Changing Trends in State Psychiatric Hospital Use From 2002 to 2005
The number of consumers who use state psychiatric hospitals has decreased steadily over the past 50 years. This decrease is mainly the result of treatment trends emerging in the 1950s that included psychotropic medication and the development of a liberating, humane policy that served as an alternative to restrictive institutionalized care. Because of these innovations, behavioral health care diverged from its traditional institutional model and developed community-based services.
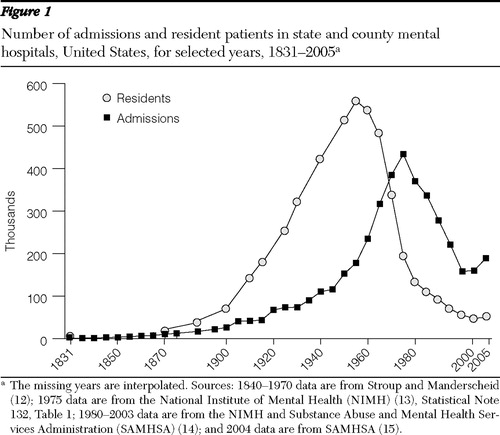
Over the longer term, since 1831, when the first data were collected, many changes have occurred in the state psychiatric hospital system. At that time, there were only 150 residents living in four state hospitals with total expenditures amounting to $30,000 a year. In subsequent years, the state hospitals were to become long-term custodial care institutions functioning as a source of control for persons who were perceived to be unable to care for themselves and whose behavior was perceived to be threatening to the social order. The number of residents increased steadily until 1955, when the total population peaked at nearly 559,000, with annual expenditures of $400 million and annual deaths between 48,000 and 50,000. Concurrently, the number of hospitals increased to 352, the largest number ever recorded ( 1 , 2 , 3 ). From that time forward, the number of residents declined steadily until 2003, when the number reached 47,000. Over $9 billion was spent on state psychiatric hospitals in 2003, with 70% of the funds coming from the states' mental health agencies. The annual number of admissions peaked in 1971 at 475,000 and declined thereafter, numbering less than 160,000 in 2002.
Despite these downward trends in the number of state hospital residents, Goldsmith and colleagues ( 4 ) predicted in 1993 a 25% increase by 2010 in the total number of inpatient admissions to all specialty mental health facilities. The estimates were based on trends in admission rates from 1980 to 1986, projected to 1990. The projected admission rates for 1990 were used with projections of the civilian population from 1990 to 2010 to produce the final estimates ( 4 ). Overall increases in the size of the population, the rising number of elderly people, and the growing number of persons in racial-ethnic minority groups all were expected to have a potential impact on the number of people using mental health facilities, especially the state psychiatric hospitals. At a later point, Salzer and colleagues ( 5 ) also examined a related phenomenon—a deceleration in the number of inpatients being discharged from public hospitals into the community. This slowdown began in the late 1990s and continued through 2005.
The objectives of this study were to determine whether the forecasted increases have been realized in recent years and, if so, to advocate for research on the factors that are suspected to have contributed to these increases. Because such findings would represent a significant departure from very long-term trends, they would have particular policy importance for the field.
Methods
Information on state psychiatric hospital admission and resident counts derives from state-level data collected by the Survey, Analysis, and Finance Branch, Center for Mental Health Services (CMHS), as part of its mission to report annual data on inpatient care. The survey, the Annual Census of Admission and Resident Patient Characteristics, State and County Mental Hospital 24-Hour Services (hereafter referred to as the annual census), collects from each state annual aggregate data on age, gender, race, and ethnicity, each by diagnosis, for year-end residents and annual admissions. Results are published in the CMHS report Admissions and Resident Patients at End of Year, United States . The annual census is the oldest continuous health survey in the United States ( 6 , 7 ).
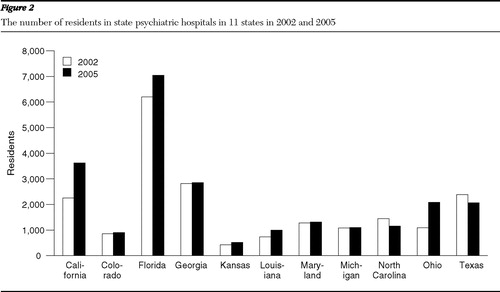
For this study, an inquiry was addressed to state mental health agency staff in the 11 key states that showed major increases in the number of state psychiatric hospital residents and admissions from 2002 to 2005, in order to discuss factors related to changes in the trends. Open-ended questions were asked of state statisticians or analysts in each of the states (California, Colorado, Florida, Georgia, Kansas, Louisiana, Maryland, Michigan, North Carolina, Ohio, and Texas). Eight states responded (California, Florida, Georgia, Louisiana, Maryland, Michigan, North Carolina, and Ohio). The inquiry was conducted to verify whether there had been an increase in admissions and residents and to request information on factors perceived to be related to the increase.
