Alcohol Use Disorders and the Use of Treatment Services Among College-Age Young Adults
An estimated 44% of U.S. college students are binge drinkers ( 1 ). Excessive drinking in late adolescence and early adulthood can have serious consequences, including injuries ( 2 ), risky sexual behaviors ( 3 , 4 ), and poor academic performance ( 5 ).
Binge drinking and heavy alcohol use among college students have been studied extensively, and an increasing number of studies have focused on early detection and intervention programs for college students ( 6 , 7 ). However, alcohol use disorders among college students have received less research attention until recently ( 3 , 8 , 9 ). In particular, little is known about the use of alcohol treatment services among 18- to 22-year-olds.
Studies of use of alcohol treatment services have typically covered a very wide age range rather than focusing specifically on young adults ( 10 , 11 , 12 , 13 , 14 ). Andersen's behavioral model of health service utilization ( 11 , 13 , 15 , 16 ) suggests that the use of treatment services is determined by predisposing characteristics, such as demographic characteristics and attitudes toward treatment or illness; enabling characteristics, such as family income; and needs-related characteristics, such as severity of alcohol problems.
Gender, age group, race or ethnicity, education, marital status, family income, and employment status are reported to be associated with use of alcohol treatment services ( 10 , 11 , 13 , 16 , 17 ), with some variations by characteristics, such as age and ethnicity ( 16 , 18 , 19 ). Additional characteristics associated with the use of alcohol treatment services include symptoms of alcohol abuse or dependence and comorbid drug use disorders ( 17 , 18 , 20 ).
A prior study reported that 6% of college students with alcohol dependence had received alcohol treatment services since starting college ( 3 ). However, the characteristics and specific symptoms of alcohol use disorders that were associated with treatment in this group were not examined, nor were the full-time students compared with others of the same age who were not in college full-time. Planning of treatment delivery requires information about all relevant groups.
Because full-time college students, part-time college students, noncollege students (those in school at a grade level below college), and nonstudents may differ in important ways, we examined the following questions among young adults who met criteria for an alcohol use disorder: What personal and clinical characteristics were associated with the receipt of alcohol services, and did this differ by educational status? What personal and clinical characteristics were associated with perceiving a need for alcohol treatment, and did this differ by educational status? Were particular symptoms of alcohol use disorder as specified in DSM-IV ( 21 ) associated with receiving or perceiving a need for alcohol treatment?
Methods
Data sources
Statistical analyses were based on data from the public use file of the 2002 National Survey on Drug Use and Health (NSDUH), formerly known as the National Household Survey on Drug Abuse. The survey is conducted annually to collect data on substance use and disorders by civilian, noninstitutionalized Americans ages 12 or older ( 22 ). It uses multistage area probability sampling methods ( 23 ) to select survey respondents, including residents of noninstitutional group quarters (shelters, rooming houses, dormitories, and group homes), residents of all 50 states and the District of Columbia, and civilians residing on military bases.
To increase respondents' willingness to report substance use behaviors ( 24 ), the survey uses a combination of computer-assisted personal interviewing and audio computer-assisted self-interviewing (ACASI) methodologies. ACASI was used for sensitive survey items, for which respondents either read the questions silently on a computer screen or listened to questions being read aloud on the computer through headphones and then entered their responses directly into the computer. The data collection procedures were approved by the Committee for the Protection of Human Subjects at RTI International.
A total of 68,126 individuals ages 12 or older participated in the 2002 survey. A weighted screening response rate of 91% was achieved, and the weighted interview response rate was 79%. Analysis weights were developed to adjust for variation in household selection, nonresponse, and poststratification of the selected sample to census data. The annual sample of NSDUH is considered representative of the U.S. general population of ages 12 and older. Its design and data collection procedures have been reported in detail elsewhere ( 22 ).
