Unintended Consequences of Regionalizing Specialized VA Addiction Services
Driven primarily by budgetary reforms, the Department of Veterans Affairs (VA) began shifting services in 1995 from hospital-based care to outpatient-based care. Then-Under Secretary for Health Kenneth Kizer aimed to decrease per-patient expenditures by 30% while increasing the number of veterans served by 20% ( 1 ). Subsequently, VA addiction services, consisting of traditional inpatient treatment models located at most parent VA facilities, were reorganized into predominantly outpatient and residential programs. As a result of this transition from inpatient care, VA spending on specialized addiction services fell from $360 million in 1995 (2.4% of total VA health care spending that year) to $226 million in 2000 (1.2% of that year's total) ( 2 ).
With the shift to outpatient care, the VA was reorganized into 22 Veterans Integrated Service Networks (VISNs). The intent was that each network would offer a full continuum of specialized medical, surgical, psychiatric, and substance abuse care, the components of which would be accessible to all eligible veterans within the VISN boundaries. Most facilities within each VISN retained general medical inpatient capabilities, including provision of alcohol and drug detoxification services; however, most inpatient specialized addiction (rehabilitation) services were closed or converted to outpatient or residential services ( 3 ). The few remaining inpatient programs for specialized addiction services were located in larger urban centers within selected VISNs. Of the 70 inpatient programs available nationwide in 1997, only 21 remained in 2000, and all but 15 programs were eliminated by 2003 ( 4 ). In New York State, there were eight VA facilities where veterans could access specialized inpatient care in 1997, but by 2000 only two inpatient rehabilitation programs remained.
Although residential programs and intensive outpatient programs were planned to be established and standard outpatient services expanded to fill treatment gaps at lower cost, overall the VA saw a 19% reduction in addiction treatment programs ( 5 ). Between 1997 and 2000 eight new residential programs were established nationwide, but 12 intensive outpatient programs and six standard outpatient programs were lost ( 5 ). New York gained four residential programs but lost three intensive outpatient programs and one standard outpatient program over the same period ( 5 ). As the number and intensity of programs declined, the severity of problems among veterans seeking treatment increased and waiting lists expanded ( 5 ).
Although remaining services are theoretically accessible to all eligible veterans, for this study we hypothesized that veterans who live in rural settings, who would likely experience greater travel distances to remaining facilities with specialized inpatient addiction services, may have greater difficulty accessing these services because of potential travel-time barriers and a lower "nonlocal" priority compared with veterans living near these facilities. Having previously developed a unique data set that included all VA and non-VA hospitalizations for New York veterans between 1998 and 2000 ( 6 ), we were able to assess whether rural veterans altered their use of VA nonspecialized (detoxification) inpatient addiction services, specialized (rehabilitation) inpatient addiction services, or both. We also examined whether rural veterans or urban veterans increased their use of non-VA inpatient addiction services to compensate for the loss of available VA inpatient addiction services. In addition, we examined the characteristics of VA enrollees who accessed addiction and nonaddiction inpatient services in VA facilities and non-VA facilities and across rural and urban settings.
Methods
We conducted a retrospective cohort study of New York veterans who were enrolled in the VA health care system and admitted to either VA facilities or non-VA facilities for inpatient drug or alcohol detoxification or rehabilitation in New York State during years in which the data for both VA services and non-VA services were available: 1998 through 2000. We linked data from multiple sources to address three questions: Where did VA patients access nonspecialized (detoxification) and specialized (rehabilitation) inpatient addiction services—in VA or non-VA facilities? Did veterans' use of either system change over the three-year interval as the VA reduced budgets and regionalized addiction care? Did rural veterans and urban veterans differ in their use of VA and non-VA inpatient addiction services? This study was approved by Dartmouth Medical School's Committee for the Protection of Human Subjects.
Identification of patients admitted to a VA facility
From VA administrative databases, we identified 353,570 veterans who were enrolled in the VA system and were residents of New York State at any time between 1998 and 2000. We defined enrollment on the basis of two criteria: being listed in the VA enrollment file and using VA health services in the prior three years. These criteria were adopted for two reasons. First, the VA enrollment file identifies patients for whom the VA has an obligation to provide a medical benefits package ( 7 ). Second, service utilization within three years "vests" patients for the purposes of administering the Veterans Equitable Resource Allocation system. Both enrollment and vesting are used to define the VA service population or "covered lives" for whom the VA has a potential medical benefits liability. Our criteria for enrolled patients replicate methods used previously ( 6 , 8 , 9 ).
