Substance Use, Symptom, and Employment Outcomes of Persons With a Workplace Mandate for Chemical Dependency Treatment
Treatment mandates are a major predictor of entry into chemical dependency treatment ( 1 , 2 , 3 , 4 , 5 ). In the public sector, individuals are often pressured to enter treatment by criminal justice or welfare agencies; in private programs the pressure is often from employers ( 1 , 3 ). Most research in this area has examined legal mandates, with treatment retention and rearrest as outcomes. Results are mixed, but outcomes are often similar to those of voluntary clients ( 5 , 6 , 7 , 8 , 9 , 10 , 11 , 12 ).
Employee substance use problems are a major policy issue for employers, insurers, and health plans, as they affect large numbers of workers and impose a substantial financial burden on employers. Treatment mandates originate from employee assistance programs, unions, or employers ( 3 , 4 , 13 ). Few recent studies have examined how workplace mandates affect treatment outcomes, but earlier studies found that employees who were mandated to enter treatment and those who sought treatment voluntarily had comparable outcomes ( 14 , 15 ).
Problem severity and motivation are robust factors affecting chemical dependency treatment outcome, possibly overriding effects of a mandate. Substance use and psychiatric disorders commonly co-occur among individuals in treatment ( 16 , 17 , 18 ), and these complex patients typically do less well than others ( 19 , 20 , 21 , 22 , 23 ). However, whether their outcomes are affected by workplace mandates has not been examined.
Because patients who are pressured to enter treatment typically are less motivated than those who are self-referred, and motivation to abstain from substance use is a key predictor of positive outcomes ( 24 , 25 , 26 , 27 ), policy makers and treatment programs do not expect superior outcomes for mandated patients. Rather, studies typically examine whether their outcomes are similar.
In this study we used data from a large managed care health plan to compare demographic characteristics, perceived need for treatment, and problem severity among employed patients who entered chemical dependency treatment with or without a workplace mandate. Controlling for other predictors of outcome, we examined the short- and long-term roles of mandates. Relevant outcomes for employers, patients, and families include treatment adherence, improvement in employment problems, and abstinence. Because of high rates of co-occurring mental health problems, we also examined outcomes in terms of the severity of psychiatric symptoms.
On the basis of the literature, we hypothesized that individuals with workplace mandates would show improvement at one-year follow-up and have abstinence, employment, and psychiatric outcomes similar to those without such mandates. We further examined whether outcomes were sustained over five years.
Methods
Setting and sample
Kaiser Permanente Northern California is a large, private, nonprofit, integrated managed care health plan covering 40% of the region's commercially insured population and providing chemical dependency and psychiatric services internally (that is, they are not contracted out). Most members are insured through their own employer or a family member's employer.
The original study collected data for 747 adults who were admitted to the Kaiser Permanente Sacramento Chemical Dependency Recovery Program (CDRP) between April 1997 and December 1998 and who were either randomly assigned to receive integrated primary care within the CDRP or standard primary care ( 28 ) or followed without random assignment. The analysis reported here included data for the individuals from the original sample who were employed full- or part-time at baseline and followed up at one year (N=405) and at five years (N=362). The study was observational and examined the effect on treatment outcomes of receiving a workplace mandate. Random assignment was not based on whether or not the participant had a workplace mandate. Those with a workplace mandate were equally distributed between the integrated primary care arm and the treatment-as-usual arm. In addition to Kaiser Permanente administrative data, we used data collected at intake and at one and five years.
Patients from all 846 consecutive admissions to treatment during the study period were recruited; 747 of the patients admitted (88%) agreed to be in the original study. Of that group, 654 (88%) consented to random assignment to a treatment condition. The others agreed to participate in other study protocols. Data were collected from all 747 participants at intake and from 668 (89%) at one year, and 598 (80%) at five years. Patients received random breath analysis and urine screens during treatment and at follow-ups. As noted above, the two study arms did not differ by workplace mandates. They also did not differ by age, gender, level of care, substance use severity, or psychiatric diagnosis. The only difference between those followed up at one year and those lost to follow-up was that more women than men were in the follow-up group (289 women, or 92%, compared with 379 men, or 88%, p=.048). A detailed description of the larger study has been published elsewhere ( 28 ).
Institutional review board approval was obtained from the University of California, San Francisco, and Kaiser Foundation Research Institute. All participants provided written informed consent.