Study variables
College enrollment. Our sample consisted of 11,337 college-age young adults. In NSDUH college-age young adults were defined as those 18 to 22 years old, and they were categorized into two main groups: full-time college students and persons not enrolled full-time in college ( 22 ). Using questions about current education and enrollment status, the NSDUH further classified the latter group into three groups: part-time college students, noncollege students (for example, students currently in a school other than a college or who did not provide information on college enrollment), and nonstudents (not in school). The group of noncollege students might include high school students, students in a GED program, and those studying at a technical or vocational school.
Demographic characteristics. We examined the following self-reported respondent characteristics: age, race or ethnicity, marital status, employment status (employed, unemployed or laid off, and not employed in the labor force), total family income, and population density of the area where the respondent lived (large metropolitan areas with a population of one million or more, small metropolitan areas with a population less than one million, and nonmetropolitan areas outside a metropolitan statistical area) ( 22 ).
Past-year alcohol and drug use disorders. Past-year alcohol use disorders and drug use disorders were assessed with DSM-IV criteria ( 21 , 22 ). Alcohol dependence referred to the presence of at least three alcohol dependence criteria in the past year. Alcohol abuse included respondents who reported a pattern of symptoms that met DSM-IV alcohol abuse criteria in the past year and who did not meet criteria for dependence. "Any drug dependence" referred to meeting criteria for DSM-IV drug dependence for one or more of the following drugs in the past year: cocaine or crack, marijuana or hashish, heroin, hallucinogens, inhalants, sedatives, tranquilizers, pain relievers, and stimulants. "Any drug abuse" included DSM-IV -defined abuse of any of these drugs in the past year. Four mutually exclusive groups of drug use were defined: no use in the past year, use without abuse or dependence, abuse, and dependence. Years of alcohol use were obtained by subtracting age of onset of alcohol use from the age at interview and were categorized into three groups (one to two years, three to four years, and five or more years).
Utilization of alcohol treatment services. Respondents were asked about past-year use of substance abuse services, the treatment setting (residential addiction rehabilitation facilities, mental health facilities, private doctors' offices, hospitals, jails or prisons, or self-help groups), and whether the service received was for alcohol-related problems. A specialty service referred to the receipt of alcohol services in any of the following settings: inpatient alcohol treatment or any alcohol treatment services at a residential addiction center or at a mental health facility ( 19 ).
Perceived need for treatment and reasons for not receiving services. The subsample of respondents who reported not receiving any alcohol-related treatment or counseling in the prior year were asked whether they felt they needed alcohol-related treatment or counseling during this period. A positive response to this question was defined as perceiving a need for alcohol treatment services ( 19 ). Those who reported a need for services were asked to identify the reasons for not receiving these services.
Data analysis
Because NSDUH uses multistage probability sampling methods, the data were weighted and analyzed by SUDAAN software ( 25 ) to account for complex design effects. All percentages reported in this article are weighted estimates, whereas sample sizes are unweighted.
We first examined the prevalence of alcohol use disorders by college enrollment status. Among past-year alcohol users, we conducted logistic regression analyses to determine the association of alcohol use disorder with college enrollment status and the other potential correlates. We then determined the characteristics associated with the use of alcohol services among young adults with an alcohol use disorder.Among the subsample of young adults with an alcohol use disorder who did not receive any alcohol services, we examined their perceived needs for these services. Finally, we determined whether service use and the perceived need for services varied byspecific symptoms of alcohol use disorders.We report odds ratios (ORs) from thelogistic regression procedures that denotedthe strength of an association betweena dichotomous outcome variable (service use) and the potential correlates (college enrollment status).
Results
Sociodemographic characteristics
Of all young adults ages 18 to 22 (N=11,333), 38% were full-time college students, 7% were part-time college students, 11% were noncollege students, and 45% were nonstudents. These proportions did not vary by gender or age group. Approximately 38% of young adults were from nonwhite minority groups, 9% had ever been married, and 69% were currently employed.