Identification of addiction admissions
We used ICD-9-CM procedure codes to identify admissions in VA facilities and non-VA facilities for alcohol or drug detoxification only (detoxification only— ICD-9-CM procedure codes 94.62, 94.65, and 94.68) and alcohol or drug rehabilitation with or without detoxification (rehabilitation— ICD-9-CM codes 94.60, 94.61, 94.63. 94.66, 94.67, and 94.69).
VA use. To determine whether patients admitted to a VA facility accessed inpatient addiction services in New York's VA system, we used ICD-9-CM codes from the VA's patient treatment file to identify patients who obtained detoxification or rehabilitation services in any VA facilities that provide these services in New York.
Non-VA use. We obtained information on enrolled veterans' non-VA admissions from New York's Statewide Planning and Research Cooperative System (SPARCS) data set, a system that collects discharge information, including ICD-9-CM procedure codes and payer information, from all non-VA New York hospitals. The SPARCS data set identifies patients by using a combination of letters from patients' first and last names and digits from their Social Security numbers. We linked the SPARCS and VA data sets by obtaining the same data elements from the VA enrollment file, mimicking the SPARCS algorithm, and using the generated unique identifier to capture information on non-VA admissions. We used ICD-9-CM procedure codes from the SPARCS data set to identify veterans who obtained inpatient detoxification only or who received rehabilitation in any non-VA facilities that provide these services in New York.
Defining rural and urban service populations
To classify veterans as rural or urban, we matched their ZIP codes to Rural-Urban Commuting Area (RUCA) codes that were developed by the Health Resources and Service Administration's Federal Office of Rural Health Policy, the Department of Agriculture's Economic Research Service, and the WWAMI [Washington, Wyoming, Alaska, Montana, and Idaho] Rural Health Research Center at the University of Washington School of Medicine ( 10 ). We used the Washington State Department of Health's RUCA consolidation system ( 11 ) to classify and compare veterans who lived in urban settings (areas of 500,000 persons or more, corresponding with U.S. Bureau of the Census-defined urbanized areas; RUCA code 1.0) to those who lived in rural settings (small towns with populations below 10,000 and isolated rural areas; RUCA codes 7.0, 7.3, 7.4, 8.0, 8.3, 8.4, 9.0, 9.1, 9.2, 10.0, 10.3, 10.4, and 10.5).
Statistical analysis
For each system of care (VA or non-VA), level of care (detoxification only or rehabilitation), and patient residence (urban or rural), we calculated average annual admissions per unique enrolled veteran by dividing the overall number of admissions by the number of unique VA enrollees in New York State applicable to each analysis. Using chi square analysis, we tested for the relative reliance on VA versus non-VA addiction and nonaddiction inpatient services for rural and urban veterans by individual year and all years combined, and we tested for rural and urban differences in annual admission rates for detoxification only or rehabilitation at either non-VA or VA hospitals across years 1998–2000. Using 1998 as the reference year, we used the standard dichotomous variable-dichotomous endpoint formula to calculate odds ratios with 95% confidence intervals for each admission category (detoxification or rehabilitation) and system of care (VA or non-VA) to estimate temporal trends in admissions rates.
Results
As shown in Table 1 and Table 2 , the correlates of residence and system of care were different between patients admitted for inpatient addiction treatment and those admitted for nonaddiction inpatient services. Among veterans hospitalized for care other than addiction treatment, private-sector patients were older than patients admitted to a VA facility, rural residents were more likely to be white, regardless of system of care, and private-sector patients were more likely to be white, regardless of rural or urban residence (p<.001 for all). In addition, patients admitted to a non-VA facility, either urban or rural, were more likely to be enrolled in Medicare, and rural VA patients were more likely to be enrolled in Medicare than their urban counterparts (p<.001 for all). Finally, patients admitted to a VA facility, either urban or rural, were more likely to have a service-connected disability, and rural patients admitted to a non-VA facility were less likely than their urban counterparts to have a service-connected disability (p<.001 for all).