Treatment programs
The CDRP offers group-based outpatient and day treatment modalities. Both include supportive group therapy, education, relapse prevention, family therapy, and individual counseling. Both last for eight weeks, with aftercare for ten months. Both conduct random drug testing. A psychiatrist is available for consultation in both programs. The Kaiser Permanente Department of Psychiatry provides individual and group psychotherapy and medication management. Participants with a workplace mandate were equally distributed between day treatment and traditional outpatient care.
Measures
Demographic characteristics documented at the intake interview included age, gender, ethnicity, education, and employment status. The intake interview also included questions about workplace mandates to enter treatment: "Did anyone tell you that if you did not get treatment you might suffer serious consequences? Serious consequences would be things like going to jail, losing your job, losing welfare benefits, losing custody of your children, or your spouse leaving you." Thus each type of mandate was asked about in the context of these serious consequences. We identified persons who were told by an employer, union, or employee assistance program that they would lose their job, and we refer to this group as having received a workplace mandate. The intake interview included also an item about perceived pressure to enter treatment. Respondents were given five choices to describe the intensity of the pressure they felt, ranging from no pressure to very strong pressure.
Data on readmission to Kaiser Permanente chemical dependency treatment were gathered from administrative databases. A new admission was defined as one that occurred after a service gap of 30 days or more. This is the definition used by the Kaiser Permanente Regional Chemical Dependency Oversight Committee and in other studies ( 29 , 30 ). Use of psychiatric services was also assessed with administrative data and defined as visits to the Kaiser Permanente Department of Psychiatry or to the CDRP psychiatrist. Administrative data were used to document treatment adherence (length of stay) at one year, which was recorded as the duration of the treatment episode in days. Possible length of stay ranged from one to 365 days. We assessed the relationship of treatment adherence with other outcomes.
Administrative data were also used to document primary and secondary ICD-9 diagnoses in the two years before intake and up to six months after intake. For the 75 participants who were employed at baseline and who had a workplace mandate, the most prevalent diagnosis was depression (N=14, 19%) followed by anxiety disorder (N=8, 11%), personality disorders (N=7, 9%), dysthymia (N=5, 7%), adjustment disorder (N=5, 7%), bipolar disorder (N=4, 5%), posttraumatic stress disorder (N=4, 5%), attention-deficit hyperactivity disorder (N=4, 5%), and eating disorders (N=1, 1%). Dysthymia differed by presence or absence of a workplace mandate; five (7%) of those with a workplace mandate had a diagnosis of dysthymia, compared with 71 (19%) of those without a workplace mandate (p<.009). Depression also differed by workplace mandate; 14 (19%) of those with a mandate had a diagnosis of depression, compared with 133 (36%) of those without a mandate (p=.004).
Participants responded to a checklist of questions based on criteria from the Diagnostic Interview Schedule for Psychoactive Substance Dependence, DSM-IV that has been used in other published studies ( 16 , 24 , 28 , 30 ). The presence or absence of each symptom was noted for the previous 30 days, and individuals with three or more symptoms out of a total of seven were classified as dependent. Rates of cocaine, stimulant, marijuana, heroin, tranquilizer, inhalant, hallucinogen, methamphetamine, or polysubstance dependence did not differ by presence or absence of a workplace mandate ( 28 ). Those with a workplace mandate had significantly lower rates of alcohol dependence, marginally lower rates of narcotic-analgesic dependence, and marginally higher rates of barbiturate dependence (data not shown).
At baseline and follow-up interviews, composite scores from the Addiction Severity Index (ASI) reflected the severity of problems in seven areas: alcohol, drug, psychiatric, legal, medical, employment, and family and social relations. The ASI is a valid and reliable instrument that examines these seven areas, and it is one of the most commonly used instruments in alcohol and drug treatment research ( 31 , 32 , 33 ). Questions measure the number, frequency, and duration of problems in each domain in the past 30 days, providing a continuous measure from 0 (no problems) to 1.0 (high severity).
Perceived need for treatment was assessed with an ASI item that is strongly related to motivation, readiness for treatment, and stage of change ( 25 ): "How important to you is treatment for your [alcohol, drug, employment, family, legal, medical, psychiatric] problem?" Response categories are extremely, considerably, moderately, somewhat, and none. Responses were dichotomized into extremely or considerably versus the other categories.
