Co-occurring Psychiatric and Substance Use Disorders: A Multistate Feasibility Study of the Quadrant Model
Co-occurring substance use and psychiatric disorders are of significant interest to policy makers, researchers, treatment providers, and consumers of services ( 1 , 2 ). National initiatives have been focused on developing evidence-based practices, developing guidelines for systems change, and exploring potential improvements in the financing of services, many of which are publicly funded ( 3 , 4 , 5 , 6 , 7 , 8 ).
Although recommendations to examine the delivery of health care services across systems have been made, there have been few studies at the consumer level ( 4 , 8 , 9 , 10 , 11 ). Two factors may account for this. One is that the utilization of services across systems is difficult to track ( 1 , 3 , 6 , 12 ). The second factor is the heterogeneity of persons with co-occurring disorders. This population ranges, for instance, from persons with severe mental illnesses and drug abuse disorders to those with alcohol dependence disorders and dysthymia ( 13 , 14 ). This heterogeneity results in differential health care benefits, utilization of different service settings and different types of evidence-based practices, and potentially different illness course and outcomes ( 14 , 15 , 16 ).
In a 2002 report to Congress, the Substance Abuse and Mental Health Services Administration referred to a conceptual model to organize the range of persons with co-occurring disorders, the likely settings to which they present for services, and the nature of the relationships between service providers necessary to optimize outcomes ( 1 ). Figure 1 portrays a simplified adaptation of the graphic version of the framework, often referred to as the quadrant model, which aligns persons on two axes: severity of substance use and severity of psychiatric disorders ( 17 ). Persons in quadrant I (low severity of psychiatric and substance use disorders) are hypothesized to use services primarily in the health care system; quadrant II (high severity of psychiatric disorders and low severity of substance use disorders), the mental health system; and quadrant III (high severity of substance use disorders and low severity of psychiatric disorders), the addiction treatment system. Persons in quadrant IV (high severity of psychiatric and substance use disorders) are hypothesized to use multiple systems and to make more frequent use of emergency and inpatient services ( 1 , 17 ).
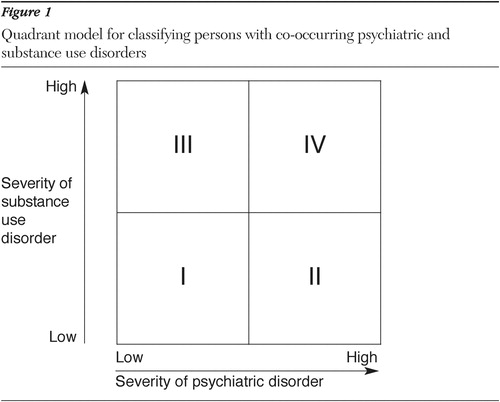
With origins traced to Ries and colleagues ( 18 , 19 ) and Rosenthal ( 20 ) and sometimes referred to as the "New York" model, this framework was deemed useful for guiding dialogue and system planning by national leaders in 1998 ( 17 ). As a pragmatic heuristic, the quadrant model has enabled policy makers and treatment providers to organize and define populations and treatments under consideration ( 1 , 3 , 17 ). A recent summation of findings from a virtual consensus panel noted that the quadrant model, although challenging to operationalize, was useful in conceptualizing systems-level factors but lacked specificity to guide practice ( 21 ).
There have been no tests of the feasibility of the quadrant model, either within systems or across systems of care. One study, a survey of addiction treatment professionals (N=453) from a single state, reported data from the quadrant model at the provider level ( 22 ). The addiction treatment providers estimated that about half (50%) of their patients with co-occurring disorders could be classified as being in quadrant III (high severity of substance use disorders and low severity of psychiatric disorders). Relatively high percentages (24.5%) were also reported of persons classified in quadrant IV (high severity of psychiatric and substance use disorders). This single study provided some support for the construct validity and promise of the model.