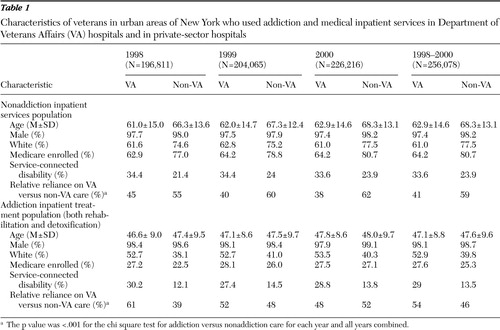 |
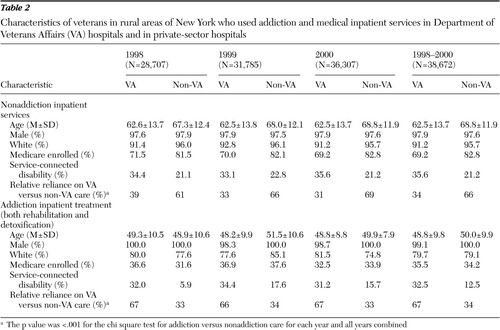 |
Table 1 and Table 2 also show that among patients admitted for addiction treatment, patients admitted to a non-VA facility were older than those admitted to a VA facility (p<.001), but rural patients admitted to a VA facility were older than urban patients admitted to a VA facility (p<.001). They also show that although rural residents, compared with urban residents, admitted for inpatient addiction treatment were more likely to be white, regardless of system of care, patients admitted to a non-VA facility were less likely to be white, regardless of residence (p<.001 for all). In addition, the tables show that among patients admitted for inpatient addiction treatment, rural patients were more likely to be enrolled in Medicare, regardless of system of care, but both urban patients and rural patients admitted to a non-VA facility were less likely to be enrolled in Medicare (p<.001 for all). Finally, the tables show that both urban patients and rural patients admitted to a VA facility for addiction treatment were more likely than those admitted to a non-VA facility to have a service-connected disability (have military-related disabilities), but rural patients admitted to a VA facility were more likely to have a service-connected disability than their urban counterparts (p<.001 for all).
Regardless of rural or urban residence, VA enrollees who were hospitalized for nonaddiction treatment received it in VA facilities less often than in non-VA facilities. In contrast, VA enrollees received addiction treatment services more often in VA facilities than in non-VA facilities (p<.001 for the chi square test of relative reliance on VA for addiction versus nonaddiction care for all years individually and combined). Urban veterans in New York used inpatient addiction services (detoxification only, rehabilitation, or both) in both VA facilities and non-VA facilities at higher rates than rural veterans did (p<.001 for all). Although less likely to receive addiction treatment, rural veterans obtained a higher proportion of these services from VA facilities. Over the three years, VA facilities provided 67% of rural veterans' addiction treatment compared with 54% of urban veterans' addiction treatment (p< .001). Rural veterans' relative reliance on addiction care in VA facilities remained stable from 1998 to 2000, whereas urban veterans used increasingly more addiction care in non-VA facilities.
As shown in Table 3 , admission rates to VA facilities for inpatient addiction services fell for both rural and urban VA enrollees from 1998 to 2000. Specifically, in 1998 detoxification admissions in VA facilities averaged 13 per 1,000 enrolled urban veterans and nine per 1,000 enrolled rural veterans, whereas in 2000 they averaged nine per 1,000 for urban veterans and six per 1,000 for rural veterans. Rehabilitation admissions to VA hospitals fell from six per 1,000 urban veterans and two per 1,000 rural veterans in 1998 to two per 1,000 urban veterans and .3 per 1,000 rural veterans in year 2000.
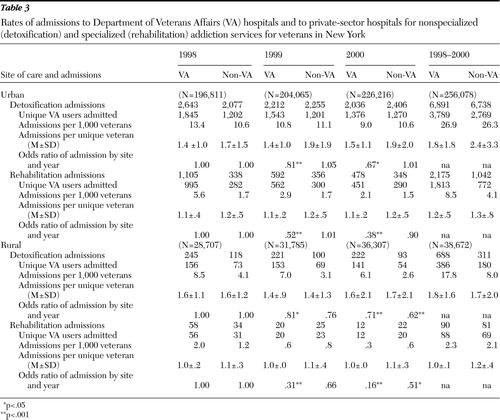 |
Rates of admission for addiction treatment to VA facilities exceeded those to non-VA facilities in every year and regardless of patient residence (with the exceptions of detoxification admissions in years 1999 and 2000 for urban VA enrollees) ( Table 3 ).
Urban veterans' admission rates to non-VA facilities for addiction services remained stable throughout the three years, at 11 per 1,000 for detoxification only and two per 1,000 for rehabilitation. Rural veterans' admission rates fell, however, from four per 1,000 for detoxification only and 1.2 per 1,000 for rehabilitation admissions in 1998 to three per 1,000 for detoxification only and .6 per 1,000 for rehabilitation admissions in 2000 ( Table 3 ).