Because of the skewed distribution of ASI scores for psychiatric severity, psychiatric outcomes at one and five years were measured as above or below the ASI median of all individuals in the sample at each interview (scores below the median indicated lower severity).
At the baseline and follow-up interviews, participants were asked about use in the past 30 days and in the past year of any alcohol, marijuana, barbiturates, sedatives, cocaine, crack, stimulants, tranquilizers, heroin, hallucinogens, opiates, painkillers, and inhalants (for the medications listed, only nonprescribed use was included in this analysis). A negative answer to use of all substances was defined as abstinence, which was validated by breath analysis and urinalysis. There was a high level of agreement between these validation measures and self-report; 6% reported no substance use but screened positive ( 28 ). Abstinence from alcohol and drugs for 30 days before the one- and five-year interviews was the primary substance use outcome.
Data analysis
As noted above, participants with a workplace mandate were equally distributed between integrated primary care and treatment as usual, as well as between outpatient and day treatment modalities. However, in post hoc regression models, neither treatment arm nor modality type were significant predictors of any of the outcomes measures, and these variables were omitted from the analyses.
Differences at baseline among the 448 participants who were employed full- or part-time at intake were examined, as were differences among the 405 participants from this group (91%) who had a one-year follow-up and among the 362 (81%) who had a five-year follow-up. Chi square tests assessed differences in proportions, and t tests compared means. Logistic regression analysis models were used to examine predictors of abstinence (dichotomous measure) at one and five years and of an ASI psychiatric severity score below the median. Because of its skewed distribution, the ASI psychiatric score was dichotomized at the median using the baseline scores. Linear regression models examined predictors of the continuous measures—length of stay and ASI employment problem score.
To account for differences attributable to self-selection, we calculated propensity scores for the likelihood of receiving a workplace mandate. We used logistic regression to examine characteristics potentially related to the receipt of a mandate. Independent variables were gender, age, marital status, ethnicity, education, income, occupation, chemical dependence and psychiatric treatment histories, type of substance dependence, and all ASI scores. We calculated the probability of receiving a mandate by using a fitted logistic regression model with these potential confounders as the independent variables. Propensity scores ranged from 0 to 1 and reflected the conditional probability of receiving a mandate given baseline characteristics, with 1 indicating highest probability. Using the quintiles of the distribution, we divided the scores into five categories and included this variable in the regression models. When the propensity score was not statistically significant, we refit the model, excluding the score. The propensity scores were not significant predictors of outcomes in any of the models; thus the results are shown without them.
All measures for which baseline differences were found between participants with and without a workplace mandate were controlled in the propensity score. In addition, the variables with significant baseline differences (alcohol and drug problem severity; psychiatric diagnosis; and motivation for treatment for alcohol, drug, psychiatric, or employment problems) were controlled for in the analysis.
In addition to assessing length of stay as an outcome, we assessed its relationship with workplace mandates and each outcome. The regression models first excluded length of stay and were then refit to include it ( 34 ). We examined Akaike information criteria (AIC) and R 2 statistics. The AIC finds the best-fitting and most parsimonious model by using the log likelihood as the fit variable. We compared two models of the same outcome using AIC; the model with the larger value was the better and more parsimonious.
Results
Table 1 presents characteristics of the 448 employed participants in the baseline sample, 75 (17%) of whom had workplace mandates. Compared with the group without mandates, the group with mandates had a significantly larger proportion of men and of African Americans, a smaller proportion of Hispanics and of individuals with a psychiatric diagnosis, and a lower level of education. ASI scores for the group with mandates were higher for employment problem severity, although the difference was not significant (p=.075), and lower for family, psychiatric, alcohol, and drug problem severity.
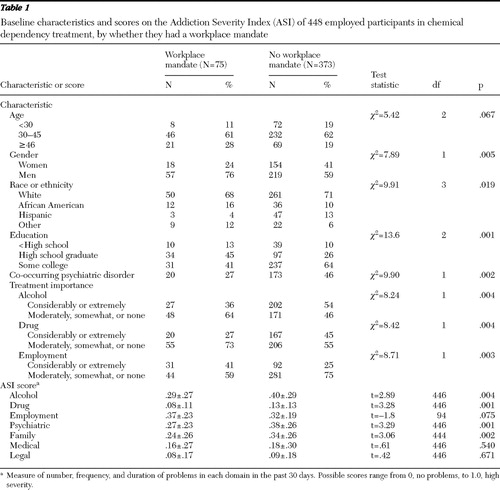 |
Compared with participants without a workplace mandate, a smaller proportion of those with a workplace mandate considered treatment for alcohol or drug problems to be considerably or extremely important, but a larger proportion considered chemical dependency treatment to address employment problems to be considerably or extremely important.
