Association of Chronic Work Stress, Psychiatric Disorders, and Chronic Physical Conditions With Disability Among Workers
During the past decade, globalization, new technologies, and changes in workforce demographic characteristics have created new occupational health challenges ( 1 , 2 , 3 ). Workers have increasingly reported exposure to stressful work environments with tighter deadlines and increased production targets set with seemingly little consideration for individual workload ( 4 , 5 , 6 ). Downsizing and restructuring of companies appear to be taking their toll on functioning and worker health status ( 2 , 3 ).
For instance, an association between psychological distress and disability has been observed. Kouzis and Eaton ( 7 ) examined the role of distress on total disability days (days spent in bed for all or most of the day), and they found that the odds of experiencing a total disability day increased with high distress, even when the effects of psychiatric and chronic physical disorders were taken into account. In these types of studies, psychological distress is measured as a set of symptoms.
Other studies have examined the link between demands of a job on disability. For example, Bourbonnais and Mondor (8) reported an association between job strain and short-term sick leave among nurses. Thus there is evidence that job characteristics have an effect on work productivity.
In addition, data are accumulating regarding the negative impact of work stress on both mental and physical health ( 9 , 10 , 11 ). For instance, high-strain work has been observed to be related to a higher risk of self-reported mental health problems ( 12 ). A two- to fourfold increase in risk of depression has been associated with inadequate employment ( 13 ), and a twofold increase in risk of any psychiatric condition has been found among those experiencing work-related stress ( 8 ). It has also been observed that job strain and work stress are associated with emotional exhaustion, worse health status, and development of chronic physical conditions ( 9 , 10 , 11 ).
There is strong evidence that psychiatric disorders extract a heavy burden on the working population in the form of disability. Depression has been identified as a leading cause of disability worldwide ( 14 ). The third most common reason for prolonged absences among public service employees were psychiatric disorders, and the second most common reason among women for absences exceeding three weeks was psychiatric disorders ( 15 ). In addition, as opposed to chronic physical conditions, whose predominant effect is absenteeism, it has been observed that the predominant effect of psychiatric disorders was on increased disability in the form of an increased number of partial disability days (days during which an individual was present but cut back on work) and extra effort days (days during which an individual functioned only with extreme effort), after the analysis controlled for occupation and sociodemographic characteristics—such as age, sex, marital status, education, and income ( 16 ). In contrast, the combination of comorbid mental and chronic physical conditions has been observed to be associated with disability in a different way than either condition alone ( 16 , 17 , 18 ).
Furthermore, accumulating evidence suggests that psychiatric disorders impair rather than completely incapacitate workers' functional ability ( 16 , 17 , 19 ). It is estimated that for a two-week period, the average depression-related presenteeism (present but not able to work) is about four hours per week, or $36 billion (USD) ( 20 ).
Building on previous work ( 16 ), this study used data from a nationally representative, population-based epidemiological survey to conduct a secondary analysis exploring the relationships between psychiatric disorders, chronic work stress, chronic physical conditions, and disability in a working population. Because the data used are cross-sectional, this study cannot make statements about causality. However, the data allow us to explore how the relationship between disability and the combination of chronic work stress and psychiatric disorders differs from the relationship between disability and the combination of chronic work stress and chronic physical conditions. Thus in this article we seek to address the following questions: Are psychiatric disorders, chronic workplace stress, and chronic physical conditions associated with disability among workers? And how are these factors associated with worker disability when they are experienced alone versus in combination with one another?
Methods
Data source
The population for this study was drawn from the Canadian Community Health Survey (CCHS) 1.2, a national population-based survey designed to gather cross-sectional data on the health status, determinants of health, and health care utilization of a representative sample of Canadians ( 21 ). Data were collected between May 2002 and December 2002. Each respondent was given a structured diagnostic interview developed for the World Health Organization's World Mental Health Initiative 2000 ( 22 ).
Sampling for the CCHS-1.2 was based on the standard area probability frame employed by Statistics Canada for its Labour Force Survey ( 23 ). The frame includes the entire country excluding the northern territories, individuals living on Indian reserves or in institutions, and full-time military personnel. The sampling was based on a stratified cluster design in which individuals were randomly sampled from households. Eligible respondents were 15 years and older ( 24 ). The response rate was 77% percent, yielding a sample size of nearly 37,000 respondents ( 23 ).