Alcohol use disorders, by college enrollment status
Among all young adults ages 18 to 22, close to 19% met criteria for past-year alcohol use disorders (11.3% for abuse and 7.4% for dependence), and 9% met criteria for past-year drug use disorders (2.9% for abuse and 6.1% for dependence). Table 1 shows that college enrollment status was associated with alcohol use disorder ( χ2 =41.54, df=3, p<.001). Full-time college students had a higher prevalence (21%) of alcohol use disorder than part-time college students (15%) and noncollege students (12%). Alcohol dependence was higher among full-time college students (8%) than among other students (3%-5%) but similar to that of nonstudents (8%).
 |
Characteristics associated with alcohol use disorders among past-year alcohol users (N=8,881) are reported in Table 2 . Part-time college students and noncollege students were less likely than full-time college students to meet criteria for an alcohol use disorder, whereas there was no difference in the odds of having an alcohol use disorder between full-time college students and nonstudents.
 |
Men, non-Hispanic white students (compared with non-Hispanic black students), those who had never been married, those in the lowest level of family income (compared with those with a family income between $40,000 and $74,999), and young adults residing in nonmetropolitan areas (compared with those in large metropolitan areas) had increased odds of having alcohol use disorders. More years of alcohol use and having a drug disorder or using drugs were highly associated with alcohol use disorders.
Service utilization, by college enrollment status
The prevalence and likelihood of past-year use of alcohol treatment services are reported in Table 3 . Use of specialty alcohol treatment (data not shown) was defined as a subset of overall treatment service use. Among those with an alcohol use disorder, very few full-time college students used services: 3.9% used any services and 1.9% used specialty services. The prevalence for part-time college students was 7.4% and 2.8%, respectively. Noncollege students were slightly more likely than the other groups to use services: 9.8% and 7.3% used any services and specialty services, respectively.
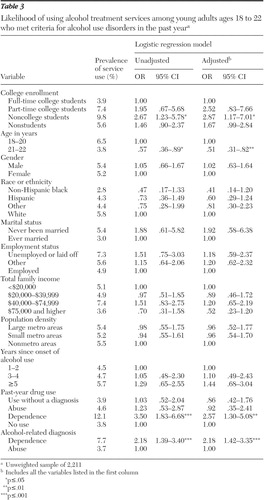 |
We also examined the prevalence of service use separately for abuse and dependence (data not shown). The overall use of any alcohol services was higher among those with alcohol dependence (7.7%) than among those with alcohol abuse (3.7%). Only 7% of full-time college students with alcohol dependence received any alcohol services in the past year.
Characteristics associated with alcohol service use among 2,211 young adults with an alcohol use disorder in the past year are reported in Table 3 . Compared with full-time college students, noncollege students were about three times as likely to use any alcohol services (adjusted OR=2.87). There were no differences in service use between full-time college students and the other groups. In addition, young adults ages 21 or 22 were less likely than those of ages 18 to 20 to use any services (adjusted OR=.51). Service use also was associated with alcohol dependence (adjusted OR=2.18) and with comorbid past-year drug dependence (adjusted OR=2.57).
Perceived need for alcohol treatment services
Very few young adults who met criteria for a past-year alcohol use disorder and did not receive any alcohol services in the past year reported needing alcohol services ( Table 4 ). The prevalence of the perceived need for alcohol treatment among young adults with an alcohol use disorder was 2.4% for full-time college students, .7% for part-time college students, 2.9% for noncollege students, and 3.4% for nonstudents. We also found that students with alcohol dependence (6.2%) were more likely than those abusing alcohol (.7%) to perceive the need for such treatment.
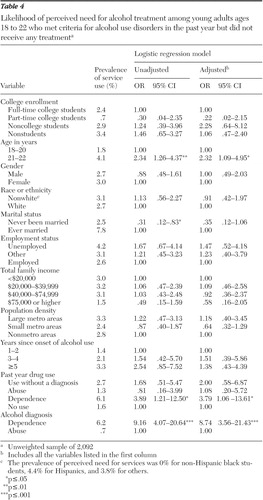 |
ORs of perceived need for alcohol services among 2,092 young adults with a past-year alcohol use disorder who did not receive any alcohol treatment services are reported in Table 4 . Whereas college enrollment status was not associated with the perceived need for alcohol services, older age (adjusted OR=2.32), alcohol dependence (adjusted OR=8.74), and comorbid drug dependence (adjusted OR=3.79) were associated with increased odds of perceiving a need for such services.