The results from the annual census were compared with the results from two other national data collections: the Survey of Mental Health Organizations, which was also conducted by CMHS and provided a complete biennial enumeration of all mental health organizations, and the Uniform Reporting System Output Tables, collected by the National Association of State Mental Health Program Directors Research Institute (NRI) for CMHS, to report data from state psychiatric hospitals on an annual basis. The results from these two data collections were congruent with annual census results.
Results
Between 2002 and 2005, the number of state psychiatric hospitals decreased from 220 to 204, and the bed capacity decreased 10.3%, from 58,000 in 2002 to 52,000 in 2005 ( 8 ). Many states reduced the number of beds, rather than the number of hospitals or residents ( 9 ).
The annual census showed that there was a significant increase in the number of admissions between 2002 and 2005, from 156,000 to 189,000, or 21.1% ( Table 1 ), and a slight increase in the number of year-end residents, from 49,500 to 50,000, or 1.0% ( 10 , 11 ). For admissions, this was the first increase since 1971. For year-end residents, this was the first increase since 1955, when the total resident population peaked at nearly 559,000. To put these results into a longer-term historical perspective, changes in the number of admissions and residents from 1831 to 2005 are shown in Figure 1 ( 12 , 13 , 14 , 15 ).
 |
Male-female admission ratios
The male-female admission ratio (M/F × 100) continues to remain high. Between 2002 and 2005, the number of male admissions increased 28.1%, and the number of female admissions increased 7.4%. Thus, for these two years, the ratios remained very high at 196 and 234, respectively. According to Stroup and Manderscheid ( 16 ), males are admitted to state psychiatric hospitals more frequently than females and are hospitalized for longer periods because of the perceived threat of dangerousness.
Changes in age groups
From 2002 to 2005, relatively large increases were noted in admissions in the 45–64 age group (33.3%) and in residents from this same age group (13.2%). These increases are indicative of a population growing older, as predicted by Goldsmith and colleagues ( 4 ) in 1993. However, sizable increases were also noted in the number of admissions in the under 18, 18–24, and 25–44 age ranges (27.0%, 19.8%, and 15.8%, respectively).
Changes in racial-ethnic groups
From 2002 to 2005, relatively large increases were noted in the number of white and African-American admissions, the most prevalent groups (increases of 30.8% and 9.9%, respectively). However, most of the increase in residents occurred among Asians and Pacific Islanders, Hispanics, and American Indians, which were the least prevalent groups (10.9%, 17.0%, and 18.3%, respectively).
Changes in diagnostic patterns
Schizophrenia. The most prevalent diagnosis in state psychiatric hospitals is schizophrenia. According to the annual census, the total number of admissions with schizophrenia diagnoses increased 23.2% from 2002 to 2005, and residents with schizophrenia increased by 3.0%.
Also of interest, in 2002, 50% of African-American state hospital residents were diagnosed as having schizophrenia (results not shown). By 2005 this number had increased to 70%. In 2002 over 38% of white residents had schizophrenia diagnoses. By 2005 this number had increased to 47%. In 2002, nearly 50% of Hispanic residents were diagnosed as having schizophrenia. By 2005 this number had increased to 67% of the reported Hispanic population in our sample. In both 2002 and 2005, 50% of Asian residents were diagnosed as having schizophrenia. Generally, the schizophrenia diagnoses increased for all groups except for persons of Asian descent ( 6 , 17 ).
Similarly, in 2002, 41% of African-American admissions had a diagnosis of schizophrenia; this percentage remained unchanged in 2005. In 2002, 23% of white admissions had diagnoses of schizophrenia. In 2005 this number increased to 24%. In both 2002 and 2005 Hispanic admissions included about 33% with schizophrenia diagnoses. Similarly, slightly more than 40% of the Asian admissions had schizophrenia diagnoses in this period.
Affective disorders. Between 2002 and 2005 admissions with affective disorders increased 16.3%. Residents with affective disorders increased 1.6% in this same period. Next to schizophrenia, affective disorders are the most prevalent diagnoses for patients in state psychiatric hospitals.