Objective study of the quadrant model is needed. For example, can persons with co-occurring disorders be reliably categorized by quadrant? Are quadrants associated with service utilization and costs? Should treatments for persons presenting for services be influenced by the quadrant that they are classified in? Because the model appears to have widespread recognition and face validity, its feasibility as a mechanism to organize and study patient populations with co-occurring disorders should be tested.
The research presented here sought to operationally define the quadrants to examine the distribution of patient-level data from persons with co-occurring disorders who receive Medicaid-funded treatment. Medicaid beneficiaries comprise the largest portion of persons with co-occurring disorders who receive public funding for services ( 23 ). By analyzing Medicaid claim diagnostic and service utilization data, information can be gathered across systems. The purpose of this study was to test the feasibility of applying the quadrant model to a Medicaid sample by using service claims from six states.
Three key questions in testing the feasibility of the quadrant model will be addressed. First, can operational definitions be developed and can persons with co-occurring disorders be categorized by quadrant? Second, as an estimate of reliability, are these categorizations and quadrant assignments consistent and replicable across state service systems? Third, as an estimate of validity, are quadrants associated with differential service utilization? Specifically, are persons in quadrant IV more likely to use inpatient and emergency department services?
Testing the feasibility of the quadrant model with state service system data may provide more objective information about the prevalence and range of persons with co-occurring disorders, their characteristics, and service utilization patterns. It may also serve to provide other states with a simple method to analyze their own data for similar trends, in order to guide policy and financing and suggest further research.
Methods
Data and sampling
We analyzed 1999 Medicaid analytic extract data (MAX files) obtained from the Centers for Medicare and Medicaid Services from six states: Arkansas, Colorado, Georgia, Indiana, New Jersey, and Washington. These states form the sample with which to examine the reliability of quadrant categories and prevalence, as well as the validity of service utilization by quadrant. The state Medicaid programs' eligibility criteria, reimbursable benefit types, and policies for mental health and addiction treatment service financing are described elsewhere ( 23 ). Claims data contain information about demographic characteristics, eligibility for services, and Medicaid-reimbursed inpatient, outpatient, and long-term care and prescription medication utilization. The data combine all fee-for-service claims with similar encounter-level data submitted by managed care providers, thus providing a complete record of services paid for by Medicaid. Relevant variables from the claims files were matched with each beneficiary's enrollment record to create a person-level file for each state. Our analyses included beneficiaries between 0 and 64 years of age without additional third-party insurance coverage. Beneficiaries with third-party coverage other than Medicaid were eliminated because claims from those insurers were not available for study.
Committees for the protection of human subjects from the University of Massachusetts Medical School and the Trustees of Dartmouth College reviewed and approved this study.
Diagnostic groups
Twelve-month diagnosed prevalence of mental disorders was identified from the following principal ICD-9 diagnoses listed on claims: 295.x to 300.x and 302 to 315. Beneficiaries with schizophrenia, bipolar disorder, or major depression were considered to have a severe mental illness. They were considered to have a substance use disorder if they were diagnosed as having a principal or additional diagnosis of alcohol or drug abuse or dependence, including ICD-9 codes 291, 292, 303, 304, 305, and 648.3.
Classification by quadrant
The following scheme was used to assign beneficiaries to each of the four quadrants.
Quadrant I. Low psychiatric severity: anxiety, mood, personality, and behavioral disorders; low substance severity: substance abuse disorders.
Quadrant II. High psychiatric severity: schizophrenia, bipolar, schizoaffective, and major affective disorders; low substance severity: substance abuse disorders.
Quadrant III. Low psychiatric severity: anxiety, mood, personality, and behavioral disorders; high substance severity: substance dependence disorders.
Quadrant IV: High psychiatric severity: schizophrenia, bipolar, schizoaffective, and major affective disorders; high substance severity: substance dependence disorders.
Persons with multiple diagnoses—for example, schizophrenia and posttraumatic stress disorder plus alcohol dependence and cocaine abuse—who may qualify for more than one quadrant—were placed in the most severe category, for example, quadrant IV (schizophrenia and substance dependence).