Alcohol use disorder, service use, and perceived need for services
We used logistic regression models separately for abuse and dependence to examine whether specific symptoms of alcohol use disorder were associated with service use and the perceived need for such services ( Table 5 ). Controlling for age, gender, college enrollment, and past-year drug use status—which was associated with alcohol use disorder or service use—we found that "alcohol use causing troubles with the law" was associated with increased use of alcohol services, without a concomitant increase in the perceived need for these services. In addition "continued alcohol use despite problems with family or friends" and "serious problems at work, home, or school" were associated with a perceived need for services.
 |
Alcohol dependence, service use, and perceived need for services
In the model for dependence symptoms, "reduced important activities" and "caused emotional or physical problems" were associated with service use. Significant correlates of a perceived need for alcohol services included "spent a great deal of time getting or using alcohol," "caused emotional or physical problems," and "was unable to cut down on use."
Reasons for not receiving alcohol services
The subsample with an alcohol use disorder who did not receive any alcohol service but reported the perceived need for such services was small, only 46 students. The most common reasons for not using services were "not ready to stop using alcohol and/or drugs" (47%), "having no health care coverage and unable to afford the cost" (19%), "concerned that getting services might cause neighbors and community to have a negative opinion" (18%), and "not knowing where to go to get treatment" (15%).
Discussion
In this nationally representative sample of young adults ages 18 to 22, we found a high prevalence of alcohol use disorders and a low prevalence of alcohol service use. About one-fifth of college-age young adults met criteria for a past-year alcohol use disorder, which was higher than estimates for adolescents ages 12 to17 (5%) ( 26 ), persons ages 15 to 54 (7%) ( 27 ), and adults ages 30 or older (less than 6% for abuse and less than 4% for dependence) ( 28 ). Our finding was similar to a recent estimate (18%) among all young adults ages 18 to 24 ( 8 ).
Prevalence of alcohol use disorders among part-time and noncollege students was lower than among full-time college students. Part-time and noncollege students are more likely to live with their parents than full-time college students, which may have some protective effects on alcohol abuse ( 29 ) because those living with their parents may be more likely to be monitored and less likely to spend long hours with alcohol-using peers or in a context that promotes alcohol use behaviors (such as bars in college towns). The resulting reduction of opportunities for alcohol exposure may contribute to moderation and lessen the risk of alcohol abuse. This explanation is speculative and requires future work to test it. Noncollege students seem to be an important subgroup to study further. They had a lower prevalence of alcohol use disorders than full-time college students but were more likely to receive alcohol services. The reasons why they were still in high school (or technical or vocational schools) were unavailable in the survey.
We also found that full-time college students were as likely as the nonstudent subgroup to have an alcohol use disorder. Frequent alcohol use is associated with increased odds of dropping out of school among high school students, and youths not in school are more likely than those in school to use alcohol ( 30 , 31 ). Yet some aspects of college-related environments also place college students at risk for alcohol abuse. In particular, full-time college students tend to live away from their parents, to associate with peers who use alcohol regularly, and to be in environments where social activities involve alcohol use, which appear to increase their risk of having an alcohol use disorder ( 3 , 4 , 32 ). However, college-related environments seem to have no significant negative influences on drug use disorders, which had a similar prevalence among all young adults. The reason might be related to the greater social acceptability of alcohol use in American colleges compared with drug use. This hypothesis requires confirmation by studies of students' attitudes toward different licit and illicit substance use.