Study population
The study used CCHS respondents aged 18 to 64 years who indicated that they were employed during the past year (N=22,118). By using a similar selection process as Kessler and Frank ( 19 ) and Dewa and Lin ( 16 ), our study excluded persons who indicated that they were a full-time student, permanently unable to work, retired, or currently on maternity leave.
Dependent variables
The primary dependent variables for this study were based on respondent answers to three questions that asked how many days in the past 14 days had they been in bed for all or most of the day (total disability day), cut down on their normal activities (partial disability day), or were able to complete normal activities with extreme effort (extra effort day). The numbers of respondents indicating the three types of disability day were 1,259, 2,466, and 2,478, respectively.
Independent variables
Four categories of independent variables were used: sociodemographic characteristics, type of disorder or chronic condition, occupational group, and province or region.
Sociodemographic indicators. Dummy variables were created for sex, marital status, and educational level. Age was included as a continuous variable.
Four socioeconomic status dummy variables (low income, lower middle, upper middle, and high income) were created on the basis of household size and income ( 25 ). For example, a household of five or more people with an annual income of less than $30,000 was categorized as low income; the same was true of households of one or two people with an annual income of less than $15,000.
With regard to race or ethnicity, respondents were categorized into one of two categories—either white or nonwhite. The decision to create only two categories was based on the fact that the proportions of separate racial or ethnic groups were too small to be meaningful. Of the 22,118 persons in the sample, 19,584 persons (88.6%) were white. Of the 11.4% of workers who were not white, less than half were black (324 persons, or 1.5%), Asian (687 persons, or 3.1%), or Hispanic (113 persons, or .5%), with the remainder falling into seven other ethnic groups (1,382 persons, or 6.3%)—for example, West Asian or Native Canadian.
Disorders and chronic conditions. The CCHS-1.2 measured six psychiatric disorders falling into the broad categories of mood and anxiety disorders by using structured interview modules from the most recent Composite International Diagnostic Interview that were based on DSM-IV criteria ( 22 , 26 ). The disorders included were depression, mania, agoraphobia, generalized anxiety disorder, and panic disorder.
The CCHS-1.2 also collected information about symptoms associated with addictions and eating problems. Problems with drugs, alcohol, and gambling were assessed by using modified versions of the World Mental Health 2000 interview modules (Ledrou I, personal communication, 2003). Problems with eating were assessed by using a version of the Eating Attitudes Test ( 27 ). Although responses to these questions are not strictly interpretable as DSM-IV mental disorders, they nevertheless indicate symptom levels strongly suggestive of the presence of disruptive or disordering problems.
Presence of any of the above disorders or problems in the past year was coded as 1 if it were present and as 0 if not.
The chronic physical condition indicator was scored as 1 if respondents affirmed having at least one chronic condition diagnosed by a health professional that lasted more than six months during the past year and as 0 otherwise. Conditions included asthma, fibromyalgia, arthritis, high blood pressure, chronic bronchitis, emphysema or chronic obstructive pulmonary disease, epilepsy, heart disease, diabetes, cancer, stomach or intestinal ulcers, stroke, bowel disorder, chronic fatigue syndrome, or migraines.
A dummy variable for chronic work stress was created by using a single-item question that asked respondents to consider their main job or business and to rate whether they found most days in the past 12 months not at all stressful, not very stressful, a bit stressful, quite a bit stressful, or extremely stressful. Respondents in the last two categories were identified as experiencing chronic work stress. Thus, in these analyses, rather than a set of symptoms (that is, psychological distress), chronic work stress indicates the respondents' perceived exposure to stressful stimuli. That is, responses were reflective of how respondents viewed their work environments and job characteristics.
Because the conditions do not occur in isolation and are correlated, interaction terms were created to capture the effects of the presence of several conditions. Seven indicator variables for the presence of multiple conditions were created from the psychiatric disorder, chronic physical condition, and chronic work stress variables. These mutually exclusive variables were chronic work stress only, a chronic physical condition only, a psychiatric disorder only, a chronic physical condition plus chronic work stress, a psychiatric disorder plus chronic work stress, a psychiatric disorder plus a chronic physical condition, and chronic work stress plus a psychiatric disorder plus a chronic physical condition. Respondents with none of these conditions served as comparisons.
Occupational group indicators. Occupational dummy variables identified which of nine occupational groups respondents endorsed: manager, professional, technician, administration, sales, trades, farm, manufacturing, or other ( 25 ).
