental health problem" ( 8 ). The 2006 findings were based on personal interviews conducted in the 2002 Survey of Inmates in Local Jails, and the rate of 64% included all inmates who reported one or more symptoms of any mental illness. Data on functional impairment and duration of illness were not collected, and inmates were not excluded if their symptoms were a result of general medical conditions, bereavement, or substance use ( 8 ). Although the methods used in this study are not consistent with other efforts to establish the prevalence of mental illnesses in jails, the findings are often, and mistakenly, cited as evidence of an escalating problem. More recently, Trestman and colleagues ( 9 ) evaluated a cohort of inmates who were not identified at intake as having a mental illness and found that over two-thirds met criteria for a lifetime psychiatric disorder, including anxiety disorders and antisocial personality disorder.
The most rigorous data on the prevalence of mental disorders among both male and female jail inmates were collected by Teplin, Abram, and McClelland ( 10 , 11 , 12 , 13 , 14 ) in the 1980s and 1990s in Cook County (Chicago), Illinois. The data were collected for the purpose of measuring severe mental disorders, which are not comparable to broader estimates of serious mental illness. These researchers used the National Institute of Mental Health Diagnostic Interview Schedule with stratified random samples of inmates awaiting trial in the Cook County Department of Corrections and estimated rates of current (two-week) severe mental disorders to be 6.4% for male inmates ( 12 ) and 12.2% for female inmates ( 11 ).
The study reported here sought to estimate current prevalence rates of serious mental illness at two jails in Maryland and three jails in New York during two time periods. These inmates would constitute the group that meets constitutional requirements for jail mental health services and for whom aggressive discharge planning would be a priority ( 15 ). Data from a screen for mental illness were collected for all inmates who were booked into the jails during the data collection phases, and a portion of those screened were selected through systematic sampling for administration of the Structured Clinical Interview for DSM-IV (SCID). Prevalence rates were estimated through a weighting procedure whereby the data were organized into strata by gender, phase, and jail. The original purpose of gathering the data used in this study was to validate and refine a mental health screen for correctional officers to administer to jail inmates at intake ( 16 , 17 ).
Methods
From large samples of recently admitted jail inmates who were screened with the Brief Jail Mental Health Screen (BJMHS), subgroups were selected and the SCID was administered to them. Results for the subsamples were weighted back to the larger screened samples in order to estimate current prevalence rates of serious mental illness. Because the original purpose of data collection was to validate the BJMHS, systematic sampling methods were used to select individuals for the SCID subsamples in order to obtain an adequate sample of inmates who screened positive and a sufficient number of female inmates to enable a separate gender analysis.
Data collection
The BJMHS was developed as a jail intake screen to determine whether an inmate should be referred for further mental health evaluation. The BJMHS was validated during two phases of data collection. During phase I (May 2002 through January 2003) the original eight-item screen was validated at two county jails in Maryland (Montgomery County and Prince George's County) and two county jails in New York (Albany County and Rensselaer County). For phase II (November 2005 through June 2006) a revised 12-item version of the screen was tested at the same jails in Maryland and at the Rensselaer County jail, but the Monroe County jail in New York was substituted as the fourth site. During both phases, the screen was administered to inmates during intake, except for Monroe County in phase II, where screens were administered within 24 hours of intake after the initial court appearance ( 17 ).
SCID
The SCID is a semistructured clinical interview designed to assess the presence of selected DSM-IV axis I diagnoses ( 18 ). The instrument is administered by a trained clinical interviewer or mental health professional and uses a modular format with skip patterns within diagnostic sections. When criteria for a given diagnosis are met, the diagnosis is scored in terms of its lifetime prevalence and its presence in the past month. For the phase I and phase II data collections, a subset of modules were administered.
For this study, serious mental illness was defined as the presence of one or more of the following diagnoses in the past month: major depressive disorder; depressive disorder not otherwise specified; bipolar disorder I, II, and not otherwise specified; schizophrenia spectrum disorder; schizoaffective disorder; schizophreniform disorder; brief psychotic disorder; delusional disorder; and psychotic disorder not otherwise specified. There were no measures of functional impairment.