Compared with 1998 levels, odds ratios of accessing the VA for detoxification fell to approximately .80 in 1999 and approximately .65 in 2000 (both p<.01) for both rural and urban veterans. Odds ratios for urban veterans' use of detoxification services in non-VA facilities remained fairly constant from 1998 to 2000, but odds ratios for rural veterans' use of detoxification services in non-VA facilities fell to .76 of 1998 levels in 1999 (not significant) and .62 in 2000 (p<.001). Compared with 1998 levels, odds ratios for admission to VA hospitals for substance abuse rehabilitation fell to .52 in 1999 and .38 in 2000 for urban residents, but for rural residents they fell more, to .31 and .16, respectively (all p<.001). Odds ratios for rehabilitation admission to non-VA facilities changed little for urban veterans, and the change was not significant (1.01 in 1999 and .90 in 2000) but fell substantially for rural veterans, to .66 in 1999 (not significant) and .51 in 2000 (p<.05) ( Table 3 ).
Discussion
After VA's reorganization in the mid-1990s, both rural veterans and urban veterans in New York reduced their use of inpatient nonspecialized and specialized addiction services. However, several trends suggest that rural New York veterans disproportionately felt the effects of addiction service cutbacks and regionalization. Since 1998 use of inpatient VA addiction services, particularly specialized services, declined more dramatically for rural veterans than for urban veterans.
The disproportionate burden that reductions imposed on rural veterans can be explained simply. Because nonspecialized inpatient addiction care (detoxification) can be accomplished on most general medical or psychiatric wards, one would anticipate that the reduction in general medical inpatient beds would affect rural VA facilities and urban VA facilities similarly. But although urban veterans appeared to compensate for loss of VA detoxification services somewhat by increasing their use of non-VA detoxification services, the same was not true of rural veterans. In fact, from 1998 to 2000 the number of non-VA hospitals in New York providing detoxification in urban areas fell 4% (from 98 to 94 hospitals), while hospitals providing detoxification in rural areas fell 25% (from 40 to 30 hospitals); hence, rural veterans experienced the additional reduction in non-VA detoxification sites during the study period.
There are three potential reasons why rural veterans disproportionately suffered from reductions in specialized inpatient VA addiction treatment (rehabilitation). First, although regionalized services were meant to be accessible to all veterans within a network, facilities may prioritize veterans from their own catchment area or local referral sources. Second, distance to care is a barrier to accessing health care services ( 12 , 13 , 14 ); regionalization to urban sites undoubtedly increased driving time for rural veterans. Third, lack of public transportation in rural areas further restricts access to treatment, over and above barriers based on distance alone ( 15 ). These distance and transportation barriers are further compounded for patients with substance use disorders, who commonly lose driver's licensure and lack the means to transport themselves to a distant facility.
Although the VA intended for the additional outpatient and residential services to replace lost inpatient services, these are likely to be inadequate substitutes, especially for rural veterans. Guideline-concordant outpatient addiction treatment requires multiple visits. Because fewer visits are likely to be completed by patients living at greater distances from care ( 16 ), rural veterans are less likely to receive the required number of addiction visits defining guideline-concordant treatment.
Our study has several limitations. Our analysis focused on inpatient care only. Lack of outpatient, residential, and domiciliary data limits our ability to make rural-urban comparisons about overall addiction care. However, similar comparison of outpatient addiction treatment would be virtually impossible given the absence of a uniform collection methodology for non-VA outpatient treatment. Acknowledging this limitation, we feel our findings are useful in describing an important aspect of addiction treatment for rural and urban veterans.
Second, our analysis is limited to VA users who live within the confines of New York State and who used New York State hospitals. Rural or urban VA users in New York may not be representative of all rural or urban VA users nationwide. Likewise, administrative and clinical changes to inpatient addiction services within New York VA facilities at the time studied may not reflect those of VA facilities in other regions.
Third, we were unable to assess rural-urban differences in substance use disorder prevalence or to track changes in prevalence among VA users for the years examined. The overall higher use of inpatient addiction services by urban veterans may be warranted. A large national survey of veterans from the same period suggests that urban veterans have a higher prevalence of alcohol use disorder compared with rural veterans ( 17 ). Although the sample used in a telephone health survey of residents of six Southern states was perhaps not similar to the New York veteran population examined herein, the survey likewise found lower rates of at-risk drinking among rural residents compared with their urban counterparts ( 18 ). Likewise, the 2001 National Household Survey on Drug Abuse found higher rates of both alcohol abuse and illicit drug abuse among metropolitan respondents compared with nonmetropolitan respondents ( 19 ). It is possible that the observed reduction in admission rates for inpatient addiction services in New York from 1998 to 2000 merely reflects a decline in need for those services. However, others have shown that veterans' needs for addiction services remained high from 1994 to 2001, making this explanation unlikely ( 20 ).
