An Economic Evaluation of Telehealth Data Collection With Rural Populations
Health disparities between rural residents and urban or suburban residents in this country reflect substantial socioeconomic differences, poorer lifestyle practices, and decreased access to care ( 1 ). This is especially true of rurally dwelling American Indians and Alaska Natives, who are in greater jeopardy than other populations because of the geographic isolation and racial inequities in their daily lives ( 2 ). For example, there are measurably higher rates of morbidity and mortality among American Indian and Alaska Native reservations compared with other rural white and minority communities ( 3 , 4 ). However, the ability to monitor these trends, to obtain a deeper understanding of the root causes of specific disparities, and to investigate possible solutions is constrained by the challenges of conducting research in rural settings. Lack of infrastructure and the high cost of importing the resources necessary to conduct appropriate work impede the acquisition of this knowledge. One promising solution lies in telecommunication technologies—especially live interactive videoconferencing commonly known as telehealth—to address barriers to accessing health care and to ascertaining individual health status, function, and need.
With respect to patient care and health-related research, cost-related studies in telehealth are limited in empirical specificity and generalizability ( 5 , 6 , 7 ). The available studies fail to provide adequate detail for cost-analytic purposes ( 5 , 6 ); still, there remains a general sense among advocates that telepsychiatry is cost-effective, at least for providing remotely based care ( 8 , 9 ). Studies demonstrate savings to patients by eliminating travel to distant providers ( 10 , 11 ). Institutions save by eliminating provider travel ( 12 , 13 ) once they reach a critical level of teleconference activity within specified periods ( 14 , 15 , 16 , 17 ). Yet no studies have examined the direct cost of conducting research using telehealth nor have they explored how research via telehealth compares with in-person interviews. One of the difficulties in examining costs in telehealth and other such clinical modalities is that fixed and variable costs vary greatly among sites, making the generalizability of study results difficult.
This investigation compared the costs of telehealth and in-person structured clinical interviews through a study mounted in a rural American Indian tribal community some 600 miles from our facility. The purpose of this study was to compare direct costs of conducting structured clinical interviews with respondents in rural locations via real-time interactive videoconferencing (that is, telehealth) versus standard in-person methods. Previous work has demonstrated that psychiatric interviews can be administered in a reliable and valid manner by live, interactive teleconferencing ( 18 ). We hypothesized that telehealth would be less expensive than in-person interviews by eliminating travel time and reducing interviewer costs associated with missed appointments. We used a prospective test-retest design to evaluate our hypothesis.
Methods
Study description
This study is one component of a larger investigation that evaluated the use of the Structured Clinical Interview for DSM-III-R (SCID) to conduct psychiatric assessments by telehealth. Participants were administered a version of the SCID for DSM-III-R that was modified for use with American Indian populations for the American Indian Vietnam Veterans Project and further adapted in the American Indian Services Utilization, Psychiatric Epidemiology, Risk and Protective Factors Project ( 19 , 20 ). Results of the parent investigation were broken down to evaluate reliability, process, and economic outcomes.
The parent study used a prospective test-retest design. The researchers administered the SCID to American Indian veterans both face to face and via telehealth on two occasions within a two-week period. The study was conducted at the American Indian and Alaska Native Programs (AIANP) of the University of Colorado at Denver and Health Sciences Center in collaboration with a rural Northern Plains American Indian reservation. Participants were recruited from the local veteran population because they represented the best sample available on the reservation with a known prevalence of lifetime psychiatric disorders ( 19 ).
Colorado Multiple Institutional Review Board and tribal approvals were obtained before the study's initiation, and written informed consent was obtained from all participants. A power analysis indicated that 50 participants were needed for the purposes of the parent study. Seventy persons were approached; 60 (86%) agreed to participate, of whom 53 (76%) completed both interviews. All participants were men, with a mean (and median) age of 54 (range 46–71). Participants were administered a modified version of the SCID adapted for previous AIANP studies ( 20 ). Two psychiatrists, each experienced in working with American Indians and posttraumatic stress disorder (PTSD) in cross-cultural settings, were trained to administer the SCID.