As soon as inmates were classified into those who screened positive and those who screened negative, clinical research interviewers who were blind to the inmates' sampling group status approached the inmates on their list of potential participants. Participation in both phases was voluntary. Informed consent forms approved by the institutional review board of Policy Research Associates, Inc., were required and obtained for all SCID subsample participants. Participants were informed that the decision to participate would not affect their stay in the jail, and a brief quiz was administered to assess competency to consent. All SCID interviews occurred within 72 hours of an inmate's admission to the jail but typically not within the first eight hours.
In both phases the overall refusal rate of inmates approached for the SCID interview was 31% ( 16 , 17 ). In phase I women were more likely than men (p<.05) to refuse when approached for an interview, and in phase II the refusal rate was particularly high in the Prince George's County jail—126 of 228 inmates (55%) who were approached refused to participate. The refusal rate was likely due to the fact that compensation was not offered to SCID sample participants at this jail and to the constraints imposed by the jail on scheduling and conducting interviews. However, because the results of all analyses are presented by gender and by jail and because no significant differences were found between those who refused and those who consented in Prince George's County, there are no biases on these two factors.
Interviewer training
Nine clinical research interviewers were trained for phase I, and 16 were trained for phase II. Many of the phase I interviewers also participated in phase II. During each phase, interviewers participated in a two-day on-site training in administration of the SCID by a certified SCID instructor. Interviewers practiced with acquaintances and volunteer psychiatric patients. Interrater reliability ( α =.964) was ensured by having each interviewer complete two reliability tapes, which were scored. Interviewers were also observed while conducting interviews in the jails.
Data analysis
All data management and analyses were conducted in SPSS (version 12) or Stata (release 10). Weighted prevalence estimates and confidence intervals were computed with the survey procedures in Stata (release 10).
Weighting
Persons who were screened by the BJMHS (a "population") were grouped into strata defined by study phase, jail, gender, and BJMHS result (positive or negative). Those who also were administered the SCID (the "sample") were classified into the same strata. Each person in the SCID subsample received a selection weight W=(N/n), where N was the number of population members in the person's population stratum and n was the number in the person's SCID sample stratum. If a certain number—represented by "a"—of those who also were administered the SCID are classified as having serious mental illness, then the estimated prevalence in the stratum is p=a/n and the estimated number of population members with serious mental illness in the stratum is A=(N/n)a=Np.These stratum numbers were added to form the numerators and were divided by the known population totals to get estimated prevalence rates. Confidence intervals for specific rates for jail, phase, and gender were based on the assumption that within strata individuals were selected for the SCID by systematic sampling. This was at best an approximation. The pooled gender-specific rates compute confidence intervals by treating jails as sampled clusters. The intervals were computed on the logit scale and transformed to the probability scale ( 19 ) and were asymmetric.
Screening samples
Phase I. Screening data were collected from 11,438 male and female jail inmates admitted to one of four county jails from May 2002 through January 2003. Valid data were obtained for 11,168 inmates. The percentage with positive scores on the eight-item BJMHS ranged from an overall high of 14% (N=399) in Prince George's County to an overall low of 9% (N=287) in Albany County.
Phase II. Between November 2005 and June 2006 a total of 10,562 inmates admitted to one of the four county jails were screened with the 12-item BJMHS. Valid data were obtained for 10,240 inmates. The percentage of screened inmates classified as positive on the basis of scoring for the eight-item BJMHS ranged from 24% (N=296) in Monroe County to 9% (N=880) in Montgomery County. The high positive rate in Monroe County is due to the large proportion of female inmates and the consistently higher number of positive scores for women.
