Psychiatric Disease Burden Profiles Among Veterans With Epilepsy: The Association With Health Services Utilization
Comorbid psychiatric illness among patients with epilepsy is an increasing concern. Extant research reports that persons with epilepsy are more likely to have depression, anxiety, psychosis, personality disorders, and substance abuse, compared with those without epilepsy ( 1 , 2 ). Although the magnitude of these differences and presence of a bidirectional effect between psychiatric disorders and epilepsy may be debated, the impact of comorbid psychiatric illness is far from benign.
Studies suggest that the detrimental impact of depression or anxiety on health status may be even greater than seizure frequency or severity ( 3 , 4 ). The severity of comorbid depression and epilepsy is also associated with diminishing quality of life ( 5 ). Moreover, patients with epilepsy and concomitant depression have greater health care utilization than those reporting no depression ( 6 ).
Although the existing literature provides evidence of the impact of psychiatric comorbidity on health status and health care utilization for patients with epilepsy, studies have rarely examined the existence of multiple psychiatric conditions. The purpose of this study is to identify patterns of concomitant psychiatric disorders found among veterans with epilepsy. We first describe the patterns of documented psychiatric diagnoses (hereafter referred to as psychiatric comorbidities) found among patients with epilepsy treated in the U.S. Veterans Health Administration (VA). Then we compare health care utilization for patients with epilepsy only and patients with epilepsy and different psychiatric comorbidity profiles.
Methods
To maximize generalizability of our conclusions regarding psychiatric comorbidity among patients with epilepsy, we identified our cohort by using data collected before deployment of troops to Afghanistan and Iraq.Rates of posttraumatic stress disorder (PTSD) may be significantly higher inthe cohortof veterans exposed to combat for the first time. We used national VA administrative databases to identify veterans with epilepsy in fiscal year (FY) 1999 (October 1, 1998, to September 30, 1999), using an algorithm previously validated in the VA ( 7 , 8 ). The cohort consists of individuals with an epilepsy diagnosis ( ICD-9 codes starting with 345) or convulsion (780.39) in FY 1997–1999 who also received an antiepileptic drug from a VA pharmacy in FY 1999. Additional details on this algorithm can be found elsewhere ( 7 ).
From the 59,429 veterans who met our inclusion criteria, we retained 23,752 patients who also responded to the 1999 Large Health Survey of Veterans (LHS), a sample of 1.4 million VA enrollees eligible to use VA health care services. The LHS randomly sampled 40% of eligible veterans and had a 65% response rate among those who were not deceased and for whom contact information was accurate.
We used ICD-9 codes to identify the following psychiatric comorbidities in this cohort: schizophrenia (295.x, excluding 295.5), bipolar disorder (296.0–296.1 and 296.4–296.8), other psychosis (297–298), depression (296.2–296.3 and 311), anxiety (300.00, 300.02, and 300.09), PTSD (309.81), substance abuse (291, 292, and 303–305, excluding 305.1), and other mental illness (290–312, excluding the codes listed above). To simplify description of the most significant types of psychiatric conditions, we combined disorders to form five psychiatric disease burden groups: serious mental illness as defined by Blow and colleagues ( 9 ) (schizophrenia, other psychosis, or bipolar disorder), affective disorders (depression or anxiety), PTSD, other mental illness, and substance abuse. PTSD was retained as a separate category because of its association with combat experience, which may be different in our sample than in nonmilitary populations ( 10 ).