Fourth, we were unable to assess potentially independent effects of geographic variation in admission rates on our findings. Geographic variation in medical, surgical, and psychiatric services has been well described in the private sector and is thought to be mediated by regional practice patterns and supplier-induced demand ( 21 , 22 ). Theoretically, the VA should be less prone to geographic variation given its centralized planning and lack of economic incentives; however, variation in admission rates and length of stay has been described in the VA as well ( 23 , 24 , 25 ). Given that our sample reflects a relatively small geographic region, all predominantly controlled by two VISN authorities, and assuming any variations remained stable over the period examined, geographic variation alone is unlikely to explain the differences we found.
Finally, as with all administrative data sets, our data may be incomplete or include incorrectly coded events. However, other studies using this database found that 98% of events that were captured in this data set were also captured in a clinical registry, and no events that occurred outside of New York were captured in the New York data set ( 6 , 26 ).
Our findings suggest that rural veterans have disproportionately suffered from reductions in addiction services. Perhaps recognizing that its reductions in addiction services in the 1990s were too extreme, the VA allocated $9.5 million for addiction treatment expansion through the Veterans Millennium Health Care and Benefits Act of 2000 (Public Law 106–117). Although this additional funding may have slowed further reductions, it did not reverse the trend. The number of veterans with substance use disorders increased by 31% between 2000 and 2003, while the average number of veterans treated in VA addiction services decreased by 8% over the same period ( 4 ). In April 2003 American Psychiatric Association Trustee Joseph English, M.D., urged the House VA-HUD [Department of Veterans Affairs and Housing and Urban Development] Appropriations Subcommittee to include an additional $2 billion to restore mental health and substance abuse services and to correct "significant inequalities in access and quality of care of specialized treatment service" ( 27 ). In order to correct these disparities, VA medical centers that serve rural veterans should be given funding priority with regard to reestablishing addiction services.
Conclusions
Our study suggests that the VA's well-intended plan to cut costs while serving more veterans resulted in the unintended consequence of reducing access to VA inpatient addiction treatment. This was especially true for rural veterans, who experienced concurrent reductions in access to these services in non-VA facilities. Although we focused on the plight of a select group—rural veterans seeking inpatient addiction treatment in the era of VA downsizing—our study is relevant to overall rural health policy in two ways. First, research is lacking on the impact of changes in health system structures on rural-urban disparities in access to health care in general U.S. populations. Our study suggests that examining combined VA and private-sector data sets can shed light on differences in rural and urban consumer responses to changes in health systems policies. Second, the VA is a large, highly coordinated system of care that is less influenced by economic incentives that drive most private-sector health care systems. The access disparities that exist in the VA may be magnified in smaller health care systems for which locating treatments in less populous areas may lack political appeal or result in loss of revenue. Our results advise health care policy makers to consider the needs of identified vulnerable populations before policies are implemented and to monitor those needs afterward to avoid creating unintended inequities in access to care.
Acknowledgments and disclosures
The authors report no competing interests.