Demographic characteristics
Demographic data extracted for this study included gender, race (white, African American, Hispanic, or other), and age cohort (younger than 21, 21–44, or 45–64 years).
Place of service
For validity testing we analyzed use of inpatient and emergency services, negative indicators for community-based services and therapeutic engagement ( 4 , 8 ). We also elected this focus because of variation in missing data for outpatient services across states.
Statistical analyses
Pearson chi square statistics were used to test for statistical differences in gender, race, age, and place of service across quadrants. Binary logistic regression models were used to test for the significance and magnitude of association between quadrant and place of service.
Results
Overall, across the six states 3.9 million Medicaid beneficiaries met the inclusion criteria for age and insurance coverage. Of these, 310,396 had only mental health disorders, 34,402 had only a substance use disorder, and 23,664 had co-occurring psychiatric and substance use disorders. Approximately 3.2% of beneficiaries with co-occurring disorders (N=752) could not be assigned to a quadrant because their substance use was identified on the basis of service use rather than diagnosis. Thus the total sample across the six states was 22,912 individuals. Missing data were negligible for age and gender (.9%), and for race (6.4%). Complete data were available for both inpatient and emergency services.
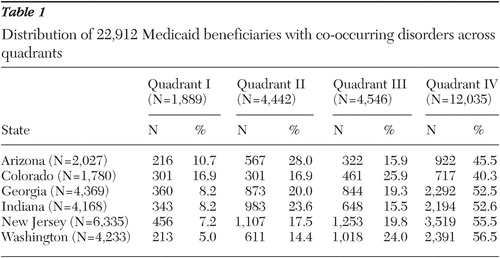
Table 1 depicts the distribution of this group by quadrant. Across all six states in total, the largest group was quadrant IV (high severity of both psychiatric disorders and substance use) (52.5%), followed by quadrant III (high severity of substance use disorders and low severity of psychiatric disorders) (19.8%), quadrant II (high severity of psychiatric disorders and low severity of substance use disorders) (19.4%), and quadrant I (low severity of psychiatric and substance use disorders) (8.2%). Ranges by state are displayed in Table 1 . Quadrant IV was consistently the highest (40.3%–56.5%), and quadrant I was consistently the lowest (5.0%–16.9%).
 |
With respect to gender, across states women were significantly more common in quadrants II (52%–62%) and quadrant IV (52%–63%), and men were significantly more common in quadrant I (52%–64%) and quadrant III (43%–71%) ( χ2 =278.2, df=6, p<.001) ( Table 2 ). Although some states had statistically significant racial differences, racial distribution was equivalent across quadrants. Age cohort varied substantially by quadrant. More than twice as many persons were younger than age 21 in quadrant III (28%) than in quadrant IV (13%), and nearly twice as many were younger than age 21 in quadrant I (56%) than in quadrant II (34%) ( χ2 =2,257.0, df=6, p<.001).
 |
Table 2 also shows that the use of inpatient and emergency departments also varied considerably by quadrant. Persons with severe psychiatric problems (quadrants II and IV) were three to four times more likely than those in quadrants I and III to be treated in inpatient settings (15%–54% versus 4%–22%) ( χ2 =1,718.2, df=3, p<.001). Odds ratios ranged from 3.2 (95% CI=2.5–4.3) (Colorado) to 8.1 (95% CI=6.5–10) (Georgia). With respect to emergency department visits, more severe psychiatric problems (quadrants II and IV) were again associated with increased utilization (15%–46% versus 7%–29% for quadrants I and III, respectively) ( χ2 =342.1, df=3, p<.001). Odds ratios for this comparison were less robust than those for inpatient utilization, ranging from 1.4 (95% CI=1.1–1.8) (Colorado) to 2.6 (95% CI=2.2–3.0) (Georgia).
The combined observations in Table 2 suggest that persons classified as having more severe psychiatric problems (quadrants II and IV) were more likely to be female, to be older, and to have been hospitalized or to have visited an emergency department.