Once participants enrolled, they were randomly assigned to one of two interview sequences: telehealth, defined as real-time, interactive videoconferencing followed by face-to-face interview, or in person, defined as a face-to-face interview followed by real-time interactive videoconferencing. Both assessments occurred within two weeks of the other. The in-person interview occurred at a private office in the community. The telehealth interview was conducted with the participant located at the tribal veterans' center and interviewers 600 miles distant at the AIANP in Denver. Interviews lasted between 80 and 90 minutes.
The psychiatrists conducted equal numbers of in-person and telehealth interviews during calendar year 2003, spanning 11 months, in four groups of approximately ten to 15 participants. The interviewing process began with the psychiatrists' interviewing between four and eight participants via telehealth from Denver. The psychiatrists then traveled to the community, stayed for a week, and conducted in-person SCIDs with the same respondents (telehealth interview before in-person interview). During this time the interviewers conducted between four and eight new respondent interviews in person; upon returning to Denver, they completed the remaining interviews via telehealth (in person before telehealth).
Cost data
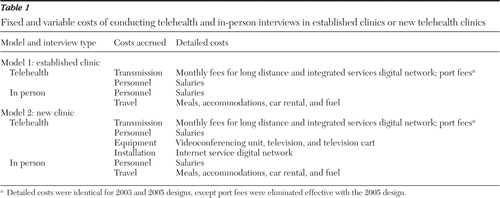
In this article we detail the costs accrued in our study so that others might use it as a guide or comparative source. This goal can be difficult to achieve, however, because organizations undoubtedly vary regarding the length of time that their telehealth clinics have operated and the types of costs that they accrue. For example, when this study was conducted, our program was already running an established tele-mental health clinic; thus the need to purchase and install videoconferencing equipment was unnecessary.
In order to address the expected cost differences between established and new telehealth clinics, we created two models. Model 1 (established telehealth clinics) was based on the costs that we accrued in this study and reflected the type of expenses that established telehealth programs might expect to pay. Model 2 (new telehealth clinics) detailed the expenses that developers of a startup telehealth clinic are likely to experience. We collected data during the course of the study. For cost data not acquired during our investigation (that is, equipment and installation charges), we used pricing information from a recent purchase for similar goods and services.
Models for established telehealth clinics and new telehealth clinics were further subdivided to examine the actual configuration costs accrued during the study (2003 design) as well as the telehealth costs under our current telecommunications configuration (2005 design). Since the conclusion of the study in 2003, AIANP videoconferencing transmission rates have decreased considerably because of internal and market forces. We installed a direct integrated services digital network (ISDN) connection that resulted in the elimination of port fees; port fees were, to some extent, an artifact of the academic setting in which the telehealth base operated, and more competitive long distance carriers made it possible to contract for a drastically reduced long-distance rate. The 2005 design enables more direct comparison with clinics that do not incur port fees ( 11 , 14 , 16 ).
In summary, we used two models to compare telehealth and in-person interviews. Each model considered two systems—designed in 2003 and 2005. Model 1 looked at costs for established clinics, and model 2 looked at costs for new clinics.
Model 1: established telehealth clinic variable costs
Transmission. The transmission costs of the 2003 design included long-distance charges, port fees, and ISDN line fees for one site. These costs totaled $12,888 (.28–.32 cents per minute per line), $7,889 ($60 per hour charge) and $2,761 total ($250 per month), respectively. The transmission costs of the 2005 design consisted of reduced long-distance charges and ISDN monthly line fees for two sites. The total of these charges equaled $4,098 and $5,521, respectively.
Personnel. Personnel charges consisted of the psychiatrists' time for conducting interviews, calculated in hours, and included travel time (for in-person interviews). Salary figures were gathered from two public sources for medical labor costs: the American Medical Group Association and the U.S. Department of Labor ( 21 ). Annual salaries for psychiatrists from these sources were averaged (mean±SD equal to $153,338±$19,852) and converted to an hourly wage rate ($73.72 per hour). To create a range of costs based on salary variations, we computed high and low estimates of personnel costs that were based on the figures from these sources (ranging from $167,375 to $139,300).
Salaries. Salary estimates also were generated for other mental health professionals capable of conducting the SCID, such as psychologists and social workers. For doctorate- and master's-level psychologists, salary estimates were obtained from American Psychological Association data and averaged over the incomes provided for entry-level and non-entry-level workers ( 22 ). We generated estimates of $25.53 per hour for doctorate-level psychologists and $17.50 per hour for master's-level psychologists. Salary estimates for social workers were obtained from the U.S. Department of Labor and the Human Resources Consulting Company figures ( 23 , 24 ), and analysis yielded an estimate of $16.83 per hour.