SCID samples
The SCID was administered to a total of 822 inmates—358 during phase I and 464 during phase II. In both phases, women and inmates who screened positive were approached in larger numbers for an interview. Across the four jails, a total of 147 (41%) women were interviewed in phase I, and 258 (56%) women were interviewed in phase II. Of the inmates in the SCID subsample, 125 (35%) at phase I and 135 (29%) at phase II had screened positive on the basis of the eight-item BJMHS. Among both men and women, consistently higher rates of serious mental illness were observed for those who screened positive, which was expected given the predictive accuracy of the BJMHS ( 16 , 17 ).
Results
Prevalence of mental illness
Table 1 shows the results of screening at the four jails by phase and by gender as well as the SCID results for the subsamples.
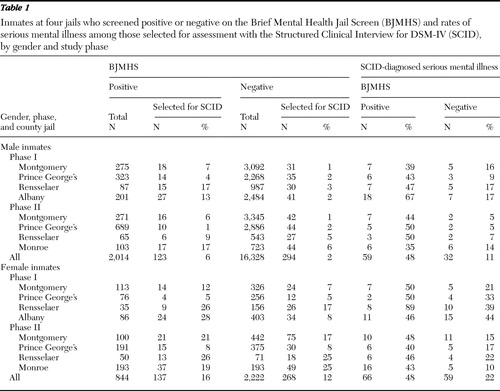 |
Table 2 presents the weighted prevalence and asymmetric 95% confidence intervals (CIs) of current serious mental illness in the jails by gender and phase. The weighted estimates adjust for oversampling in the SCID subsample of women and of inmates who screened positive and provide accurate estimates of the prevalence of serious mental illness. Data from all four jails were used for analysis in each phase. The same analysis using just the three jails that participated in both phases yielded results that were not significantly different.
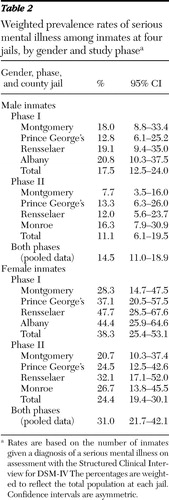 |
Male inmates. Prevalence of serious mental illness among male inmates in phase I ranged from 12.8% in Prince George's County to 20.8% in Albany County, with an overall rate of 17.5%. In phase II prevalence of serious mental illness for men ranged from 7.7% in Montgomery County to 16.3% in Monroe County, with an overall rate of 11.1%. Analysis of pooled data from the two phases yielded an estimated 14.5% prevalence rate of serious mental illness among male jail inmates. The addition of posttraumatic stress disorder (PTSD) as a serious mental illness increased the estimate to 17.1% (asymmetric CI=3.2%–21.8%).
Female inmates. Estimated rates of serious mental illness among female inmates in phase I ranged from 28.3% in Montgomery County to 47.7% in Rensselaer County, with an overall rate of 38.3%. Phase II results for women were slightly lower, with prevalence rates ranging from 20.7% in Montgomery County to 32.1% in Rensselaer County and an overall rate of 24.4%. Analysis of pooled data from the two phases yielded a prevalence rate of 31% among female jail inmates. As with the male inmates, the addition of PTSD as a serious mental illness raised the prevalence rate among female inmates only modestly to 34.3% (asymmetric CI=24.4%–45.7%).
Discussion
The final, weighted prevalence rates of current serious mental illness for recently booked jail inmates were 14.5% for men and 31.0% for women across the jails and study phases. When these estimates are applied to the 13 million annual jail admissions in 2007, assuming that the proportion of female admissions was 12.9%, there were about two million (2,161,705) annual bookings of persons with serious mental illnesses into jails. If a primary SCID diagnosis of PTSD was included as a serious mental illness, the weighted estimates increased to 17.1% for men and 34.3% for women.
The estimated prevalence rates among female inmates found in this study were double those for male inmates. This gender difference is particularly important given the rising number and proportion of female inmates in U.S. jails ( 1 ). The estimated prevalence among female inmates is higher whether or not current PTSD is included as a serious mental illness.
