Service Utilization Patterns of Maltreated and Nonmaltreated Children From Low-Income, African-American Families
The U.S. Surgeon General identified the reduction of child maltreatment rates as an issue of foremost public health importance ( 1 ). In 2006 nearly one million children were victims of maltreatment ( 2 ). Maltreatment has adverse effects on youths' psychological, emotional, and behavioral well-being; can lead to physical injury and death ( 2 ); and may result in increased financial expenditures for child welfare benefits ( 3 ), increased hospital visits or hospitalizations ( 4 ), and long-term mental health effects and subsequent treatment that can persist into adulthood ( 5 ).
Limitations of extant research examining service utilization and child maltreatment include a focus on child welfare system samples, assessment of only mental and behavioral health services, minimal attention to youths exposed to other forms of violence (including intimate partner violence), and limited research with African-American populations ( 3 , 6 ). It is likely that not all child maltreatment survivors are involved with the child welfare system, and they may continue to be exposed to violence and victimization. Increased knowledge of health care utilization patterns among these maltreated children is important. In addition, children may present to various health care and social service entities (psychiatric and crisis services, for example) beyond the traditional mental health systems. Youths exposed to intimate partner violence may use medical care services (emergency departments or primary care) and mental health services more than youths not exposed to intimate partner violence ( 7 ). Furthermore, research examining patterns of child maltreatment and service utilization rates by race and ethnicity have indicated that youths who are from minority groups are among those most vulnerable to lower rates of health care service utilization, particularly mental health care services ( 8 ).
This brief report presents the results of a study that investigated health care and social service utilization rates among African-American youths. The study aimed to determine whether there are differences in service utilization rates between maltreated and nonmaltreated youths. We hypothesized that health care and social service utilization rates would be significantly higher among maltreated youths.
Methods
Participants were 153 African-American children (ages eight to 12) of women recruited from two emergency care centers and two urgent care clinics of a large, university-affiliated, public hospital for the project Supporting African-American Families, Empowering Their Youth (SAFETY) ( 9 , 10 ) between March 2002 and July 2005. The hospital serves a predominantly African-American, low-income, inner-city population. Women were eligible to participate in the study if they were a caregiver for at least one eight- to 12-year-old child and if they reported either no lifetime intimate partner violence or intimate partner violence in the past year. Once written informed consent was obtained from mothers and verbal assent was obtained from the youths, each participant was interviewed separately, in person, by a trained interviewer. Exclusion criteria included medical instability, cognitive impairment, or psychotic symptoms.
The Childhood Trauma Questionnaire (CTQ) is a 28-item measure that assesses childhood experiences of abuse (emotional, physical, and sexual) ( 11 , 12 ). Items are rated on a 5-point scale; scores range from 5 to 25 for each type of child maltreatment, with higher scores indicating greater incidence of child abuse. The CTQ has adequate internal consistency (Cronbach's α =.60–.89 for subscales with African-American samples) and test-retest reliability and has convergent validity ( 11 , 12 ). Within the sample, internal consistency for the CTQ subscales ranged from .61 to .73. For the sample the perpetrator of child maltreatment was unknown. The categories of maltreatment were dichotomized with established cutoff points for each CTQ scale ( 12 ).
Youth service utilization patterns were measured with a modified version of the Adult Service Utilization Form developed and piloted for the SAFETY project, the Youth Service Utilization Form. Youth service utilization was based on child self-report and categorized into five areas: psychiatric services (such as hospitalization, day treatment, and medications), medical services (including emergency department and clinic appointments), child care services (including after-school programs), social support services (including community-based youth groups, church groups, and parks and recreation programs), and crisis services (such as a homeless shelter and hotline). Frequency of utilization was rated with four response options (never, once, twice, and three times or more).
Results
Female caregivers' mean±SD age was 32.3±6.9 years. Of the mothers, 122 (80%) had a 12th-grade education or less and 98 (64%) were unemployed. Children's mean age was 10.0±1.4, and 69 (45%) children were boys. For children for whom there was suspicion of abuse or neglect, a referral was made to child protective services. Forty-four percent (N=68) of the mothers reported intimate partner violence within the past year.
Overall reported rates of maltreatment in the sample were as follows: 17% of youths reported emotional abuse, 17% reported physical abuse, and 5% reported sexual abuse. Youth-reported rates of service utilization were as follows: 27 (18%) utilized psychiatric services, 64 (42%) used medical services, 74 (48%) utilized child care resources, 47 (31%) accessed social support services, and 13 (9%) utilized crisis services.