Travel. Travel costs included car rental, fuel, lodging, and meals for two psychiatrists.
Model 2: new telehealth clinic costs
Fixed costs. We included equipment and installation charges for organizations establishing a new telehealth clinic. These costs included two Polycom Viewstation videoconferencing units and two television monitors and carts. For the 2003 design, we included the price of installing three ISDN lines (384 kbps) at one site, whereas for the 2005 design we included the price of installing three ISDN lines at two sites. Depreciation was calculated against both the equipment and installation charges over four years according to a straight-line method at a market rate of 25%.
Variable costs. We anticipated that the variable costs for a new telehealth service (transmission, personnel, and travel expenses) would remain the same. Variable costs were computed as described in model 1. Table 1 details the costs used for both models in our study.
 |
Results
Model 1: established telehealth clinic
Table 2 presents direct costs for telehealth and in-person interviews under the 2003 design and variations on the 2005 design. The top section of Table 2 shows costs for an established telehealth clinic. Personnel costs revealed that telehealth interviews took 131.5 personnel hours. In-person interviews, including travel time, required 352.0 personnel hours. Total costs for telehealth interviews were $33,230. For in-person interviews, the bottom section of Table 2 , although three times as many clinician hours were expended, total costs were slightly lower, at $31,465.
 |
The 2005 design cost scenarios favored an established telehealth over in-person interviews at a range of personnel costs, with savings ranging from $10,000 to $13,000. Transmission charges were constant across each scenario and reflected the reduced long-distance rates, direct ISDN lines, and the absence of port fees.
Model 2: start-up telehealth clinic
Table 2 presents direct costs for telehealth and in-person interviews under the 2003 design and variations on the 2005 design; the midsection of this table shows costs for new telehealth clinics (model 2). The variable costs (personnel, transmission, and travel) remained the same as in model 1, with the addition of the fixed costs of equipment and installation, which were depreciated over four years (depreciation would occur only for ongoing telehealth activity).
The 2003 design costs for telehealth interviews totaled $37,438. Of this, $4,208 accounted for equipment and installation charges. With these additional videoconferencing charges, the difference in overall costs between telehealth and in-person interviews rose to $5,973, favoring in-person interviews. The 2005 design cost scenarios favored telehealth over in-person interviews. On the basis of high, average, and low salary ranges, telehealth was less expensive than in-person interviewing, with savings ranging from about $6,400 to about $9,400.
Personnel cost differences
Table 3 extends the 2005 design scenario for established clinics by varying direct costs by interview modality with personnel training and associated wages. As previously discussed, telehealth interviews using psychiatrists as interviewers were cheaper than in-person interviews; this pattern also held for doctorate-level psychologists. For lower wage-earning occupations (such as master's-level psychologists and social workers), in-person interviews were less expensive to conduct, although we saw a savings of less than $500. Because we held the cost of transmission and travel constant among all scenarios, the difference in savings in Table 3 is entirely attributable to salary variations.
 |
Discussion
This is the first empirical study to measure and compare the costs of conducting research using telehealth with reservation-based American Indians. For actual costs incurred in 2003, the telehealth interviews cost approximately $1,700 more to conduct than in-person interviews. One of the major contributing factors to this difference was the port fees, which were, to our knowledge, unique to the University of Colorado and have not been calculated or cited in previous economic studies in telehealth ( 13 , 14 , 16 , 25 ). When our videoconferencing configuration changed and port fees were eliminated, telehealth interviews generated a savings of $12,153 over in-person interviews.
Market change affected these cost calculations as well. Because the research project spanned almost a year, the market price of long-distance communication over ISDN lines dropped twice and then once again after the conclusion of the study. Such rate decreases for ISDN lines are considerable; had the study been conducted a year later, we would have saved nearly $9,000 in long-distance costs alone. Transmission costs are expected to decrease further as competition between ISDN and Internet protocol-based videoconferencing compete for market share ( 26 ). As equipment and ISDN installation are figured into the equation (a situation most new clinics will face), telehealth costs increase. However, because these purchases represent fixed costs, the increased use of the videoconferencing minimizes the total price burden of these expenditures over time.