Among the 75 participants with a workplace mandate, 40 (53%) had no other mandate, 18 (24%) had one other, and 17 (23%) had at least two others. Among those with a workplace mandate who had additional mandates, 32 (43% of all those with workplace mandates) had a mandate from their family, 12 (16%) from a mental health provider, nine (12%) from a health provider, and seven (9%) from a legal source (data not shown). Among the 373 participants without workplace mandates, 267 (72%) had no mandate, 93 (25%) had one, and 13 (3%) had two or more. Of these, 94 (25%) received a mandate from family, nine (2%) from a mental health provider, eight (2%) from a health provider, and ten (3%) from a legal source.
Bivariate analyses examined the relationship between feeling pressure to enter treatment and other variables. A response of "very strong" to the question "How much pressure did you feel to enter treatment?" was positively related to having a workplace mandate. Specifically, at one-year follow-up, 38 of the 70 participants with a workplace mandate (54%) gave this response, compared with 48 of the 335 without a mandate (14%) (p<.001). This response was also related to abstinence at one year; 61 of the 252 participants who were abstinent at one year (24%) gave this response, compared with 25 of the 152 who were not abstinent (16%), but the difference was not significant (p=.065). In addition, feeling very strong pressure to enter treatment was related to perceived need for treatment to address employment problems; 37 of the 106 participants who perceived a need for treatment in this area (35%) gave this response, compared with 49 of the 299 participants who did not perceive such a need (16%) (p<.001). Feeling very strong pressure was not significantly related to the severity of alcohol, drug, psychiatric, or employment problems at one year (data not shown).
Having a workplace mandate was related to length of stay in chemical dependency treatment. At one year, the group with a workplace mandate had longer stays than those without a workplace mandate (mean±SD of 124±129 and 72±97 days; t=-3.29, df=91, p=.001). Among those with a workplace mandate, length of stay was not significantly different between those with no additional mandates and those with additional mandates (data not shown).
Changes in ASI scores from baseline to the two follow-ups in the groups with and without a workplace mandate are shown in Table 2 . Scores at one year indicated significant improvements in both groups. However, for participants with a workplace mandate, improvements were not significant in the severity of legal problems and medical problems. At five years, similar patterns persisted; however, those with a workplace mandate showed significant improvement in employment problems, and those without a mandate showed marginal improvement (p=.058) in this area. Medical severity was not significant at five years.
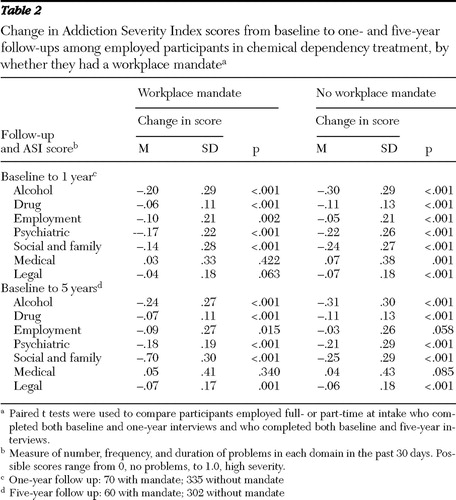 |
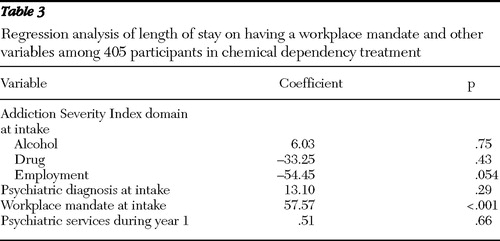
Table 3 presents an ordinary least-squares regression model of predictors of length of stay in chemical dependency treatment. Having a workplace mandate was related to a longer stay (p<.001), and greater severity of employment problems at intake was marginally related to a shorter stay (p=.054). Severity of alcohol and drug problems and psychiatric diagnosis were not significant predictors of length of stay.
