Direct Care Workers in the National Drug Abuse Treatment Clinical Trials Network: Characteristics, Opinions, and Beliefs
The National Drug Abuse Treatment Clinical Trials Network (CTN) began in 1999 with support from the National Institute on Drug Abuse. Research centers (currently 17) partner with five or more local alcohol and drug treatment centers (currently almost 150 distinct corporations) to conduct multisite clinical trials that test behavioral, pharmacological, and integrated behavioral and pharmacological treatment interventions in treatment programs with heterogeneous patient populations ( 1 ). Successful trials generate evidence of effectiveness and may promote the dissemination and adoption of science-based behavioral and pharmaceutical therapies. The first trials assessed buprenorphine detoxification ( 2 , 3 ), motivational interviewing and motivational enhancement therapy ( 4 ), and low-cost incentives for use with patients in methadone and outpatient programs ( 5 , 6 ). Initial results documented the feasibility of collaboration with community drug abuse treatment centers and provided a foundation for expansion and growth.
Bridging the gap between practice and research, however, requires more than conducting clinical trials in community settings. Individuals who work in the treatment programs are essential to the introduction, adoption, and sustainability of science-based practices. Unfortunately, there is little current information on the workforce that provides treatment services for substance use disorders and on workers' opinions about the use of evidence-based therapies. The Center for Substance Abuse Treatment (CSAT) recognized the lack of a systematic strategy to build counselors' skills and recommended increased attention to the development of alcohol and drug abuse counselors ( 7 ). CSAT's Partners for Recovery initiative includes an emphasis on workforce development ( 8 ). In addition, the Substance Abuse and Mental Health Services Administration supports the Annapolis Coalition on the Behavioral Health Workforce to promote the development of the workforce for mental health and substance use treatment services ( 9 ). The coalition's expert panel on substance use disorders recommended the development of a professional education infrastructure with education and training standards.
The first reports of research on the alcohol and drug abuse treatment workforce are more than 25 years old and provide insight into changes over time. Data from the 1979 National Drug and Alcohol Treatment Utilization Survey (NDATUS) suggested that fewer than one in four counselors (22%) had a graduate degree and that more than one in three (37%) did not have a college degree ( 10 ). A 1985 census of Massachusetts treatment programs found a workforce that was relatively equally divided between men and women, counselors with and without graduate degrees, and staff with and without personal experience in recovery ( 11 ). Women with graduate degrees who did not identify themselves as being in recovery were primarily located in outpatient treatment services; conversely, men without graduate training and in recovery made up a majority of the workforce in detoxification and residential treatment ( 11 ). More recently, the National Treatment Center Study of 400 private facilities noted that a majority of the counselors (56%) were women and most had a master's or doctoral degree ( 12 ).
A CSAT-sponsored survey of the behavioral health workforce estimated that 67,000 individuals provided therapy in outpatient, residential, and methadone treatment programs in 1998, that 70% of the workforce were women, and that 53% had a graduate degree ( 7 , 13 ). Reported response rates were good (78% of facilities and 81% of practitioners), but respondents were self-selected ( 14 ). CSAT also surveyed treatment program directors, clinical supervisors, program counselors, and state directors to assess use of the Treatment Improvement Protocol publications ( 15 ); the response rate was strong (80%). Half of the respondents were women (51%), and most (80%) had at least a bachelor's degree. Facility directors (64%) and clinical supervisors (61%) were more likely than counselors (42%) to have a master's degree ( 15 ).
Counselors' opinions were examined in a survey of 317 individuals participating in the Delaware Valley Network of the CTN ( 16 ). Most of the respondents (80%) favored increased use of research-based treatments, but only about one in three supported the use of naltrexone (39%) or methadone maintenance (34%). Respondents with higher levels of education were less likely to support the use of confrontation and were more likely to support the use of medications ( 13 ). These items were also included in a survey of counselors in the Great Lakes Network of the CTN, and similar results were obtained ( 17 ). Workforce education and training, therefore, appear to be critical variables in facilitating adoption of evidence-based practices.