Our data suggest that entry into alcohol treatment services tends to be associated with drug or alcohol dependence and with legal problems. Among those with legal problems, treatment is often mandated by courts. Similarly, those with comorbid drug use problems may come to the attention of family members, health care providers, or the criminal justice system, who then prompt or coerce the person with the disorder into receiving services ( 19 , 33 , 34 , 35 ). Other studies also have suggested that individuals with an alcohol use disorder typically do not seek help until their alcohol use results in substantial problems in their lives ( 36 , 37 ). Denial of alcohol-related problems and lack of motivation to receive treatment may explain this finding ( 38 , 39 ). Consistent with other studies ( 19 , 40 , 41 ), the individual's perception that alcohol use is not a problem was a major barrier to alcohol treatment. Our study found that, among those with an alcohol use disorder who did not receive alcohol services in the past year, only 2.4% of full-time college students reported a need for alcohol services. In addition, young people may have financial barriers or may not know where to go for help and how to obtain confidential alcohol treatment ( 42 , 43 ).
Alternatively, the low prevalence of alcohol treatment use may have resulted, at least in part, from the inclusion of mild cases of alcohol abuse, where the need for treatment is debatable. Such cases might occur when individuals receive a diagnosis of alcohol abuse with only one symptom of abuse, as dictated by DSM-IV. Although studies have suggested that many adults with an alcohol use disorder eventually get better without receiving treatment ( 44 ), treatment or counseling is important for at least some young adults with an alcohol use disorder. In particular, alcohol dependence is more chronic than abuse ( 45 , 46 , 47 ) and may require formal treatment to prevent alcohol-related mental and physical illnesses. Various interventions, including prevention, alcohol treatment services, and harm reduction approaches (such as providing buses on weekend evenings from college towns, where drinking often takes place, to college dormitories), could help reduce substantial direct and indirect consequences of alcohol abuse, including academic problems, violent behaviors, physical injuries, property damage on campuses, and unwanted sexual behaviors, as well as injury and death from driving under the influence of alcohol ( 2 , 3 , 4 , 5 , 6 , 7 ).
The physiological aspects of alcohol use disorders (withdrawal symptoms) predict the chronicity of alcohol dependence ( 48 , 49 ), but they were unassociated with alcohol service use or the perceived need for such services in this study. Rather, alcohol-related social and legal problems, as well as the inability to cut down on alcohol use, increased young adults' or others' recognition of having alcohol problems. The low prevalence of service use (5%) among women with an alcohol use disorder also deserves research attention. Young women appear to be more likely than young men to first adopt binge drinking in college ( 50 ), and college-attending women get drunk more frequently than non-college-attending women ( 9 ).
These findings should be interpreted with some caution. First, NSDUH data, including school enrollment status, are based on respondents' self-reports. Although our key variables referred to past-year behaviors, and NSDUH incorporates computer-assisted interviewing techniques to improve the accuracy of self-reports of substance use behaviors ( 24 ), our findings could be influenced by recall and reporting biases.
Second, NSDUH assessments of alcohol use disorders are based on a single structured interview administered by trained interviewers, and diagnoses are not validated by clinicians. This limitation is found in most large-scale epidemiological studies ( 51 ). Our estimates of alcohol use disorders are much lower than the estimate (38%) from a survey of college students ( 3 ), which suggests that NSDUH is unlikely to largely overestimate the prevalence of alcohol use disorders. Third, the lack of information about the quality of services received prevents our analysis of these variables.
Heavy drinking and alcohol problems increase during the transition into college years ( 52 ). The high prevalence of alcohol use disorders among full-time college students and nonstudent young adults calls for continuous efforts to reduce alcohol use and alcohol-related harm. Both primary prevention and focused interventions have been recommended ( 32 , 53 , 54 , 55 ). Interventions to motivate treatment use among young adults with an alcohol use disorder may be more effective if they build on the symptoms that increase the perceived need for treatment, including associated emotional problems or the inability to reduce alcohol use. Increased availability of and access to community- and college-based alcohol-screening programs may be an effective way to identify individuals with harmful alcohol use behaviors, to offer alcohol-related education, and to refer them to appropriate treatment service programs ( 40 ).