 |
Logistic regression models of predictors at one year of abstinence from alcohol and drugs and severity of psychiatric problems, as well as linear regression models of severity of employment problems, are shown in Table 4 . To examine the role of length of stay, the regression models first excluded length of stay and were then refit to include it. In the model that excluded length of stay, having a workplace mandate predicted abstinence (odds ratio [OR]=1.86). When length of stay was included, having a workplace mandate was no longer significant; however, in this model a longer stay predicted abstinence (OR=1.01). The change in AIC was statistically significant. In both models, perceived need for alcohol treatment and receipt of psychiatric services predicted abstinence. We replicated the analysis, substituting abstinence at six months for length of stay (data not shown). Six-month abstinence was a significant predictor of abstinence at one year (OR=3.22, 95% confidence interval [CI]=13.53–46.78); however, having a workplace mandate was not a significant predictor of abstinence in this model, which is similar to the model in which length of stay was used. In post hoc analysis, a measure of having other types of mandates was added; however, receipt of other mandates was not a significant predictor of abstinence, and addition of the other mandates did not change the significance of having a workplace mandate.
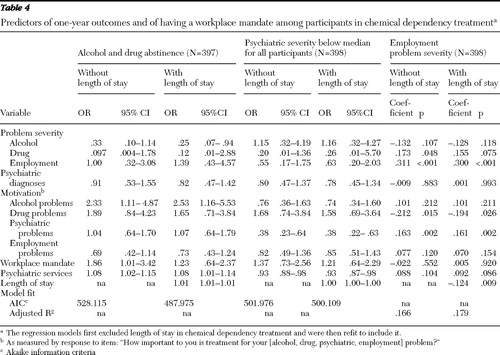 |
Predictors of severity of psychiatric problems at one year (ASI scores below the median at one year) were also examined ( Table 4 ). Having a workplace mandate was not related to lower psychiatric severity in either length-of-stay model. In both models, perceived need for psychiatric treatment and receipt of psychiatric services was related to higher psychiatric severity scores. Having a psychiatric diagnosis was not significant in either model. Length of stay was a marginally significant predictor of severity of psychiatric problems. The model fit did not change when length of stay was added. We replicated the analysis while including the baseline measure of psychiatric problem severity and found that higher baseline scores were related to higher psychiatric severity at one year (OR=.09, CI=.02–.33, in the model with length of stay) (not shown).
Predictors of severity of employment problems at one year were also examined ( Table 4 ). Having a workplace mandate was not significant in either length-of-stay model. A longer stay was related to lower employment problem severity. Perceived need for chemical dependency treatment to address employment problems was not related to lower scores on severity of employment problems in either model. However, in both models, perceived need for treatment for drug problems was related to lower employment problem severity, and perceived need for treatment for psychiatric problems was related to higher employment problem severity. Higher baseline severity of employment problems was related to higher severity of employment problems at one year. The model fit improved when length of stay was included.
We used logistic and linear regression models to examine the same outcomes at five years, and we also measured treatment readmission and receipt of psychiatric services between one and five years (not shown). All results were consistent with the one-year results, including the significance of length of stay for abstinence (OR=1.004, CI=1.002–1.006). However, having a workplace mandate did not predict abstinence at five years. Baseline and one-year severity scores in all problem areas predicted the same outcomes in the same direction at five years. Perceived need for alcohol treatment remained important in predicting abstinence (OR=3.01, CI=1.36–6.64), and perceived need for psychiatric treatment remained important in predicting psychiatric severity (OR=.59, CI=.35–.997). None of the motivation measures predicted severity of employment problems at five years. Receipt of psychiatric services was positively related to abstinence, even when length of stay was included in the model (OR=.96, CI=.92–.999). Readmission to chemical dependency treatment predicted abstinence at five years (OR=1.83, CI=1.15–2.90 in the model without length of stay; OR=1.91, CI=1.19–3.05 in the model with length of stay) but not severity of psychiatric or employment problems.