Province or region indicators. Five province or region indicators were created to indicate the respondent's province or region of residence. These included British Columbia, the Prairies (the provinces of Alberta, Saskatchewan, and Manitoba), Ontario, Quebéc, and the Maritimes (the provinces of New Brunswick, Nova Scotia, Prince Edward Island, and Newfoundland).
Analyses
All analyses were done with SAS version 9. Descriptive characteristics of respondents who reported having a total disability day, a partial disability day, or an extra effort day were calculated. To compare the prevalence rates of psychiatric disorders, chronic work stress, chronic physical conditions, and combinations of these conditions, 95% confidence intervals for all estimates were calculated by using the bootstrap resampling SAS macro developed by Statistics Canada ( 28 ) to account for the CCHS's complex sampling design. The bootstrap variance estimator is the standard deviation of the point estimates calculated for each of 500 samples by using the bootstrap weights.
To examine the association of psychiatric disorders, chronic workplace stress, chronic physical conditions, and combinations of these conditions with disability among workers, logistic regressions were used that controlled for sociodemographic characteristics, province or region, and occupational grouping. Occupational dummy variables were used to control for unobserved factors on the basis of two assumptions. First, we assumed that participants' decisions to select their occupations were not made at random. As a result, choice of occupation may be linked to factors also associated with disability. Second, we assumed that occupation also reflects the workplace environment and characteristics that might be associated with disability. We used occupational status to generally adjust for unknown participant and workplace characteristics, particularly because our concern is the relationship between chronic work stress, health, and mental health status and disability rather than these other factors. Thus the occupational dummy variables were included to adjust our estimates for unobserved participant heterogeneity in much the same way as a fixed effects specification.
Results
Overall, 32.8% of our sample (N=7,255) met the definition for having no condition. Among the respondents, 6,768 (30.6%) experienced chronic work stress either alone or in combination with a chronic physical condition, a psychiatric disorder, or both. A total of 10,196 (46.1%) reported at least one chronic physical condition either alone or accompanied by chronic work stress or a psychiatric disorder. Finally, 2,367 (10.7%) met our definition of a psychiatric disorder. Generally, there was a decreasing trend among respondents reporting combinations of conditions.
The reverse pattern was observed when the relationship between the combinations of conditions and disability days were examined—that is, the proportions of individuals with a disability day grew as the combinations of conditions increased from no condition to the co-occurrence of a psychiatric disorder, a chronic physical condition, and chronic work stress. Although this pattern held across all three types of disability days, a partial disability day and an extra effort day presented with a steeper gradient than a total disability day.
In general, as the type of disability changed from the more obvious (total disability day) to the less obvious (extra effort day), the proportions experiencing disability increased. A higher proportion of women reported each of the three types of disability days compared with men. In addition, compared with married respondents, a greater percentage of those who were single experienced disability—particularly a total disability day, a partial disability day, or both. Compared with nonwhites, white respondents were more likely to report both a partial disability day and an extra effort day, although the two groups experienced a total disability day in similar proportions.
Socioeconomic status was not significantly associated with disability. Respondents across different education and income levels endorsed the disability items in consistent proportions.
Ontarians and Quebécers were less likely than respondents from British Columbia and the Prairies to report a partial disability day or an extra effort day. Compared with all other respondents, Quebécers were less likely to report having a total disability day.
Logistic regression results are shown in Table 1 . In general, compared with no condition, increasing combinations of psychiatric disorders, chronic physical conditions, or chronic work stress were associated with increasing odds of reporting disability after the analysis controlled for sociodemographic characteristics, occupation, and region.
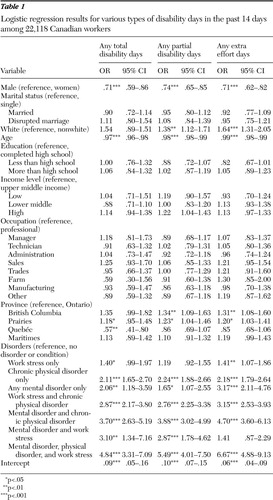 |
The odds of the three types of disability days were consistent among individuals reporting a chronic physical condition only (total disability day, OR=2.11; partial disability day, OR=2.24; and extra effort day, OR=2.18) and chronic physical condition plus chronic work stress (total disability day, OR=2.87; partial disability day, OR=2.76; and extra effort day, OR=3.15). The odds of disability days were elevated for chronic work stress only, but the effect was not as large and the confidence interval around the estimate included 1.00 for a total disability day and a partial disability day (total disability day, OR=1.40, and extra effort day, OR=1.41; the OR for a partial disability day was 1.19, but this finding was not significant).