Acknowledgments and disclosures
This work was supported mainly by grant R21-AA-013255 from the National Institute on Alcohol Abuse and Alcoholism to Dr. Wu. It was partly supported by grant R21-DA-015938 from the National Institute on Drug Abuse to Dr. Wu and by grant K05-AA-00161 from the National Institute on Alcohol Abuse and Alcoholism to Dr. Hasin. The Substance Abuse and Mental Health Data Archive and the Inter-University Consortium for Political and Social Research provided the public use data files for the National Survey on Drug Use and Health, which is sponsored by the Office of Applied Studies, Substance Abuse and Mental Health Services Administration. The opinions expressed in this article are solely those of the authors, not of any sponsoring agency. Readers are encouraged to review the original reports of the National Survey on Drug Use and Health for more details on the design of the survey, its data collection methodology, and the survey's limitations.
The authors report no competing interests.
1. Wechsler H, Lee JE, Kuo M, et al: College binge drinking in the 1990s: a continuing problem—results of the Harvard School of Public Health 1999 College Alcohol Study. Journal of American College Health 48:199-210, 2000Google Scholar
2. Hingson R, Heeren T, Winter M, et al: Magnitude of alcohol-related mortality and morbidity among U.S. college students ages 18-24: changes from 1998 to 2001. Annual Review of Public Health 26:259-279, 2005Google Scholar
3. Knight JR, Wechsler H, Kuo M, et al: Alcohol abuse and dependence among U.S. college students. Journal of Studies on Alcohol 63:263-270, 2002Google Scholar
4. Wechsler H, Davenport A, Dowdall G, et al: Health and behavioral consequences of binge drinking in college: a national survey of students at 140 campuses. JAMA 272:1672-1677, 1994Google Scholar
5. Aertgeerts B, Buntinx F: The relation between alcohol abuse or dependence and academic performance in first-year college students. Journal of Adolescent Health 31:223-235, 2002Google Scholar
6. Barnett NP, Tevyaw TO, Fromme K, et al: Brief alcohol interventions with mandated or adjudicated college students. Alcoholism, Clinical and Experimental Research 28:966-975, 2004Google Scholar
7. Hingson RW, Howland J: Comprehensive community interventions to promote health: implications for college-age drinking problems. Journal of Studies on Alcohol 63(Mar suppl):226-240, 2002Google Scholar
8. Dawson DA, Grant BF, Stinson FS, et al: Another look at heavy episodic drinking and alcohol use disorders among college and noncollege youth. Journal of Studies on Alcohol 65:477-488, 2004Google Scholar
9. Slutske WS, Hunt-Carter EE, Nabors-Oberg RE, et al: Do college students drink more than their non-college-attending peers? Evidence from a population-based longitudinal female twin study. Journal of Abnormal Psychology 113:530-540Google Scholar
10. Dawson DA: Gender differences in the probability of alcohol treatment. Journal of Substance Abuse 8:211-225, 1996Google Scholar
11. Grant BF: Toward an alcohol treatment model: a comparison of treated and untreated respondents with DSM-IV alcohol use disorders in the general population. Alcoholism, Clinical and Experimental Research 20:372-378Google Scholar
12. Hasin DS, Grant BF: AA and other helpseeking for alcohol problems: former drinkers in the U.S. general population. Journal of Substance Abuse 7:281-292, 1995Google Scholar
13. Weisner C, Matzger H: A prospective study of the factors influencing entry to alcohol and drug treatment. Journal of Behavioral Health Services and Research 29:126-137, 2002Google Scholar
14. Wu LT, Kouzis AC, Leaf PJ: Influence of comorbid alcohol and psychiatric disorders on utilization of mental health services in the National Comorbidity Survey. American Journal of Psychiatry 156:1230-1236, 1999Google Scholar
15. Andersen RM: Revisiting the behavioral model and access to medical care: does it matter? Journal of Health and Social Behavior 36:1-10, 1995Google Scholar