Frequencies were calculated for each utilization category, and utilization rates by maltreatment group were compared with the chi square test ( Table 1 ). Bivariate analyses revealed statistically significant differences in psychiatric and child care service utilization between maltreated and nonmaltreated youths across all three maltreatment categories. The frequency of use of psychiatric services (p<.01) and child care services (p=.03) by emotionally abused youths was significantly greater compared with use by their nonemotionally abused counterparts. Among physically abused children and adolescents, rates of psychiatric service use (p<.01) and child care service use (p=.03) also were higher than among children and adolescents who were not physically abused. Sexually abused children also had higher frequencies of psychiatric service use (p=.03) and child care service use (p= .03) than youths who were not sexually abused. Among emotionally abused youths, frequency of medical service use (p=.03) was higher than it was among their nonemotionally abused counterparts.
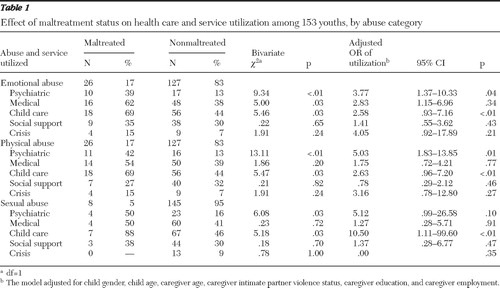 |
To assess the independent effect of maltreatment on utilization, individual multivariate logistic regression models were constructed for each utilization category, with controls for child demographic (gender and age) and caregiver factors (age, intimate partner violence status, education, and employment) ( Table 1 ). After controlling for child and caregiver factors, the regression analyses showed significant differences by maltreatment status in psychiatric service utilization among youths reporting emotional abuse (adjusted odds ratio [AOR]=3.77) and physical abuse (AOR=5.03). In both of these categories, maltreated youths were more likely than nonmaltreated youths to use psychiatric services. A similar trend occurred for youths who had been sexually abused, although the difference was not statistically significant. Maltreated youths also were more likely to use child care services. Emotionally abused (AOR=2.58) and physically abused (AOR=2.63) youths were almost three times more likely than their nonmaltreated counterparts to use child care services, whereas sexually abused youths (AOR=10.50) were approximately ten times more likely to use child care services than non-sexually abused youths.
Discussion and conclusions
With reported estimates of child maltreatment approaching one million ( 2 ) and accumulating evidence of its adverse effects on physical and mental health, child maltreatment is an issue of great concern. Among substantiated cases of child maltreatment in the United States, nearly 7% of youths experience emotional abuse, 16% report physical abuse, and almost 9% report sexual abuse ( 2 ). Rates within our sample approximated these national data.
In this study, we examined rates of health care and social service utilization among African-American youths who were not known to be involved in the welfare system and assessed utilization rates across multiple domains of services (psychiatric, medical, child care, social support, and crisis). Results indicated that utilization rates of psychiatric and child care services were greater for victims of emotional, physical, and sexual abuse, even after we controlled for child and caregiver demographic variables and maternal intimate partner violence status. In addition, rates of medical service utilization were found to be higher for emotionally abused youths than for youths who were not emotionally abused.
With regard to psychiatric services, maltreated youths across all categories of maltreatment (that is, emotional, physical, and sexual abuse) were between six and 13 times more likely to utilize psychiatric services, including hospitalization and counseling, and child care services. These findings differ from those of a previous study by Thompson ( 13 ) in which no increased likelihood of mental health service use was found on the basis of maltreatment status. However, the contradictory outcomes may be attributable to differences in the study populations. Although Thompson's study included participants with low incomes, the youths in the sample were younger (ages two to seven) and more racially heterogeneous (African American, Caucasian, Hispanic, or mixed race-ethnicity), and a majority (60%) were recruited from families reported to child protective systems. These differences may suggest that psychiatric service utilization may be affected by demographic characteristics such as age and race, as well as involvement in the child welfare system ( 14 ). For example, younger children may be less likely to receive mental health treatment, and receipt of services increases as children age ( 13 ).
Across all categories of maltreatment, maltreated children were approximately five times more likely than their nonmaltreated counterparts to use child care services, such as after-school programs. Caregivers may view child care services as an avenue for acquiring protection from the maltreated child's perpetrator and for offering a secure and stable environment. In addition, because they are mandated reporters of abuse, child care workers may be viewed by caregivers as gatekeepers to obtaining additional resources. Medical service utilization was found to be higher for maltreated than for nonmaltreated youths only in the emotional abuse category. Childhood trauma has been linked with sensitization of the stress response and immune activation ( 15 ). Maltreated children may be more prone to chronic stress, and resulting alteration to their immune system may put them at risk for acute and chronic health problems, resulting in increased medical service needs.