Discussion
Summary of findings
The purpose of this investigation was to examine the feasibility of applying the quadrant model to state system-level data. We attempted to classify persons by diagnosis into quadrants, examine the reliability of quadrant distribution across six states, and explore validity by differential service use by quadrant. On the basis of our analyses of Medicaid claims data from six states for the year 1999, it appears that the quadrant model has promise.
In response to the first research question, can operational definitions be developed and can persons with co-occurring disorders be categorized by quadrant, it was possible to create and consistently identify quadrant membership of persons across a sample of six different states.
The second research question pertained to the reliability and consistency of quadrant "membership" across states. These data demonstrated a reliable pattern: quadrant IV was the most populated (40.3% to 56.5%) and quadrant I was the least (5.0% to 16.9%). The six states were generally equivalent in the proportion of persons in quadrant II (14.4% to 28.0%) and quadrant III (15.9% to 25.9%) and overall (19.4% and 19.8% for quadrant II and quadrant III, respectively).
In response to our third research question, which concerned validity, we hypothesized that persons in quadrant IV would have the highest utilization of the most expensive services. Quadrant IV utilization was greater than other quadrants for both inpatient hospital and emergency department visits in nine of the 12 (75%) possible comparisons (two settings by six states). In Washington, quadrant II utilization was greater than quadrant IV utilization for both settings, and in Arizona it was greater for emergency department visits only.
Across the quadrants and states, psychiatric disorder severity, not substance use severity, was most associated with utilization of the more expensive inpatient and emergency department services. Having a high level of psychiatric severity (quadrant II or IV) versus a lower level of psychiatric severity (quadrant I or III), regardless of substance use severity, increased dramatically the chances of receiving inpatient services and consistently raised the likelihood of emergency department visits.
Limitations
It is unlikely that claims data completely capture either the epidemiological or clinical realities of persons with co-occurring disorders. Claims data depend on a number of events, from patients' reporting or demonstrating symptoms to providers' identifying and recording information on medical records and Medicaid claim forms ( 24 ). Factors too numerous to detail here likely place the present estimates of co-occurring disorders at the lower end of a possible range, especially relative to epidemiological data ( 25 , 26 , 27 ).
The design of this study also assumed that use of the most expensive services, inpatient and emergency department, were indicative of less engagement with community services and poorer outcomes. We had no reliable measure of utilization of outpatient services or overall functioning, so these inferences may be negatively biased.
The quadrant model also has reductionistic features. Severity, both in terms of substance use and psychiatric problems, is likely not on a two-dimensional continuum. To draw a line between low and high severity, based on diagnosis, does not take into account the range of severity within diagnostic groups or the level of acuity of the clinical presentation during any given treatment episode. This line therefore provides the basis for future research.
Despite these caveats, the quadrant model has nonetheless been well adopted conceptually by community providers and policy makers ( 21 ). The consistency of the findings of the quadrant representation across six state Medicaid systems supports the potential utility of the quadrant model to articulate characteristics and service utilization patterns.
A final limitation is the use of data from six states for one year. Although the findings were consistent, this study should be replicated with other states and time periods.
Implications
This study suggests that the quadrant model has pragmatic utility for state policy makers, researchers, and clinical system leaders. The classification of persons with co-occurring disorders by quadrant provides simple and useful information about prevalence rates, characteristics, and service use. We employed Medicaid claims data from six states gathered from 1999. The findings were remarkably consistent across states. Future research by each state and analysis of more recent annual data (or multiple-year data) are recommended. In fact, any given state could analyze changes in patterns over time using this method.