These prevalence estimates provide evidence for what jail staff already know to be true: the volume of inmates entering jails with serious mental illnesses is substantial. One possible explanation for the high estimates is limited access to community behavioral health services ( 20 ). We believe that rates for male and female inmates could be applied to a particular jail to yield a reasonable estimate for planning purposes. Using these estimates, jail administrators can likely anticipate that the prevalence of serious mental illness will be between 11.0% and 18.9% among men and between 21.7% and 42.1% among women, with a 14.5% average among men and a 31.0% average among women.
Several limitations of this study are noteworthy. Because no measure of functional impairment was used, it is unclear whether these individuals met federal and state definitions of serious or severe mental illness ( 21 ). In addition, the definition of serious mental illness did not include some axis I disorders that can be very severe, such as anxiety disorder. Similarly, some axis II disorders, such as borderline personality disorder, can also be severe, and none were included. On the other hand, only a small proportion of the overall SCID subsample who were deemed to have a serious mental illness received a primary diagnosis of depressive disorder not otherwise specified (four inmates, or 1.9%)
Although some variation was noted across the jails and study phases, the estimates were consistent. The reason for the variation is unclear because the same screening and diagnostic interview, and in many cases the same interviewers, were employed during both phases. We examined other factors, such as differences or changes in racial composition, as possible reasons for the differences among jails or phases, but none were found.
Conclusions
There is broad consensus that jails are not the optimal settings to provide acute psychiatric treatment. In line with the recommendations of the Criminal Justice/Mental Health Consensus Project report ( 22 ) and the President's New Freedom Commission on Mental Health ( 23 ), many communities have instituted mechanisms to divert individuals with serious mental illnesses from the front door of the jail to community-based services or have established linkages to services by way of transition planning at the back door. Since a 1992 survey estimated that only 52 jail diversion programs operated in the United States ( 24 ), there has been a rapid expansion of specialized law enforcement-based responses ( 25 ), problem-solving mental health courts ( 26 ), and specialized probation models ( 27 ) aimed at reducing the prevalence of individuals with mental illnesses in jail settings. Such expansion has been supported by an array of state and federal grant programs, including the Criminal Justice, Mental Health and Substance Abuse Reinvestment Act in Florida; the Mental Health Courts Program and the Justice and Mental Health Collaboration Program of the Bureau of Justice Assistance; and the Targeted Capacity Expansion for Jail Diversion Programs and the Jail Diversion and Trauma Recovery-Priority to Veterans initiatives of the Substance Abuse and Mental Health Services Administration. Nonetheless, the substantial presence of individuals with serious mental illnesses in our country's jails, as estimated in this study, calls for a clearer explication of the contributing factors and discussion of appropriate responses.
Acknowledgments and disclosures
This research was partly supported by a contract from the Council of State Governments. The original data were collected under grants 2001-IJ-CX-0030 and 2005-IJ-CX-0004 from the Office of Justice Programs, National Institute of Justice, U.S. Department of Justice. The points of view in this article are those of the authors and do not necessarily represent the official positions or policies of the U.S. Department of Justice.
The authors report no competing interests.