Respondents with a psychiatric disorder only had higher odds of reporting an extra effort day (OR=3.17) than either a total disability day (OR=2.06) or a partial disability day (OR=1.65), whereas a psychiatric disorder plus chronic work stress was associated with the opposite pattern (total disability day, OR=3.10; partial disability day, OR=2.87; and extra effort day, OR=1.41, although the finding for extra effort day was not significant). A psychiatric disorder plus a chronic physical condition and the combination of these two plus chronic work stress were associated with highest odds of disability ( Figure 1 ).
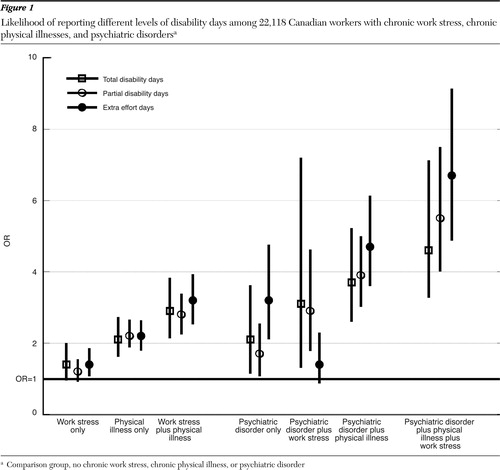
The magnitude of the odds ratios for the three disability types also increased as the type of disability changed from the most obvious (total disability day, OR=4.84) to the least obvious (extra effort day, OR=6.67) for a combination of a psychiatric disorder plus a chronic physical condition plus chronic work stress ( Figure 1 ).
Discussion
Consistent with the literature, our results indicate about a third of workers experience chronic work stress. Bond and colleagues ( 6 ) found that 26% of workers reported that they are "often or very often burned out or stressed" by their work. A recent survey by the Canadian Mental Health Association ( 29 ) found that 25% of employed respondents identified work as a major source of stress and anxiety.
Our results also corroborate reports indicating that comorbid psychiatric disorders and chronic physical conditions are more disabling than either condition alone ( 16 , 17 , 19 ). Workers in our sample with both conditions had odds ratios of reporting disability days that were between a third to nearly twice as high as those for workers with either condition alone.
In the case of chronic physical conditions, the additional presence of chronic work stress appeared to increase the probability of any type of disability day. These results suggest that workers being treated for chronic physical conditions may be an important group to consider for workplace stress intervention. In addition, there is evidence that early intervention with this group may decrease the likelihood of mental disorders ( 30 ).
Our findings indicate a more complex disability pattern than previously reported for the association between psychiatric disorders and disability days in the presence of chronic work stress ( 16 ). In the presence of chronic work stress, rather than primarily affecting extra effort days, psychiatric disorders were associated with an increased probability of total and partial disability days. This suggests that with chronic work stress, workers with mental illness experience more intense disability days.
Nearly 40% of those with chronic work stress or a chronic physical disorder or psychiatric disorder reported two or more of these conditions. These findings would be consistent with a single construct—for example, diminished capacity—as opposed to separate, independent domains. Our data cannot elucidate whether it is more appropriate to conceptualize chronic work stress and psychiatric and physical disorders as independent or as manifestations of a single phenomenon. However, the association of multiple conditions with increasing odds of disability suggests that at some point, diminished capacity becomes a pervasive rather than a compartmentalized experience.
The observed regional variances may reflect the influence of workplace factors. Our findings are consistent with those of Duxbury and colleagues ( 31 ), who observed that compared with other Canadian provinces, Quebéc workplaces were more supportive of employees' needs—for example, allowing varying work hours, interrupted work days, and telecommuting. This suggests that Quebéc's work environments are more adaptable to worker needs and thus may play a role in mediating the impact of psychiatric and physical disorders and chronic work stress on disability. It is also important to note that beyond individual work environments, broad social and economic pressures may also affect work disability ( 32 ).