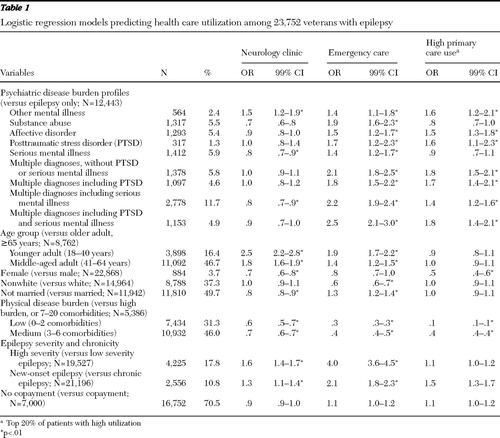
To better understand the patterns of concomitant diagnoses, we developed mutually exclusive psychiatric disease burden profiles. Patients with single psychiatric comorbidities were specified as such. Because serious mental illness and PTSD have been found to have different and significantly detrimental impacts on self-reported health status among patients with epilepsy ( 11 ), we classified multiple psychiatric comorbidities by using the following hierarchy: multiple diagnoses without PTSD or serious mental illness, multiple diagnoses including PTSD, multiple diagnoses including serious mental illness, and multiple diagnoses including PTSD and serious mental illness. This classification system yielded nine different psychiatric disease burden profiles ( Table 1 ).
 |
We used VA clinic codes to identify the following utilization measures: primary care, neurology, and emergency outpatient utilization during FY 1999. Because of skewed distributions, we recategorized measures as any emergency care, any neurology care, and high primary care utilization (the top 20%, that is, six or more visits).
Covariates included demographic and clinical characteristics. Demographic characteristics (age, sex, race, and marital status) were obtained primarily from administrative data, but because of high rates of missing race data, we used patients' self-report of race on the LHS for those with missing race data. We dichotomized marital status into married versus nonmarried and race into white versus nonwhite (that is, black, Hispanic, other, and unknown).
Clinical characteristics included epilepsy chronicity, epilepsy severity, and physical comorbidities. Epilepsy was classified as either new onset or chronic. Patients with diagnoses between FY 1997–1998 were classified as having chronic epilepsy. Those with a first diagnosis in FY 1999 who also received care in the VA system FY 1997–1999 were defined as having new-onset epilepsy. Those first diagnosed in FY 1999 without prior VA care were considered to have unknown onset and were excluded from analyses.
Epilepsy severity was identified by using a proxy measure previously found to be an indicator of more severe epilepsy ( 8 ). Individuals were identified as having more severe epilepsy if they received emergency or hospital care with a primary diagnosis of epilepsy; a diagnosis of status epilepticus; parenteral forms of fosphenytoin, phenytoin, or benzodiazepines; or a diagnosis of intractable epilepsy.
Physical comorbidities were identified by using ICD-9 codes for 26 physical disease states and summed to produce a measure of physical disease burden. We categorized patients into three groups by quartile: low (lowest quartile, none to two disease states), medium (middle two quartiles, three to six disease states), and high (top quartile, seven to 20 disease states).
Because outcomes assessed in this study represent use of health care services, we also controlled for potential barriers to access. Patients with no copayment requirement (that is, service-connected disability ≥50% or very low income) had no financial barrier to receiving care and were compared with those with a required copayment.
We first describe the cohort and then use logistic regression analyses to determine the extent to which patients with different psychiatric disease burden profiles were likely to receive each type of health care, compared with patients with epilepsy only, after controlling for sociodemographic and clinical characteristics. The study was approved by the University of Texas Health Science Center at San Antonio's institutional review board. All analyses were conducted with SPSS 14.
Results
Our cohort consisted of 23,752 patients with epilepsy who returned LHS surveys and received VA care in FY 1997–1999. These individuals were predominantly male (N=22,868, or 96%) and white (N=14,964, or 63%). A total of 4,275 were black (18%), 950 were Hispanic (4%), 238 were from another race (1%), and the race was unknown for 3,325 (14%). Approximately half were married (N=11,942, or 50%). The mean±SD number of physical comorbidities was 4.4±3.0. Patients with new-onset epilepsy accounted for 11% of the cohort, and 18% of the cohort were classified as having more severe epilepsy.
Nearly half of the cohort had at least one psychiatric comorbidity (N=11,312, or 48%). Of those, 27% (N=3,072) had diagnoses for two distinct types of psychiatric diagnostic groups, 17% (N=1,865) had three, 9% (N=1,065) had four, and 4% (N=401) had five. Individuals with multiple psychiatric diagnoses accounted for approximately 57% (N=6,403) of veterans with psychiatric comorbidity. Table 1 shows the distribution of psychiatric disease burden profiles.