1. Sabol WJ, Minton TD: Jail Inmates at Midyear 2007. Washington, DC, Department of Justice, Office of Justice Programs, Bureau of Justice Statistics, 2008Google Scholar
2. Cohen F, Dvoskin J: Inmates with mental disorders: a guide to law and practice. Mental and Physical Disability Law Reporter 16:339–346, 1996Google Scholar
3. Estelle v Gamble, 429 US 97, 103 (1976)Google Scholar
4. Ruiz v Estelle, 503 F Supp 1256, 1323 (SD Tex, 1980)Google Scholar
5. Solomon AL, Osborne JWL, LoBuglio SF, et al: Life After Lockup: Improving Reentry From Jail to the Community. Washington, DC, Urban Institute, 2008Google Scholar
6. Lamb HR, Weinberger LE, Marsh JS, et al: Treatment prospects for persons with severe mental illness in an urban county jail. Psychiatric Services 58:782–786, 2007Google Scholar
7. Ditton PM: Mental Health and Treatment of Inmates and Probationers. Pub no NCJ 174463. Washington DC, Department of Justice, Office of Justice Programs, Bureau of Justice Assistance, 1999Google Scholar
8. James DJ, Glaze LE: Mental Health Problems of Prison and Jail Inmates. Pub no NCJ 213600. Washington, DC, Department of Justice, Office of Justice Programs, Bureau of Justice Statistics, 2006Google Scholar
9. Trestman RL, Ford J, Zhang W, et al: Current and lifetime psychiatric illness among inmates not identified as acutely mentally ill at intake in Connecticut's jails. Journal of the American Academy of Psychiatry and the Law 35:490–500, 2007Google Scholar
10. Teplin LA, Abram KM, McClelland GM: Prevalence of psychiatric disorders among incarcerated women: I. pretrial jail detainees. Archives of General Psychiatry 53:505–512, 1996Google Scholar
11. Abram KM, Teplin LA, McClelland GM: Comorbidity of severe psychiatric disorders and substance use disorders among women in jail. American Journal of Psychiatry 160:1007–1010, 2003Google Scholar
12. Teplin LA: The prevalence of severe mental disorder among urban male detainees: comparison with the Epidemiologic Catchment Area program. American Journal of Public Health 84:663–669, 1990Google Scholar
13. Teplin LA: Psychiatric and substance use disorders among male urban jail detainees. American Journal of Public Health 84:290–293, 1994Google Scholar
14. Abram KM, Teplin LA: Co-occurring disorders among mentally ill jail detainees. American Psychologist 46:1036–1045, 1991Google Scholar
15. Osher F, Steadman HJ, Barr H: A best practice approach to community reentry from jails for inmates with co-occurring disorders: the APIC model. Crime and Delinquency 49:79–96, 2003Google Scholar
16. Steadman HJ, Scott JE, Osher FC, et al: Validation of the Brief Jail Mental Health Screen. Psychiatric Services 56:816–822, 2005Google Scholar
17. Steadman HJ, Robbins PC, Islam T, et al: Revalidating the Brief Jail Mental Health Screen to increase accuracy for women. Psychiatric Services 58:1598–1601, 2007Google Scholar
18. First MB, Gibbon M, Spitzer RL, et al: User's Guide for the Structured Clinical Interview for DSM-IV-TR Axis I Disorders: SCID-I, Research Version. New York, New York State Psychiatric Institute, Biometric Research Department, 2001Google Scholar
19. Korn EL, Graubard BI: Analysis of Health Surveys. New York, Wiley, 2003Google Scholar
20. Wilper AP, Woolhandler S, Boyd JW, et al: The health and health care of US prisoners: a nationwide survey. American Journal of Public Health 99:666–672, 2009Google Scholar
21. Kessler RC, Berglund PA, Zhao S, et al: The 12-month prevalence and correlates of serious mental illness, in Mental Health United States, 1996. Edited by Manderscheid RW, Sonnenscheim MA. Washington, DC, US Government Printing Office, 1996Google Scholar
22. Council of State Governments: Criminal Justice/Mental Health Consensus Project. New York, Council of State Governments, 2002Google Scholar
23. Subcommittee on Criminal Justice: Background Paper. Rockville, Md, President's New Freedom Commission on Mental Health, 2004Google Scholar
24. Steadman HJ, Barbera S, Dennis DL: A national survey of jail diversion programs for mentally ill detainees. Hospital and Community Psychiatry 45:1109–1113, 1994Google Scholar
25. Schwarzfeld M, Reuland M, Plotkin M: Improving Responses to People With Mental Illnesses: The Essential Elements of a Specialized Law Enforcement-Based Program. New York, Council of State Governments Justice Center, 2008Google Scholar
26. Thompson M, Osher, FC, Tomasini-Joshi D: Improving Responses to People With Mental Illnesses: The Essential Elements of a Mental Health Court. New York, Council of State Governments Justice Center, 2008Google Scholar
27. Skeem JL, Louden J: Toward evidence-based practice for probationers and parolees mandated to mental health treatment. Psychiatric Services 57:333–342, 2006Google Scholar