16. Wu P, Hoven CW, Tiet Q, et al: Factors associated with adolescent utilization of alcohol treatment services. American Journal of Drug and Alcohol Abuse 28:353-369, 2002Google Scholar
17. Hajema KJ, Knibbe RA, Drop MJ: Social resources and alcohol-related losses as predictors of help seeking among male problem drinkers. Journal of Studies on Alcohol 60:120-129, 1999Google Scholar
18. Kirchner JE, Booth BM, Owen RR, et al: Predictors of patient entry into alcohol treatment after initial diagnosis. Journal of Behavioral Health Services and Research 27:339-346, 2000Google Scholar
19. Wu LT, Ringwalt CL: Alcohol dependence and use of treatment services among women in the community. American Journal of Psychiatry 161:1790-1797, 2004Google Scholar
20. Grant BF: The influence of comorbid major depression and substance use disorders on alcohol and drug treatment: results of a national survey, in Treatment of Drug-Dependent Individuals With Comorbid Mental Disorders. Edited by Onken LS, Blaine JD, Genser S, et al. NIDA Research Monograph 172. Rockville, Md, National Institute on Drug Abuse, 1997Google Scholar
21. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC, American Psychiatric Association, 1994Google Scholar
22. Results From the 2002 National Survey on Drug Use and Health: National Findings. Rockville, Md, Substance Abuse and Mental Health Services Administration, Office of Applied Studies, 2003Google Scholar
23. Bowman KR, Chromy JR, Odom DM, et al: 2001 National Household Survey on Drug Abuse: sample design report, in 2001 National Household Survey on Drug Abuse Methodological Resource Book, vol 1, section 2. Research Triangle Park, NC, Research Triangle Institute, 2003Google Scholar
24. Turner CF, Ku L, Rogers SM, et al: Adolescent sexual behavior, drug use, and violence: increased reporting with computer survey technology. Science 280:867-873, 1998Google Scholar
25. SUDAAN User's Manual, release 8.0. Research Triangle Park, NC, Research Triangle Institute, 2002Google Scholar
26. Chung T, Martin CS, Armstrong TD, et al: Prevalence of DSM-IV alcohol diagnoses and symptoms in adolescent community and clinical samples. Journal of the American Academy of Child and Adolescent Psychiatry 41:546-554, 2002Google Scholar
27. Kessler RC, Crum RM, Warner LA, et al: Lifetime co-occurrence of DSM-III-R alcohol abuse and dependence with other psychiatric disorders in the National Comorbidity Survey. Archives of General Psychiatry 54:313-321, 1997Google Scholar
28. Grant BF, Dawson DA, Stinson FS, et al: The 12-month prevalence and trends in DSM-IV alcohol abuse and dependence: United States, 1991-1992 and 2001-2002. Drug and Alcohol Dependence 74:223-234, 2004Google Scholar
29. Gfroerer JC, Greenblatt JC, Wright DA: Substance use in the US college-age population: differences according to educational status and living arrangement. American Journal of Public Health 87:62-65, 1997Google Scholar
30. Yamada T, Kendix M, Yamada T: The impact of alcohol consumption and marijuana use on high school graduation. Health Economics 5:77-92, 1996Google Scholar
31. Wu LT, Schlenger WE, Galvin DM: The relationship between employment and substance use among students aged 12 to 17. Journal of Adolescent Health 32:5-15, 2003Google Scholar
32. Weitzman ER, Nelson TF, Wechsler H: Taking up binge drinking in college: the influences of person, social group, and environment. Journal of Adolescent Health 32:26-35, 2003Google Scholar
33. Grella CE, Joshi V: Gender differences in drug treatment careers among clients in the national Drug Abuse Treatment Outcome Study. American Journal of Drug and Alcohol Abuse 25:385-406, 1999Google Scholar
34. Weisner C, Matzger H, Tam T, et al: Who goes to alcohol and drug treatment? Understanding utilization within the context of insurance. Journal of Studies on Alcohol 63:673-682, 2002Google Scholar
35. Hasin DS: Treatment/self-help for alcohol-related problems: relationship to social pressure and alcohol dependence. Journal of Studies on Alcohol 55:660-666, 1994Google Scholar