These findings should be considered with respect to the study limitations. Measures of disability and work stress were dependent on self-report and thus subject to recall and reporting bias. However, the disability measures used required a 14-day recall period that would improve the self-report accuracy. Furthermore, it has been argued that individuals rather than researchers are best at assessing their own levels of performance and disability ( 33 ). Meerding and colleagues ( 34 ) demonstrated that self-reported productivity was significantly correlated with objective work output. Similarly, Kessler and colleagues ( 18 ) reported agreement between self-reports of work performance and absenteeism and administrative work records of productivity and sick days.
It is also important to note that the disability questions were not limited to work activities. Although we could assume that the levels of functioning in work and nonwork are related, this may not be strictly the case. Because the questions do, however, clearly reflect disability (days spent entirely or partially in bed, days spent unable to function to a completely normal level, or days spent functioning at a normal level but through extreme effort) and disability occurring during a 14-day period among workers, it is not unreasonable to assume that a substantial proportion of disability days reflect lost work productivity and that the patterns described would hold.
Finally, we used cross-sectional data and cannot make statements about causality. It is possible that persons with disorders experience more work stress or that persons at risk of having disorders are in jobs with more conditions adverse to mental health. It is also possible that individuals with a psychiatric disorder or a chronic physical condition are more likely to experience chronic work stress. However, our results suggest that the relationship between disability and the combination of chronic work stress and psychiatric disorders differs from the relationship between disability and the combination of chronic work stress and chronic physical conditions. In turn, there can be an expected difference in the way they affect the workplace.
Conclusions
Our results indicate that chronic work stress may amplify the disability associated with psychiatric disorders and chronic physical conditions. This suggests that treatment focused only on symptoms of psychiatric or physical disorders may miss an important piece of the puzzle. Successfully treating symptoms without considering chronic work stress may be analogous to patching up a flat tire with duct tape while knowing that the patch will not last and that inevitably the tire will again need repair.
Our results indicate that treatment of individuals with psychiatric disorders and chronic physical conditions may require a two-pronged approach. Along with providing treatment for symptoms, the focus should be on assisting the worker to develop effective coping mechanisms at work. In addition, it may be worthwhile to consider whether the workers' environments are compounding the disability. This may require a partnership between the treating physician and employer to identify ways to create a less stressful environment. Herein lies the challenge. Mechanisms must be developed to assist physicians and workplaces to collaboratively consider interventions that go beyond typical clinical or occupational health considerations.
Acknowledgments and disclosures
The analyses for this project were supported by grant ACC-65795 from the Canadian Institutes of Health Research. Dr. Dewa received support from an Ontario Ministry of Health and Long-Term Career Scientist Award. Dr. Koehoorn received support from a Michael Smith Foundation for Health Research Scholar Award.
The authors report no competing interests.
1. Rantanen J: Research challenges arising from changes in worklife. Scandinavian Journal of Work, Environment and Health 25:473–483, 1999Google Scholar
2. Ostry AS, Barroetavena M, Hershler R, et al: Effect of de-industrialisation on working conditions and self reported health in a sample of manufacturing workers. Journal of Epidemiology and Community Health 56:506–509, 2002Google Scholar
3. Bunting M: Willing Slaves. Toronto, HarperCollins, 2005Google Scholar
4. Vezina M, Bourbonnais R, Brisson C, et al: Workplace prevention and promotion strategies. HealthcarePapers 5:32–44, 2004Google Scholar
5. Paoli P, Merllie D: Third European Survey on Working Conditions 2000. Dublin, European Foundation for the Improvement of Living and Working Conditions, 2001Google Scholar
6. Bond JT, Galinsky E, Swanberg JE: The 1997 National Study of the Changing Work Force. Scandinavian Journal of Work, Environment and Health 25:616–624, 1998Google Scholar