Results of this study offer support to the notion that a significant number of youths who are not yet involved in the child welfare system have been exposed to maltreatment. Comparing the health care service utilization practices of these youths with those of their nonmaltreated counterparts may facilitate policy-level changes to improve screening and subsequent treatment for maltreated youths. This study broadens our knowledge of the array of services potentially used by maltreated youths and offers additional domains that can serve as points of access for providers to identify and intervene with these youths.
The findings obtained must be considered in light of study limitations. First, the assessment of service utilization was based on child report, which could have resulted in inaccurate or biased reporting or in underreporting. Second, the sample was too small to separate child maltreatment group by whether the mother had experienced intimate partner violence, and therefore the severity of exposure to such violence and its impact on child maltreatment service utilization is unknown. Third, we did not assess for child's health insurance status, which has been shown to differentially affect mental health care utilization. Specifically, children with private or public insurance use mental health services at a greater rate than uninsured youths ( 8 ). Furthermore, generalizability is limited because of the relative homogeneity of this sample with regard to race and socioeconomic status.
In light of these limitations, future studies could benefit from more objective measures of service utilization by including data from other direct sources, such as the youths' parents, child care providers, hospitals, clinics, and social support agencies. Furthermore, these studies could be conducted with more diverse, larger samples, including youths within and outside of the child welfare system, and analyses that account for the mother's intimate partner violence status to further delineate its impact on children's health care service utilization.
Acknowledgments and disclosures
The data reported here were drawn from a study funded by grant R49/CCR419767-0 from the National Center for Injury Prevention and Control, Centers for Disease Control and Prevention, awarded to Dr. Kaslow.
The authors report no competing interests.
1. Healthy People 2010: Understanding and Improving Health and Objectives for Improving Health. Washington, DC, US Department of Health and Human Services, 2000Google Scholar
2. Child Maltreatment 2006. Washington, DC, US Department of Health and Human Services, 2008Google Scholar
3. Harman JS, Childs GE, Kelleher KJ: Mental health care utilization and expenditures by children in foster care. Archives of Pediatrics and Adolescent Medicine 154:1114–1117, 2000Google Scholar
4. Wang C-T, Holton J: Total Estimated Cost of Child Abuse and Neglect in the United States. Chicago, Prevent Child Abuse America, 2007Google Scholar
5. Kaplow JB, Widom CS: Age of onset of child maltreatment predicts long-term mental health outcomes. Journal of Abnormal Psychology 116:176–187, 2007Google Scholar
6. Becker M, Jordan N, Larsen R: Behavioral health service use and costs among children in foster care. Child Welfare 85:633–647, 2006Google Scholar
7. Rivara FP, Anderson ML, Fishman P, et al: Intimate partner violence and health care costs and utilization for children living in the home. Pediatrics 120:1270–1277, 2007Google Scholar
8. Kataoka SH, Zhang L, Wells KB: Unmet need for mental health care among US children: variation by ethnicity and insurance status. American Journal of Psychiatry 159:1548–1555, 2002Google Scholar
9. Kaslow NJ, Heron S, Roberts K, et al: Family and community factors that predict internalizing and externalizing symptoms in low-income, African American children. Annals of the New York Academy of Sciences 1008:55–68, 2003Google Scholar
10. Paranjape A, Heron S, Kaslow NJ: Utilization of services by abused, low-income African-American women. Journal of General Internal Medicine 21:189–192, 2006Google Scholar
11. Bernstein DP, Ahluvalia T, Pogge D, et al: Validity of the Childhood Trauma Questionnaire in an adolescent psychiatric population. Journal of the American Academy of Child and Adolescent Psychiatry 36:340–348, 1997Google Scholar
12. Bernstein DP, Fink L: Childhood Trauma Questionnaire: A Retrospective Self-Report. San Antonio, Tex, Harcourt Brace, 1998Google Scholar
13. Thompson R: The course and correlates of mental health care received by young children: descriptive data from a longitudinal urban high-risk sample. Children and Youth Services Review 27:39–50, 2005Google Scholar
14. Leslie LK, Hurlburt MS, James S, et al: Relationship between entry into child welfare and mental health service use. Psychiatric Services 56:981–987, 2005Google Scholar
15. Heim C, Newport DJ, Mletzko T, et al: The link between childhood trauma and depression: insights from HPA axis studies in humans. Psychoneuroendocrinology 33:693–710, 2008Google Scholar