36. Bucholz KK, Homan SM, Helzer JE: When do alcoholics first discuss drinking problems? Journal of Studies on Alcohol 53:582-589, 1992Google Scholar
37. Kessler RC, Aguilar-Gaxiola S, Berglund PA, et al: Patterns and predictors of treatment seeking after onset of a substance use disorder. Archives of General Psychiatry 58:1065-1071, 2001Google Scholar
38. Cunningham JA, Sobell LC, Sobell MB, et al: Barriers to treatment: why alcohol and drug abusers delay or never seek treatment. Addictive Behaviors 18:347-353, 1993Google Scholar
39. Grant BF: Barriers to alcoholism treatment: reasons for not seeking treatment in a general population sample. Journal of Studies on Alcohol 58:365-371, 1997Google Scholar
40. Greenfield SF, Keliher A, Sugarman D, et al: Who comes to voluntary, community-based alcohol screening? Results of the first annual National Alcohol Screening Day, 1999. American Journal of Psychiatry 160:1677-1683, 2003Google Scholar
41. Wu LT, Ringwalt CL: Use of alcohol treatment and mental health services among adolescents with alcohol use disorders. Psychiatric Services 57:84-92, 2006Google Scholar
42. Davies J, McCrae BP, Frank J, et al: Identifying male college students' perceived health needs, barriers to seeking help, and recommendations to help men adopt healthier lifestyles. Journal of American College Health 48:259-267, 2000Google Scholar
43. Klein JD, McNulty M, Flatau CN: Adolescents' access to care: teenagers' self-reported use of services and perceived access to confidential care. Archives of Pediatrics and Adolescent Medicine 152:676-682, 1998Google Scholar
44. Dawson DA, Grant BF, Stinson FS, et al: Recovery from DSM-IV alcohol dependence: United States, 2001-2002. Addiction 100:281-292, 2005Google Scholar
45. Hasin DS, Grant B, Endicott J: The natural history of alcohol abuse: implications for definitions of alcohol use disorders. American Journal of Psychiatry 147:1537-1541, 1990Google Scholar
46. Hasin DS, Van Rossem R, McCloud S, et al: Differentiating DSM-IV alcohol dependence and abuse by course: community heavy drinkers. Journal of Substance Abuse 9:127-135, 1997Google Scholar
47. Schuckit MA, Smith TL: A comparison of correlates of DSM-IV alcohol abuse or dependence among more than 400 sons of alcoholics and controls. Alcoholism, Clinical and Experimental Research 25:1-8, 2001Google Scholar
48. Hasin D, Paykin A, Meydan J, et al: Withdrawal and tolerance: prognostic significance in DSM-IV alcohol dependence. Journal of Studies on Alcohol 61:431-438, 2000Google Scholar
49. Schuckit MA, Danko GP, Smith TL, et al: A 5-year prospective evaluation of DSM-IV alcohol dependence with and without a physiological component. Alcoholism, Clinical and Experimental Research 27:818-825, 2003Google Scholar
50. Resnick MD, Bearman PS, Blum RW, et al: Protecting adolescents from harm: findings from the National Longitudinal Study on Adolescent Health. JAMA 278:823-832, 1997Google Scholar
51. Wu LT, Pilowsky DJ, Schlenger WE: High prevalence of substance use disorders among adolescents who use marijuana and inhalants. Drug and Alcohol Dependence 78:23-32, 2005Google Scholar
52. Schulenberg JE, Maggs JL: A developmental perspective on alcohol use and heavy drinking during adolescence and the transition to young adulthood. Journal of Studies on Alcohol Supplement 54-70, 2002Google Scholar
53. Baer JS, Kivlahan DR, Blume AW, et al: Brief intervention for heavy-drinking college students: 4-year follow-up and natural history. American Journal of Public Health. 91:1310-1316, 2001Google Scholar
54. Borsari B, Carey KB: Effects of a brief motivational intervention with college student drinkers. Journal of Consulting and Clinical Psychology 68:728-733, 2000Google Scholar
55. Marlatt GA, Baer JS, Kivlahan DR, et al: Screening and brief intervention for high-risk college student drinkers: results from a 2-year follow-up assessment. Journal of Consulting and Clinical Psychology 66:604-615, 1998Google Scholar