Discussion
We examined outcomes of length of stay, abstinence, and severity of psychiatric and employment problems in relation to having a workplace mandate to enter chemical dependency treatment. Individuals with a workplace mandate showed significant improvements in all problem domains except medical and legal problems, whereas those without a workplace mandate improved in all seven domains (alcohol, drug, employment, psychiatric, family, medical, and legal domains). When analyses controlled for other outcome predictors, individuals with a workplace mandate had outcomes similar to those without a mandate. An important exception was that when length of stay in chemical dependency treatment was excluded from the model, having a workplace mandate predicted abstinence at one year. At five years the results of the bivariate analyses were similar, except that persons with a workplace mandate showed sustained improvement in the severity of employment problems, whereas others did not.
As expected, longer treatment stays, which are a consequence of workplace mandates, predicted better outcomes. Consistent with other research ( 35 , 36 , 37 ), length of stay was a critical predictor of all outcomes and remained so at five years. Treatment adherence (such as medication adherence) is a primary outcome examined in the psychiatric literature, and studies have examined the role of feared loss of housing, financial leverage, and threatened hospitalization in improving adherence ( 38 , 39 , 40 ). Adherence is also an important outcome in chemical dependency treatment. The first test of whether individuals are adhering to treatment is whether they continue to attend treatment programs. Most programs include drug testing and impose sanctions for positive tests.
Participants with a workplace mandate perceived alcohol and drug treatment as less important compared with participants without a workplace mandate, and they perceived alcohol and drug treatment to address employment problems as more important. They also reported feeling stronger pressure to enter treatment. Similarly, post hoc analysis found that very strong pressure to enter treatment was related to high perceived need for treatment to address employment problems but not for alcohol or drug problems. Research has shown that motivation for treatment for substance use problems is related to better treatment outcomes. We broadened the measure to examine motivation for treatment for various problem areas and found that type of motivation made a difference. Thus, although participants with a workplace mandate gave lower ratings than those without a mandate to the importance of treatment for alcohol and drug problems, the mandated participants had similar or better outcomes in terms of abstinence. However, rating treatment to address employment problems as important did not predict improvement in employment problems or in any of the other outcomes studied. Our finding that independent of having a workplace mandate, those who had a high perceived need for treatment for alcohol or drug problems had better employment outcomes suggests that being motivated to address substance use problems is fundamental to improvement in problems related to substance use and in substance use itself.
Another key finding is that receipt of psychiatric services was related to positive substance use outcomes, although it was also related to poorer psychiatric outcomes. This finding is similar to those of other studies ( 16 , 41 ) and is probably attributable to the fact that patients with more severe psychiatric symptoms receive more services. The findings of this study underscore the prominence of co-occurring problems in populations with chemical dependence, including employed persons, and the importance of addressing these problems.
The study has several limitations. Data were not available on intensity of the workplace mandate or on what sanctions persisted after treatment completion, which may have influenced results. Randomized assignment to receipt of a workplace mandate is not feasible. However, we used propensity scores to address differences between those with and without a workplace mandate.
Conclusions
We examined a wider range of outcome measures than other studies of workplace mandates, and we used both short- and long-term follow-ups. We also looked at perceived need for treatment for problems in addition to alcohol and drug problems. Whereas other studies of treatment mandates have looked at samples of public populations and studied legal mandates, in this study the sample consisted of enrollees in a private managed care plan and workplace mandates were examined. How far can we go in interpreting results? Participants with a workplace mandate stayed in treatment longer, had better abstinence outcomes, and did as well on other outcomes as those without a workplace mandate. Again, we cannot determine whether they would have done as well if they had not been pressured to enter and remain in treatment. However, given that their perceived need for treatment for substance use problems was low, it is likely that they would not have entered treatment without pressure ( 2 , 42 ). In addition, although participants with a workplace mandate had many characteristics not related in the literature to positive treatment outcomes, they did at least as well as others. Employers should be encouraged by the significant decrease in the severity of employment problems at one and five years. Indeed, compared with employees without a workplace mandate, employees who had such a mandate appeared more likely to sustain significant improvement over five years.
Finally, how chemical dependency treatment should address this population is an important clinical issue. Traditional treatment ideology in the United States has posited that individuals cannot be helped unless they are "ready." In recent years programs have begun using interventions to increase treatment motivation ( 4 ). We know little about how workplace mandates work—whether they cause individuals to "hit bottom," provide them an opportunity to save their job, or keep them in treatment long enough for other therapeutic processes to take over. This is an important area for further research. The effect of length of stay suggests that continuing care models of treatment may have important benefits for these patients.