7. Kouzis AC, Eaton WW: Psychopathology and the development of disability. Social Psychiatry and Psychiatric Epidemiology 32:379–386, 1997Google Scholar
8. Bourbonnais R, Mondor M: Job strain and sickness absence among nurses in the province of Quebec. American Journal of Industrial Medicine 39:194–202, 2001Google Scholar
9. Bourbonnais R, Comeau M, Vezina M, et al: Job strain, psychological distress, and burnout in nurses. American Journal of Industrial Medicine 34:20–28, 1998Google Scholar
10. Shields M: Stress, health and the benefit of social support. Health Reports 15:9–38, 2004Google Scholar
11. Ibrahim SA, Scott FE, Cole DC, et al: Job strain and self-reported health among working women and men: an analysis of the 1994/5 Canadian National Population Health Survey. Women Health 33:105–124, 2001Google Scholar
12. Amick BC III, Kawachi I, Coakley EH, et al: Relationship of job strain and iso-strain to health status in a cohort of women in the United States. Scandinavian Journal of Work, Environment and Health 24:54–61, 1998Google Scholar
13. Grzywacz JG, Dooley D: "Good jobs" to "bad jobs": replicated evidence of an employment continuum from two large surveys. Social Science and Medicine 56:1749–1760, 2003Google Scholar
14. World Health Report 2001: Mental Health: New Understanding, New Hope. Geneva, World Health Organization, 2001Google Scholar
15. Stansfeld S, Feeney A, Head J, et al: Sickness absence for psychiatric illness: the Whitehall II Study. Social Science and Medicine 40:189–197, 1995Google Scholar
16. Dewa CS, Lin E: Chronic physical illness, psychiatric disorder and disability in the workplace. Social Science and Medicine 51:41–50, 2000Google Scholar
17. Lim D, Sanderson K, Andrews G: Lost productivity among full-time workers with mental disorders. Journal of Mental Health Policy and Economics 3:139–146, 2000Google Scholar
18. Kessler RC, Ormel J, Demler O, et al: Comorbid mental disorders account for the role impairment of commonly occurring chronic physical disorders: results from the National Comorbidity Survey. Journal of Occupational and Environmental Medicine 45:1257–1266, 2003Google Scholar
19. Kessler RC, Frank RG: The impact of psychiatric disorders on work loss days. Psychological Medicine 27:861–873, 1997Google Scholar
20. Stewart WF, Ricci JA, Chee E, et al: Cost of lost productive work time among US workers with depression. JAMA 289:3135–3144, 2003Google Scholar
21. Gravel R, Beland Y: The Canadian Community Health Survey: mental health and well-being. Canadian Journal of Psychiatry 50:573–579, 2005Google Scholar
22. World Mental Health Survey Initiative. World Mental Health, 2003. Available at www.hcp.med.harvard.edu/wmh. Accessed Apr 24, 2003Google Scholar
23. Statistics Canada: Labour Force Survey FAQ webpage. Statistics Canada, 2003. Available at www.statcan.ca/english/survey/labour/labour.htm. Accessed Apr 23, 2003Google Scholar
24. Canadian Community Health Survey, Cycle 1.2 Interviewer training guide. Ottawa, Statistics Canada, 2002Google Scholar
25. Canadian Community Health Survey (CCHS) Cycle 1.2 Derived Variable (DV) Specifications. Ottawa, Statistics Canada, 2004Google Scholar
26. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC, American Psychiatric Association, 1994Google Scholar
27. Garner DM, Olmsted MP, Bohr Y, et al: The eating attitudes test: psychometric features and clinical correlates. Psychological Medicine 12:871–878, 1982Google Scholar
28. Canadian Community Mental Health Survey—Mental Health and Well-being. Statistics Canada, 2005. Available at www.statcan.ca/english/sdds/5015.htm. Accessed Jan 17, 2005Google Scholar
29. The 2001 Canadian Mental Health Survey. Canadian Mental Health Association, 2001. Available at www.cmha.ca/bins/contentpage.asp?cid=4-42-213. Accessed July 29, 2005Google Scholar
30. Nitzkin J, Smith SA: Clinical Preventive Services in Substance Abuse and Mental Health Update: From Science to Services. Rockville, Md, Substance Abuse and Mental Health Services Administration, 2004Google Scholar
31. Duxbury L, Higgins C: Where to Work in Canada? An Examination of Regional Differences in Work Life Practices. Report Commissioned by the BC Work-Life Summit 2003. Ottawa, Canadian Policy Research Network, 2003Google Scholar
32. Dew K, Keefe V, Small K: "Choosing" to work when sick: workplace presenteeism. Social Science and Medicine 60:2273–2282, 2005Google Scholar
33. Kessler RC, Ames M, Hymel PA, et al: Using the World Health Organization Health and Work Performance Questionnaire (HPQ) to evaluate the indirect workplace costs of illness. Journal of Occupational and Environmental Medicine 46(suppl 6):S23–S37, 2004Google Scholar
34. Meerding WJ, IJzelenberg W, Koopmanschap MA, et al: Health problems lead to considerable productivity loss at work among workers with high physical load jobs. Journal of Clinical Epidemiology 58:517–523, 2005Google Scholar