Affective disorders were more prevalent among whites than among other racial or ethnic groups. From 2002 to 2005 less than 10% of African-American residents were diagnosed as having affective disorders (results not shown). Among whites the comparable number was 16% of residents. In 2005 about 13% of Hispanic residents were diagnosed as having affective disorders.
Sixteen percent of African-American admissions had a diagnosis of an affective disorder. The parallel figure for whites was 31% and for Hispanics, more than 33% ( 6 , 7 , 17 ).
State reports about factors in the increases
The state that showed the largest consistent increase since 2000 in both annual admissions and year-end residents was California ( Figures 2 and 3 ). The admissions in this state increased 109% from 2000 to 2005, accompanied by a 2% increase in the number of residents (results not shown). All ten other states showed increases in admissions, residents, or both over the six-year period. Most of the 11 states studied showed consistent increases since 2000 ( 7 ). Staff persons from the state mental health agencies of each of these states were asked to participate in a brief telephone interview.
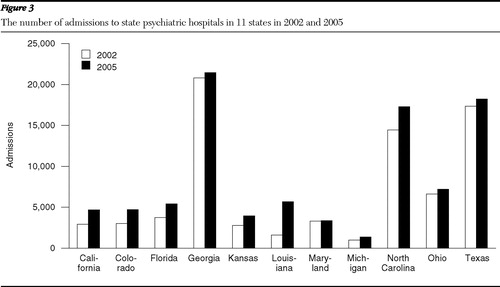
The eight states that participated in the interview (California, Florida, Georgia, Louisiana, Maryland, Michigan, North Carolina, and Ohio) reported that several factors were related to the increases in the number of residents and admissions. These factors included an increase in the forensic population (reported by seven of the eight states that participated), an increase in consumers diagnosed as having schizophrenia or affective disorders, and shortages of community housing and community care staff.
Discussion and conclusions
State psychiatric hospitals have continued to receive considerable attention from researchers and policy analysts during the past decade. Geller ( 18 ) provided a sweeping view over the past 50 years, and Mechanic and colleagues ( 19 ) gave a more detailed view over a decade. Torrey and colleagues ( 20 ) decried the lack of beds, and Salinsky and Loftis ( 9 ) presented a pro-and-con policy analysis of this issue. Never far from the surface in these analyses are concerns about the effects of deinstitutionalization in the absence of parallel efforts to build strong community services. In this tradition, this study was the first to show growth of admissions and residents in state psychiatric hospitals since the beginning of deinstitutionalization in 1955.
The increases in the number of admissions and residents in state psychiatric hospitals between 2002 and 2005 was a marked reversal from trends over a very long term. These increases may be related to several factors. State staff reported larger numbers of patients entering state psychiatric hospitals via the criminal justice system, more consumers with schizophrenia and affective disorders, and lack of available community housing and staff.
The reports by staff from mental health agencies were corroborated by independent data. For a 2004 NRI report on forensic state hospitals, the 36 state hospitals that responded to the survey questions reported a total of 40,000 residents, at least 14,000 (35%) of whom were forensically involved mental health care consumers ( 21 ). Over half of the beds in some state psychiatric hospitals are occupied by these consumers ( 22 ). Recently built state hospitals have been constructed solely for forensically linked mental health care consumers or for sex offenders ( 23 ). The continuing high male-female ratio observed in these data is congruent with an increase in the number of persons with mental illness who are forensically involved.
Unfortunately, researchers currently know very little about the precise dynamics through which a person with mental illness moves from the community to become a forensically involved patient in a state psychiatric hospital. Thus this report is an urgent call for research to investigate these dynamics. We can speculate that the dynamics involve the lack of availability of community-based mental health services; the large and growing number of persons with mental illness who receive no services at all; the interaction between a person and the police, in which the person becomes defined as having a mental illness and as being a criminal; the sorting process used by the court system to determine whether a person with a mental illness will be sent to a prison or to a state psychiatric hospital; and the ease or difficulty of entering a state psychiatric hospital. However, these remain only speculations in the absence of good research. We need to determine evidence about the dynamics and their operation. Initially, this is likely to involve descriptive work in the community, followed by more complex research designs as our knowledge develops.
The annual census data and the results from other studies raise important questions about the new state psychiatric hospital trends reported here for the first time. From a policy perspective, continued monitoring of state psychiatric hospital trends is clearly warranted, and research is urgently needed on the dynamics leading to these trends. These new trends may indicate important, long-term changes.
Acknowledgments and disclosures
Dr. Manderscheid is a consultant on continuity of care to Janssen Pharmaceuticals. The other authors report no competing interests.