The SCID is also designed for nonphysician interviewers; Table 3 shows scenarios with interviewers of different professional training. In these scenarios, telehealth was more expensive for salaried professionals earning less than $39,000 under an established clinic. This has obvious implications for researchers who are able to circumvent equipment and installation costs by pooling resources. Possible ways to reduce or avoid such costs include conducting research over shared networks, partnering with existing networks, or reducing unit interview costs by conducting multiple studies over the same telehealth connection. In addition, research projects with a greater volume of telehealth activity, higher travel costs, and higher budgets could realize economies of scale. Evidence of economies of scale in telehealth interviews has been documented in the few existing studies and shows that higher volume increases the cost savings for telehealth networks ( 16 , 17 , 25 ).
Besides the potential benefits to direct costs, telehealth research has other, less tangible benefits that are more difficult to value in monetary terms. Telehealth reduces the need for travel and increases the ease and convenience for study personnel. In this investigation, the interviewers spent a total of one month in the field completing in-person interviews. This complicated scheduling and created significant inconvenience for the interviewers. It is difficult to recruit trained health professionals to rural communities ( 27 ), which may provide one explanation of why less research is conducted in rural areas. Also, study personnel found the telehealth interviews were logistically easier to arrange, with reduced costs of failure. If a participant missed a telehealth interview, it could easily be rescheduled for a future date, whereas missed in-person interviews not rescheduled while the interviewer visited the remote location could not be completed, and personnel time in the field was lost. Finally, in addition to the logistical and personnel benefits of telehealth research, videoconferencing provides and facilitates greater contact, communication, and collaboration between the end site and the research organization. For example, the AIANP uses videoconferencing to provide supervision of field research from Denver to its remote and rural sites. So even if the actual costs of telehealth and in-person interviews are equivalent, telehealth interviews may be more cost-beneficial.
There are limitations to this economic evaluation. First, because this is the first study of its type, the generalizability of the results beyond the field of tele-mental health and the study population (male Northern Plains American Indian veterans) is unknown. Second, this study focused only on the telehealth modality of live interactive videoconferencing and is only suggestive for other telehealth applications, such as via e-mail, telephone, and Web-based research. Third, the argument for using cost as the basis for using telehealth over in-person interviews assumed that the scientific validity, reliability, and participant satisfaction was not negatively impacted ( 18 ). In order for telehealth research to be successfully conducted, the impact of videoconferencing on the administration, the performance of the measures used, and the impact on the process with the study population must be understood. This last point is an ongoing aspect of our work.
Conclusions
Despite its limitations, this study represents a critical first step in beginning to understand the economic implications of conducting telehealth-facilitated research. Future studies should replicate this one to increase empirical evidence on the relative costs of telehealth research, the feasibility of extending tele-psychiatric research to other medical applications for telehealth, and economic evaluations of the use of other telehealth modalities (such as via e-mail or Web) for research. Research, as well as medical practice, using videoconferencing holds the potential to increase efficiency and decrease the cost of contact with rural, remote, and underserved populations. Telehealth-facilitated research promises to help reduce health disparities with rural and underserved populations.
Acknowledgments and disclosures
The study was supported by grant 1F32-MH-63527-01A1 from the National Institute of Mental Health and by grant P60-MD-000507 from the National Center for Minority Health and Health Disparities. The opinions expressed in this article are those of the authors and do not necessarily reflect the views of the Indian Health Service. The grant sponsors played no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
The authors report no competing interests.