In this cohort, the median number of primary care visits within the VA was three (mean 3.7±4.1); 20% of patients (N=4,838) had six or more primary care visits in FY 1999. Moreover, 46% (N=10,969) received emergency care, and 41.9% (N=9,947) received neurology care in FY 1999.
Table 1 presents odds ratios and 99% confidence intervals for the logistic regression analysis assessing the likelihood of health care utilization by psychiatric disease burden profile. Individuals with serious mental illness and those with multiple conditions including serious mental illness were less likely than those who had only epilepsy to receive neurology care. Individuals with other mental illnesses were more likely to receive neurology care than individuals with epilepsy only. Those with any psychiatric comorbidity were more likely to receive emergency care than those with epilepsy only, and all groups with psychiatric comorbidity except those with substance abuse and serious mental illness were more likely than those with epilepsy alone to have high primary care utilization.
Discussion
Prior studies have rarely examined the extent of multiple psychiatric comorbidities among patients with epilepsy or the implications of such comorbidity for health services utilization. This study is the first to fully evaluate the panoply of psychiatric illnesses in a national sample of VA patients with epilepsy. These results suggest that multiple psychiatric comorbidities are quite common in this population. Moreover, our findings indicate that the presence of multiple psychiatric comorbidities and their distinct patterns are associated with health care utilization ( 6 ).
Our results indicate that it is common for veterans with epilepsy to receive emergency care, despite a relatively high rate of neurology care and frequent contact with their primary care provider. Because a number of studies, for example, a study by Ghose and colleagues ( 12 ), have identified higher health care utilization for patients with psychiatric comorbidity and other chronic diseases, this finding is not surprising. Nonetheless it highlights the complexity introduced to epilepsy care when patients have psychiatric comorbidity.
The finding that patients with serious mental illness, with or without multiple conditions, were less likely to receive neurology care than were patients with epilepsy only suggests that coordination of care may be particularly problematic for those patients. These patients differ in that they may lack insight into their illness, have trouble coordinating care for several chronic conditions, or simply place too many competing demands on clinical time ( 13 ) to accommodate specialty neurology care. It is also possible that the doctor-patient relationship between these patients and their multiple providers overwhelms available coordination of care efforts and services ( 14 ). Neurology care has been associated with more appropriate prescribing for older veterans with epilepsy ( 8 ), and prior research indicates that patients with psychiatric comorbidities are less likely to receive high-quality care than similar patients without psychiatric comorbidities ( 15 ). Accordingly, future research should more closely examine psychiatric comorbidity profiles of patients with epilepsy to see how these profiles correspond to the quality of care provided and examine the role of psychiatric care within the context of epilepsy and mental health treatment.
Our findings must be interpreted in light of several potential limitations. First, psychiatric comorbidity was identified by using diagnoses from administrative databases. Yet, because 70% of the individuals with a psychiatric diagnosis in this cohort had at least one psychiatric visit in FY 1999 alone, we have confidence that individuals having a psychiatric diagnosis were accurately identified.
The second is related to generalizability. Our data did not allow us to examine differences in psychiatric disease burden profiles among patients with different types of epilepsy and seizure disorders. This population is one in which there are few patients with seizures that occur in childhood or adolescence, and some of the cases of epilepsy may be related to head trauma sustained during military service. Moreover, this cohort was primarily male, so further assessment of psychiatric disease burden profiles among women is needed. Thus the ability to generalize to all patients with epilepsy from this VA sample may be limited. However, these findings suggest that it is critical to examine this question in a non-VA population because the VA system requires mood disorder screening for all primary care patients and because mental health care is more readily available in the VA system than in many sectors of society.