Among Medicaid beneficiaries, persons with co-occurring disorders were more commonly categorized in quadrant IV (high severity of psychiatric disorders and substance use disorders). This likely does not reflect the population prevalence, where moderately severe depression (dysthymia) and alcohol use disorders occur at the highest rate ( 27 ), making the co-occurring disorders in quadrant III the most common ones by quadrant in the community. Nonetheless, in publicly funded systems and programs, the recognition that persons with severe mental illnesses also have severe substance use problems is now widely accepted ( 4 ). Evidence-based practices are available, and many states are engaged in significant implementation efforts for persons categorized in quadrants II and IV ( 4 , 16 ). The high utilization of inpatient and emergency services found in these data suggests that there is considerable room for progress. In community-based studies, use of these services is a proxy for a lack of therapeutic engagement and negative outcomes ( 28 ).
Another important finding is the high rate of persons with substance dependence disorders (quadrants III and IV). Classification in quadrant III was greater overall than either quadrant II or quadrant I. The consistent appearance of dependence-level disorders across all persons with co-occurring disorders—70.7% of persons with nonsevere mental illnesses and 73.0% of persons with severe mental illnesses—is remarkable. Thus 72.4% of Medicaid beneficiaries with co-occurring disorders met criteria for substance dependence disorders. Among persons with nonsevere mental illnesses, the proportion of individuals with dependence-level disorders (quadrant III) constitutes 2.4 times the number of persons with low severity of substance use (quadrant I) (19.8% versus 8.2%, respectively). And for persons with severe mental illnesses, the number with at least one dependence-level diagnosis (quadrant IV) is 2.6 times the number with substance use disorders (quadrant II).
Conclusions
These findings have policy and treatment service implications. For instance, even though substance use disorders are not disabilities that would, alone, qualify a person for Medicaid, state Medicaid programs pay indirectly (and directly) for their treatment. The earlier provision of treatments for persons with substance abuse-level conditions may reduce the number who progress to more severe dependence-level problems. Moreover, these findings suggest the advantages for Medicaid to include addiction treatment benefits and offer expanded coverage for persons with substance dependence disorders. At minimum, reimbursement policy should create incentives for mental health providers who offer integrated addiction treatment services ( 1 ) and addiction treatment providers who provide enhanced services for persons with severe psychiatric disorders ( 14 ).
Acknowledgments and disclosures
This research was supported by a grant from the Robert Wood Johnson Substance Abuse Policy Research Program (Clark) and by grant K23-DA-016574 from the National Institute on Drug Abuse (McGovern).
The authors report no competing interests.
1. Report to Congress on the Prevention and Treatment of Co-occurring Substance Abuse Disorders and Mental Disorders. Rockville, Md, Substance Abuse and Mental Health Services Administration, 2002Google Scholar
2. Improving the Quality of Health Care for Mental and Substance-Use Conditions: Quality Chasm Series. Washington, DC, Institute of Medicine, 2006Google Scholar
3. Substance Abuse Treatment for Persons With Co-occurring Disorders. Treatment Improvement Protocol Series 42. DHHS pub no SMA-05-3992. Rockville, Md, Center for Substance Abuse Treatment, 2005Google Scholar
4. Drake RE, Essock SM, Shaner A, et al: Implementing dual diagnosis services for clients with severe mental illness. Psychiatric Services 52:469–476, 2001Google Scholar
5. Pincus HA, Burnam MA, Magnabosco K, et al: State Activities to Improve Services and Systems of Care for Individuals With Co-occurring Mental and Addictive Disorders. RAND Working Paper WR-344-RW. Santa Monica, Calif, RAND, 2005Google Scholar
6. Gabriel RM, McFarland BH, Zani BG, et al: Differential access to services of co-occurring mental health and substance use disorders across managed care and fee for service system: a multi-state study. Presented at the Academy Health Annual Research Meeting, Seattle, Wash, June 25–27, 2006Google Scholar