1. Eberhardt MS, Pamuk ER: The importance of place of residence: examining health in rural and nonrural areas. American Journal of Public Health 94:1682–1686, 2004Google Scholar
2. Probst JC, Moore CG, Glover SH, et al: Person and place: the compounding effects of race/ethnicity and rurality on health. American Journal of Public Health 94:1695–1703, 2004Google Scholar
3. Centers for Disease Control and Prevention: Health status of American Indians compared with other racial/ethnic minority populations—selected states, 2001–2002. Morbidity and Mortality Weekly Report 52:1148–1152, 2003Google Scholar
4. Denny CH, Holtzman D, Cobb N: Surveillance for health behaviors of American Indians and Alaska Natives: findings from the Behavioral Risk Factor Surveillance System, 1997–2000. Surveillance Summaries: Morbidity and Mortality Weekly Report. Surveillance Summaries 52:1–13, 2003Google Scholar
5. Whitten PS, Mair FS, Haycox A, et al: Systematic review of cost effectiveness studies of telemedicine interventions. BMJ 324:1434–1437, 2002Google Scholar
6. Hailey D, Roine R, Ohinmaa A: Systematic review of evidence for the benefits of telemedicine. Journal of Telemedicine and Telecare 8(suppl 1):1–30, 2002Google Scholar
7. Hakansson S, Gavelin C: What do we really know about the cost-effectiveness of telemedicine? Journal of Telemedicine and Telecare 6(suppl 1):S133–S136, 2000Google Scholar
8. Hyler SE, Gangure DP: A review of the costs of telepsychiatry. Psychiatric Services 54:976–980, 2003Google Scholar
9. Monnier J, Knapp RG, Frueh BC: Recent advances in telepsychiatry: an updated review. Psychiatric Services 54:1604–1609, 2003Google Scholar
10. Bynum AB, Irwin CA, Cranford CO, et al: The impact of telemedicine on patients' cost savings: some preliminary findings. Telemedicine Journal and E-Health 9:361–367, 2003Google Scholar
11. Trott P, Blignault I: Cost evaluation of a telepsychiatry service in northern Queensland. Journal of Telemedicine and Telecare 4(suppl 1):66–68, 1998Google Scholar
12. Simpson J, Doze S, Urness D, et al: Telepsychiatry as a routine service—the perspective of the patient. Journal of Telemedicine and Telecare 7:155–160, 2001Google Scholar
13. Tang WK, Chiu H, Woo J, et al: Telepsychiatry in psychogeriatric service: a pilot study. International Journal of Geriatric Psychiatry 16:88–93, 2001Google Scholar
14. Elford DR, White H, St John K, et al: A prospective satisfaction study and cost analysis of a pilot child telepsychiatry service in Newfoundland. Journal of Telemedicine and Telecare 7:73–81, 2001Google Scholar
15. Kennedy C, Yellowlees P: A community-based approach to evaluation of health outcomes and costs for telepsychiatry in a rural population: preliminary results. Journal of Telemedicine and Telecare 6(suppl 1): S155–S157, 2000Google Scholar
16. Doze S, Simpson J, Hailey D, et al: Evaluation of a telepsychiatry pilot project. Journal of Telemedicine and Telecare 5:38–46, 1999Google Scholar
17. Simpson J, Doze S, Urness D, et al: Evaluation of a routine telepsychiatry service. Journal of Telemedicine and Telecare 7:90–98, 2001Google Scholar
18. Shore JH, Savin D, Orton H, et al: Diagnostic reliability of telepsychiatry in American Indian veterans. American Journal of Psychiatry 164:115–118, 2007Google Scholar
19. Matsunaga Vietnam Veterans Project. White River Junction, Vt, National Center for Post-Traumatic Stress Disorder and the National Center for American Indian and Alaska Native Mental Health Research, 1996Google Scholar
20. Beals J, Novins DK, Spicer P, et al: Challenges in operationalizing the DSM-IV clinical significance criterion. Archives of General Psychiatry, 61:1197–1207, 2004Google Scholar
21. 2004 Medical Group Compensation and Financial Survey. Alexandria, Va, American Medical Group Association, 2004Google Scholar
22. Singleton D, Tate A, Randall G: Salaries in Psychology 2001: Report of the 2001 APA Salary Survey. Washington, DC, American Psychological Association, 2003Google Scholar
23. Occupational Employment and Wages, May 2003. Washington, DC, US Department of Labor, 2004Google Scholar
24. Wageweb Health Care: National Averages, vol 2005. Richmond, Va, Human Resources Programs Development and Improvement, 2003Google Scholar
25. Moser PL, Stadlmann S, Heinzle G, et al: A cost comparison of telepathology and a visiting pathologist service. Journal of Telemedicine and Telecare 9:200–203, 2003Google Scholar
26. Grigsby B: 4th annual telemedicine program review: part 2. United States. Telemedicine Today 5:30–38, 1997Google Scholar
27. Felix H, Shepherd J, Stewart MK: Recruitment of rural health care providers: a regional recruiter strategy. Journal of Rural Health 19(suppl):340–346, 2003Google Scholar