1. Journey of Change. Washington DC, Department of Veterans Affairs, Veterans Health Administration, 1997Google Scholar
2. Cost Distribution Report Tabulation Fiscal Years 1993–2003. Department of Veterans Affairs, Health Economics Resource Center, 2006. Available at www.herc.research.va.gov/data/cdr.aspGoogle Scholar
3. Humphreys K, Huebsch PD, Moos RH, et al: The transformation of the Veterans Affairs Substance Abuse Treatment System. Psychiatric Services 50:1399–1401, 1999Google Scholar
4. Tracy W, Trafton JA, Humphreys K: The Department of Veterans Affairs Substance Abuse Treatment System: Results of the 2003 Drug and Alcohol Program Survey. Palo Alto, Calif, Program Evaluation and Resource Center, 2004Google Scholar
5. Humphreys K, Horst D: The Department of Veterans Affairs Substance Abuse Treatment System: Results of the 2000 Drug and Alcohol Program Survey. Palo Alto, Calif, Program Evaluation and Resource Center, 2001Google Scholar
6. Weeks WB, Bazos DA, Bott DM, et al: New York's statistical model accurately predicts mortality risk for veterans who obtain private sector CABG. Health Services Research 40:1186–1196, 2005Google Scholar
7. Enrollment—provision of hospital and outpatient care to veterans—VA: proposed rule. Federal Register 63:37299–37307, 1998Google Scholar
8. Weeks WB, Bott DM, Lamkin RP, et al: Veterans Health Administration and Medicare outpatient health care utilization by older rural and urban New England veterans. Journal of Rural Health 21:65–69, 2005Google Scholar
9. Weeks WB, Mahar PJ, Wright SM: Utilization of VA and Medicare services by Medicare-eligible veterans in northern New England: the impact of additional access points in a rural setting. Journal of Health Care Management 50:95–106, 2005Google Scholar
10. Rural Urban Commuting Area Code, Vol 2004. Washington, DC, US Department of Agriculture, Economic Research Service, 2001Google Scholar
11. ZIP Code RUCA approximation methodology, Vol 2004. Washington, DC, WWMAI [Washington, Wyoming, Alaska, Montana, and Idaho] Rural Health Research Center, 2004Google Scholar
12. Mooney C, Zwanziger J, Phibbs CS, et al: Is travel distance a barrier to veterans' use of VA hospitals for medical surgical care? Social Science and Medicine 50:1743–1755, 2000Google Scholar
13. Schmitt SK, Phibbs CS, Piette JD: The influence of distance on utilization of outpatient mental health aftercare following inpatient substance abuse treatment. Addictive Behaviors 28:1183–1192, 2003Google Scholar
14. Fortney JC, Booth BM, Blow FC, et al: The effects of travel barriers and age on the utilization of alcohol treatment aftercare. American Journal of Drug and Alcohol Abuse 21:391–406, 1995Google Scholar
15. Arcury TA, Preisser JS, Gesler WM, et al: Access to transportation and health care utilization in a rural region. Journal of Rural Health 21:31–38, 2005Google Scholar
16. Fortney JC, Rost K, Zhang M, et al: The impact of geographic accessibility on the intensity and quality of depression treatment. Medical Care 37:884–893, 1999Google Scholar
17. Wallace AE, Weeks WB, Wang S, et al: Rural and urban disparities in health-related quality of life among veterans with psychiatric disorders. Psychiatric Services 57:851–856, 2006Google Scholar
18. Booth BM, Curran GM: Variations in drinking patterns in the rural South: joint effects of race, gender, and rural residence. American Journal of Drug and Alcohol Abuse 32:561–568, 2006Google Scholar
19. Substance Abuse or Dependence in Metropolitan and Non-metropolitan Areas. Rockville, Md, Substance Abuse and Mental Health Services Administration, Jan 3, 2003. Available at www.oas.samhsa.gov/2k3/urban/urban.htmGoogle Scholar
20. Tessler R, Rosenheck R, Gamache G: Declining access to alcohol and drug abuse services among veterans in the general population. Military Medicine 170:234–238, 2005Google Scholar
21. Hendryx MS, Rohland BM: A small area analysis of psychiatric hospitalizations to general hospitals: effects of community mental health centers. General Hospital Psychiatry 16:311–312, 1994Google Scholar
22. Folland S, Stano M: Sources of small area variations in the use of medical care. Journal of Health Economics 8:85–107, 1989Google Scholar
23. Rosenheck R, Astrachan B: Regional variation in patterns of inpatient psychiatric care. American Journal of Psychiatry 147:1180–1183, 1990Google Scholar
24. Barbour G, Kizer KW, Ashton CM, et al: Geographic variations in utilization rates in Veterans Affairs hospitals and clinics. New England Journal of Medicine 340:32–39, 1999Google Scholar
25. Friss L, Friedman B, Demakis J: Geographic differences in the use of Veterans Administration hospitals. Social Science and Medicine 28:347–354, 1989Google Scholar
26. Weeks WB, Bott DM, Bazos DA, et al: VA patients' use of the private sector for coronary revascularization in New York: opportunities to improve outcomes by directing care to high performance hospitals. Medical Care 44:519–526, 2006Google Scholar
27. English JT: News Release: APA Urges House Appropriations Subcommittee to Increase Funding for Veterans. Arlington, Va, American Psychiatric Association, 2003. Available at www.psych.org/newsroom/pressreleases/urgesfund4vet41003.pdfGoogle Scholar