7. Adelmann PK: Mental and substance use disorders among Medicaid recipients: prevalence estimates from two national surveys. Administration and Policy in Mental Health 31:111–129, 2003Google Scholar
8. Dickey B, Azeni H: Persons with dual diagnoses of substance abuse and major mental illness: their excess costs of psychiatric care. American Journal of Public Health 86:973–977, 1996Google Scholar
9. Buck JF: Spending for state mental health care. Psychiatric Services 52:1294, 2001Google Scholar
10. Coffey RM, Mark T, King E, et al: National Estimates of Expenditures for Substance Abuse Treatment, 1997. SAMHSA pub no SMA-01-3511. Rockville, Md, Center for Substance Abuse Treatment, Center for Mental Health Services, Feb 2001Google Scholar
11. Ridgely MS, Goldman HH, Willenbring M: Barriers to the care of persons with dual diagnoses: organizational and financing issues. Schizophrenia Bulletin 16:123–132, 1990Google Scholar
12. Grella CE, Gilmore J: Improving service delivery to the dually diagnosed in Los Angeles County. Journal of Substance Abuse Treatment 24:115–122, 2002Google Scholar
13. Cacciola JS, Alterman AI, McKay JR, et al: Psychiatric co-morbidity in patients with substance use disorders: do not forget axis II disorders. Psychiatric Annals 31:321–331, 2001Google Scholar
14. McGovern MP, Matzkin AL, Giard J: Assessing the dual diagnosis capability of addiction treatment services: the dual diagnosis capability in addiction treatment (DDCAT) index. Journal of Dual Diagnosis 3:111–123, 2007Google Scholar
15. Harris KM, Edlund MJ: Use of mental health care and substance abuse treatment among adults with co-occurring disorders. Psychiatric Services 56:954–959, 2005Google Scholar
16. Watkins KE, Hunter SB, Burnam MA, et al: Review of treatment recommendations for persons with a co-occurring affective or anxiety and substance use disorder. Psychiatric Services 56:913–926, 2005Google Scholar
17. National Dialogue on Co-occurring Mental Health and Substance Abuse Disorders. Alexandria, Va, Washington, DC, National Association of State Mental Health Program Directors, National Association of State Alcohol and Drug Abuse Directors, 1999Google Scholar
18. Ries R: Clinical treatment matching models for dually diagnosed patients. Psychiatric Clinics of North America 16:167–175, 1993Google Scholar
19. Ries R, Miller NS: Dual diagnosis: concept, diagnosis and treatment, in Current Psychiatric Therapy. Edited by Dunner DL. Philadelphia, Saunders, 1993Google Scholar
20. Rosenthal RN: Mental Illness/Chemical Addiction: A Guide to Emergency Services Assessment and Treatment. Albany, New York State Office of Mental Health, 1992Google Scholar
21. Pincus HA, Watkins K, Viamovska AM, et al: Models of care for co-occurring disorders. Final Draft Report to SAMHSA/CSAT. Santa Monica, Calif, RAND, 2006Google Scholar
22. McGovern MP, Xie H, Segal SR, et al: Addiction treatment services and co-occurring disorders: prevalence estimates, treatment practices and barriers. Journal of Substance Abuse Treatment 31:267–275, 2006Google Scholar
23. Clark RE, Samnaliev M, McGovern MP: Treatment for co-occurring mental and substance use disorders in five state Medicaid programs. Psychiatric Services 58:942–948, 2007Google Scholar
24. Lurie N, Popkin MK, Dysken M, et al: Accuracy of diagnoses of schizophrenia in Medicaid claims. Hospital and Community Psychiatry 43:69–71, 1992Google Scholar
25. Regier DA, Farmer ME, Rae DS, et al: Comorbidity of mental disorders with alcohol and other drug abuse: results from the epidemiologic catchment area (ECA) study. JAMA 264:2511–2518, 1990Google Scholar
26. Kessler RC, Chiu WT, Demler O, et al: Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry 62:617–627, 2005Google Scholar
27. Grant BF, Stinson FS, Dawson DA, et al: Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the national epidemiologic survey on alcohol and related conditions. Archives of General Psychiatry 61:807–816, 2004Google Scholar
28. Drake RE, Mueser KT, Brunette MF, et al: A review of treatments for people with severe mental illnesses and co-occurring substance use disorders. Psychiatric Rehabilitation Journal 27:360–374, 2004Google Scholar