1. Frank RG, Glied SA: Better But Not Well: Mental Health Policy in the United States Since 1950. Baltimore, Johns Hopkins University Press, 2006Google Scholar
2. Grob G, Goldman H: The Dilemma of Federal Mental Health Policy. New Brunswick, NJ, Rutgers University Press, 2007Google Scholar
3. Witkin MJ, Atay J, Manderscheid RW: Trends in state and county mental hospitals in the US from 1970 to 1992. Psychiatric Services 47:1079–1081, 1996Google Scholar
4. Goldsmith HF, Manderscheid RW, Henderson MJ, et al: Projections of inpatient admissions to specialty mental health organizations: 1990 to 2010. Hospital and Community Psychiatry 44:478–483, 1993Google Scholar
5. Salzer MS, Kaplan K, Atay J: State psychiatric hospital census after the 1999 Olmstead Decision: evidence of decelerating deinstitutionalization. Psychiatric Services 57:1501–1504, 2006Google Scholar
6. Atay J, Manderscheid RW, Male AA, et al: Additions and Resident Patients at End of Year, State and County Mental Hospitals, by Age and Diagnosis, by State, United States, 2003. Rockville, Md, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services, 2004Google Scholar
7. Atay J, Crider R, Foley D, et al: Background Report, Admissions and Resident Patients, State and County Mental Hospitals, United States, 2004. Rockville, Md, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services, 2006Google Scholar
8. Foley D, Manderscheid RW, Atay J: Highlights of organized mental health services in 2002 and major national and state trends, in Mental Health, United States, 2004. Edited by Manderscheid RW, Berry J. DHHS SMA-06-4195. Rockville, Md, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services, 2007Google Scholar
9. Salinsky E, Loftis C: Shrinking inpatient psychiatric capacity: cause for celebration or concern. Presented at the National Health Policy Forum, George Washington University, Washington, DC, Aug 1, 2007Google Scholar
10. Survey of Mental Health Organizations (SMHO), 2004. Rockville, Md, Substance Abuse and Mental Health Services Administration, 2004Google Scholar
11. Uniform Reporting Tables, 2003–2005. Alexandria, Va, National Association of State Mental Health Program Directors, 2005Google Scholar
12. Stroup AL, Manderscheid RW: The development of the state mental hospital system in the United States: 1840–1980. Journal of the Washington Academy of Sciences 78:59–68, 1988Google Scholar
13. National Institute of Mental Health (NIMH), Statistical Note 132, Provisional Patient Movement and Administrative Data, State and County Psychiatric Inpatient Services, July 1, 1974–June 30, 1975, Table 1 . Rockville, Md, National Institute of Mental Health, July 1976 Google Scholar
14. Additions and Resident Patients at End of Year, State and County Mental Hospitals, by Age and Diagnosis, by State, United States, 2003, Table 2. Rockville, Md, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services, 2004Google Scholar
15. Background Report, Admissions and Resident Patients, State and County Mental Hospitals, United States, 2005. Rockville, Md, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services, 2007Google Scholar
16. Stroup AL, Manderscheid RW: Male-female admission differentials in state mental hospitals, 1889–1980. Journal of the Washington Academy of Science 78:259–270, 1988Google Scholar
17. Atay J, Crider R, Foley D, et al: Background Report, Admissions and Resident Patients, State and County Mental Hospitals, United States, 2005. Rockville, Md, Center for Mental Health Services, 2007Google Scholar
18. Geller JL: The last half-century of psychiatric services as reflected in Psychiatric Services. Psychiatric Services 51:41–67, 2000Google Scholar
19. Mechanic D, McAlpine DD, Olfson M: Changing patterns of psychiatric inpatient care in the United States, 1988–1994. Archives of General Psychiatry 55:785–791, 1998Google Scholar
20. Torrey EF, Entsminger K, Geller J, et al: The Shortage of Public Hospital Beds for Mentally Ill Persons. Arlington, Va, Treatment Advocacy Center, unpublished manuscript, Mar 2008. Available at www.treatmentadvocacycenter.org Google Scholar
21. State Forensic Mental Health Services: 2004, State Profile Highlights. Alexandria, Va, National Association of State Mental Health Program Directors Research Institute, 2005Google Scholar
22. Schmelling S: The person and prison, mental illness discussion highlights need for change. NIH Record 59(15), July 2007. Available at nihrecord.od.nih.gov/newsletters/2007/07272007 Google Scholar
23. Lutterman T: Trends in SMHA mental health services. Presented at the National Grantee Conference on the Mental Health Block Grant and Data, Leading Change in Mental Health Systems, Washington DC, May 20–22, 2008Google Scholar