Acknowledgments and disclosures
The study was funded by grant R37-DA10572 from the National Institute on Drug Abuse, by grant R01-AA15183 from the National Institute on Alcohol Abuse and Alcoholism, and by the John D. and Catherine T. MacArthur Foundation Research Network on Mandated Community Treatment.
The authors report no competing interests.
1. Weisner C, Matzger H, Tam T, et al: Who goes to alcohol and drug treatment? Understanding utilization within the context of insurance. Journal of Studies on Alcohol 63:673–682, 2002Google Scholar
2. Weisner C: Coercion in alcohol treatment, in Broadening the Base of Treatment for Alcohol Problems. Washington, DC, National Academy Press, 1990Google Scholar
3. Weisner C, Schmidt LA: Rethinking access to alcohol treatment. Recent Developments in Alcoholism 15:107–136, 2001Google Scholar
4. Institute of Medicine: Improving the Quality of Health Care for Mental and Substance-Use Conditions. Washington, DC, National Academies Press, 2005Google Scholar
5. Klag S, O'Callaghan F, Creed P: The use of legal coercion in the treatment of substance abusers: an overview and critical analysis of thirty years of research. Substance Use and Misuse 40:1777–1795, 2005Google Scholar
6. Hiller ML, Knight K, Broome KM, et al: Legal pressure and treatment retention in a national sample of long-term residential programs. Criminal Justice and Behavior 25:463–481, 1998Google Scholar
7. Rempel M, DeStafano CD: Predictors of engagement in court-mandated treatment: findings at the Brooklyn Treatment Court, 1996–2000. Journal of Offender Rehabilitation 33:87–124, 2001Google Scholar
8. Brecht ML, Anglin MD, Wang JC: Treatment effectiveness for legally coerced versus voluntary methadone maintenance clients. American Journal of Drug and Alcohol Abuse 19:89–106, 1993Google Scholar
9. Prendergast ML, Farabee D, Cartier J, et al: Involuntary treatment within a prison setting: impact on psychosocial change during treatment. Criminal Justice and Behavior 29:5–26, 2002Google Scholar
10. Collins JJ, Allison M: Legal coercion and retention in drug abuse treatment. Hospital and Community Psychiatry 34:1145–1149, 1983Google Scholar
11. Farabee D, Prendergast M, Anglin MD: The effectiveness of coerced treatment for drug-abusing offenders. Federal Probation 62:3–10, 1998Google Scholar
12. Sowers WE, Daley DC: Compulsory treatment of substance use disorders. Criminal Behaviour and Mental Health 3:403–415, 1993Google Scholar
13. Masi D, Altman L, Benayon C, et al: Employee assistance programs in the year 2002, in Mental Health, United States, 2002. Edited by Manderscheid RW, Henderson MJ. Rockville, Md, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services, 2006Google Scholar
14. Lawental E, McLellan AT, Grissom GR, et al: Coerced treatment for substance abuse problems detected through workplace urine surveillance: is it effective? Journal of Substance Abuse 8:115–128, 1996Google Scholar
15. Chopra KS, Preston DA, Gerson LW: The effect of constructive coercion on the rehabilitative process: a study of the employed alcoholics in an alcoholism treatment program. Journal of Occupational Medicine 21:749–752, 1979Google Scholar
16. Chi FW, Satre DD, Weisner C: Chemical dependency patients with cooccurring psychiatric diagnoses: service patterns and 1-year outcomes. Alcoholism: Clinical and Experimental Research 30:851–859, 2006Google Scholar
17. Kessler RC, Berglund P, Demler O, et al: Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry 62:593–602, 2005Google Scholar
18. Compton WM III, Cottler LB, Phelps DL, et al: Psychiatric disorders among drug dependent subjects: are they primary or secondary? American Journal on Addictions 9:126–134, 2000Google Scholar
19. Feinman JA, Dunner DL: The effect of alcohol and substance abuse on the course of bipolar affective disorder. Journal of Affective Disorders 37:43–49, 1996Google Scholar
20. Nunes EV, Levin FR: Treatment of depression in patients with alcohol or other drug dependence: a meta-analysis. JAMA 291: 1887–1896, 2004Google Scholar