Conclusions
Multiple psychiatric comorbidities are common among veterans with epilepsy, and these patterns are associated with variations in health care utilization that may have implications for the quality of care provided. Our findings suggest the need for additional research into new populations to ascertain the prevalence of these psychiatric disease burden profiles, the quality of care provided to patients with different patterns of psychiatric comorbidity, and how care is coordinated for these extraordinarily complex patients. Such identification will allow adequate treatment and social services planning to optimize treatment and outcomes for these patients.
Acknowledgments and disclosures
This study was funded by the Department of Veterans Affairs, Health Services Research and Development Service Merit Review Entry Program Award (MRP-02-267, MRP-05-145, and IIR 02-274). The authors also acknowledge the Veterans Health Administration Office of Quality and Performance for providing access to data from the 1999 Large Health Survey of Veteran Enrollees. The authors thank Ann VanCott, M.D., and Alan Ettinger, M.D., for their comments.
The authors report no competing interests.
1. Qin P, Xu H, Laursen TM, et al: Risk for schizophrenia and schizophrenia-like psychosis among patients with epilepsy: population based cohort study. British Medical Journal 331:23, 2005Google Scholar
2. Swinkels WA, Kuyk J, Dyck R, et al: Psychiatric comorbidity in epilepsy. Epilepsy and Behavior 7:37–50, 2005Google Scholar
3. Boylan LS, Flint LA, Labovitz DL, et al: Depression but not seizure frequency predicts quality of life in treatment-resistant epilepsy. Neurology 62:258–261, 2004Google Scholar
4. Johnson EK, Jones JE, Seidenberg M, et al: The relative impact of anxiety, depression, and clinical seizure features on health-related quality of life in epilepsy. Epilepsia 45:544–550, 2004Google Scholar
5. Cramer JA, Blum D, Reed M, et al: The influence of comorbid depression on quality of life for people with epilepsy. Epilepsy and Behavior 4:515–521, 2003Google Scholar
6. Cramer JA, Blum D, Fanning K, et al: The impact of comorbid depression on health resource utilization in a community sample of people with epilepsy. Epilepsy and Behavior 5:337–342, 2004Google Scholar
7. Pugh MJ, Van Cott AC, Cramer JA, et al: Trends in antiepileptic drug prescribing for older patients with new-onset epilepsy: 2000–2004. Neurology 70:2171–2178, 2008Google Scholar
8. Pugh MJ, Cramer J, Knoefel J, et al: Potentially inappropriate antiepileptic drugs for elderly patients with epilepsy. Journal of the American Geriatrics Society 52:417–422, 2004Google Scholar
9. Blow FC, Ullman E, Barry KL, et al: Effectiveness of specialized treatment programs for veterans with serious and persistent mental illness: a three-year follow-up. American Journal of Orthopsychiatry 70:389–400, 2000Google Scholar
10. Hoge CW, Terhakopian A, Castro CA, et al: Association of posttraumatic stress disorder with somatic symptoms, health care visits, and absenteeism among Iraq war veterans. American Journal of Psychiatry 164:150–153, 2007Google Scholar
11. Zeber JE, Copeland LA, Amuan M, et al: The role of comorbid psychiatric conditions in health status in epilepsy. Epilepsy and Behavior 10:539–546, 2007Google Scholar
12. Ghose SS, Williams LS, Swindle RW: Depression and other mental health diagnoses after stroke increase inpatient and outpatient medical utilization three years poststroke. Medical Care 43:1259–1264, 2005Google Scholar
13. Hofer TP, Zemencuk JK, Hayward RA: When there is too much to do: how practicing physicians prioritize among recommended interventions. Journal of General Internal Medicine 19:646–653, 2004Google Scholar
14. Druss BG, Rosenheck RA, Desai MM, et al: Quality of preventive medical care for patients with mental disorders. Medical Care 40:129–136, 2002Google Scholar
15. Frayne SM, Halanych JH, Miller DR, et al: Disparities in diabetes care: impact of mental illness. Archives of Internal Medicine 165:2631–2638, 2005Google Scholar