21. Swartz MS, Wagner HR, Swanson JW, et al: Substance use and psychosocial functioning in schizophrenia among new enrollees in the NIMH CATIE study. Psychiatric Services 57:1110–1116, 2006Google Scholar
22. Swartz MS, Swanson JW, Hiday VA, et al: Violence and severe mental illness: the effects of substance abuse and nonadherence to medication. American Journal of Psychiatry 155:226–231, 1998Google Scholar
23. Swartz MS, Swanson JW: Involuntary outpatient commitment, community treatment orders, and assisted outpatient treatment: what's in the data? Canadian Journal of Psychiatry 49:585–591, 2004Google Scholar
24. Satre DD, Mertens J, Arean PA, et al: Contrasting outcomes of older versus middle-aged and younger adult chemical dependency patients in a managed care program. Journal of Studies on Alcohol 64:520–530, 2003Google Scholar
25. Shen Q, McLellan AT, Merrill JC: Client's perceived need for treatment and its impact on outcome. Substance Abuse 21:179–192, 2000Google Scholar
26. Miller WR: Motivation for treatment: a review with special emphasis on alcoholism. Psychological Bulletin 89:84–107, 1985Google Scholar
27. Moos RH: Depressed outpatients' life contexts, amount of treatment, and treatment outcome. Journal of Nervous and Mental Disease 178:105–112, 1990Google Scholar
28. Weisner C, Mertens J, Parthasarathy S, et al: Integrating primary medical care with addiction treatment: a randomized controlled trial. JAMA 286:1715–1723, 2001Google Scholar
29. Campbell CI, Weisner C, Sterling S: Adolescents entering chemical dependency treatment in private managed care: ethnic differences in treatment initiation and retention. Journal of Adolescent Health 38:343–350, 2006Google Scholar
30. Mertens JR, Weisner C, Ray GT: Readmission among chemical dependency patients in private, outpatient treatment: patterns, correlates and role in long-term outcome. Journal of Studies on Alcohol 66:842–847, 2005Google Scholar
31. McLellan AT, Kushner H, Metzger D, et al: The fifth edition of the Addiction Severity Index. Journal of Substance Abuse Treatment 9:199–213, 1992Google Scholar
32. Weisner C, McLellan AT, Hunkeler EM: Addiction Severity Index data from general membership and treatment samples of HMO members: one case of norming the ASI. Journal of Substance Abuse Treatment 19:103–109, 2000Google Scholar
33. McLellan AT, Luborsky L, Cacciola J, et al: New data from the Addiction Severity Index: reliability and validity in three centers. Journal of Nervous and Mental Disease 173:412–423, 1985Google Scholar
34. Judd CM, Kenny DA: Process analysis: estimating mediation in treatment evaluations. Evaluation Review 5:602–619, 1981Google Scholar
35. Leukefeld CG, Tims FM: Compulsory treatment: a review of findings. NIDA Research Monograph 86:236–251, 1988Google Scholar
36. Ray GT, Weisner CM, Mertens JR: Relationship between use of psychiatric services and five-year alcohol and drug treatment outcomes. Psychiatric Services 56:164–171, 2005Google Scholar
37. Weisner C, Ray GT, Mertens J, et al: Short-term alcohol and drug treatment outcomes predict long-term outcome. Drug and Alcohol Dependence 71:281–294, 2003Google Scholar
38. Appelbaum PS, Redlich A: Use of leverage over patients' money to promote adherence to psychiatric treatment. Journal of Nervous and Mental Disease 194:294–302, 2006Google Scholar
39. Elbogen EB, Swanson JW, Appelbaum PS, et al: Competence to complete psychiatric advance directives: effects of facilitated decision making. Law and Human Behavior 31:275–289, 2007Google Scholar
40. Robbins PC, Petrila J, LeMelle S, et al: The use of housing as leverage to increase adherence to psychiatric treatment in the community. Administration and Policy in Mental Health 33:226–236, 2006Google Scholar
41. Hser YI, Anglin MD, Grella C, et al: Drug treatment careers: a conceptual framework and existing research findings. Journal of Substance Abuse Treatment 14:543–558, 1997Google Scholar
42. Carroll JS: Consent to mental health treatment: a theoretical analysis of coercion, freedom, and control. Behavioral Sciences and the Law 9:129–142, 1991Google Scholar