The CTN recognized that counselors, managers and clinical supervisors, and medical and support staff have important roles in the treatment of alcohol and drug disorders. Previous research focused on counselors and either did not provide information on medical and support staff or did not differentiate type of staff in the analysis. To characterize the CTN workforce and to build a database that could be used later to explore the associations between workforce characteristics and study outcomes, a survey of participating treatment programs and their staff was conducted. The study was initiated early in the development of the CTN, and three research centers and their treatment center partners were added after the study began. Three sets of trials were collecting data: buprenorphine detoxification (inpatient and outpatient), motivational interviewing and motivational enhancement therapy, and use of motivational incentives (contingency management) in outpatient and methadone treatment.
Methods
Drug abuse treatment organizations participating in the CTN were invited to complete organizational, treatment unit, and workforce surveys. Completed organizational surveys were obtained from 106 of 112 eligible community treatment programs (95% response rate). Treatment unit surveys were completed by 348 of the 384 units (91% response rate) listed in the organizational survey. Details on the organizational and treatment unit surveys are available from the corresponding author. The last item on the treatment unit survey asked for the names of employees in four job categories: counseling staff, medical staff, other staff with patient contact (including receptionists and aides), and management staff and clinical supervisors. Surveys were prepared for each person listed and distributed through local protocol coordinators.
Protocol coordinators
The 17 research centers participating in the CTN identified a protocol coordinator who oversaw study implementation in his or her network. Coordinators distributed invitations to complete the survey, monitored response rates, and encouraged local participation. The Oregon network led protocol implementation, trained and supported the coordinators, and served as the data management center.
Workforce survey
Sealed envelopes addressed to the individuals listed in the treatment unit survey were delivered to protocol coordinators. Coordinators negotiated the time and method of distribution with participating treatment programs. Most often the envelopes were distributed to recipients in staff meetings, and paper versions of the survey were completed at that time. Completed surveys were sealed in postage-paid reply envelopes. Respondents either mailed the form directly to the study's data management center or returned sealed envelopes to the protocol coordinator for batch return via overnight delivery services. Some programs distributed surveys through the corporate mail system. Respondents could also complete the survey on a secure Web site (17% completed the Web version). Confidential follow-up letters were mailed approximately four weeks later. Individuals who had completed the survey received a thank-you note; nonrespondents were reminded to complete and return the survey.
The survey requested information on years of experience in substance abuse treatment, education, training, licensing, credentials, and primary job title. Five-point Likert scales for 22 items assessed beliefs and opinions related to specific treatment approaches and interventions for alcohol and drug dependence (1, strongly disagree; 2, disagree; 3, neither agree nor disagree; 4, agree; 5, strongly agree). Items were drawn from previous work ( 16 , 18 ) or developed for this survey. Items were worded exactly as in the tables in this article.
Institutional review board
The Oregon Health and Science University Institutional Review Board (IRB) reviewed and approved study procedures. Local IRBs (N=40) also approved the protocol. Potential participants were given an information sheet describing the study, and completion of the survey was viewed as provision of informed consent; procedures were modified if a local IRB required a signed consent. Protocol coordinators stressed that programs and staff could decline to participate. Data collection began March 25, 2002, and extended to August 24, 2004, to allow programs that entered the CTN in January 2003 to participate. Because of delays associated with local and national IRB review and variation in the speed of data collection, time to complete the three surveys varied among the 17 networks.
Participant compensation
Participant compensation varied. Nine networks offered food (for example, pizza) during or after data collection, three provided gift certificates or a drawing for cash prizes, and one paid the programs—and the programs, in turn, handled staff compensation. Among the groups that provided compensation, the response rate was 77% (2,834 of 3,704). The four groups that did not offer compensation had a response rate of 58% (952 of 1,630).
Data analysis
Descriptive statistics were generated for demographic variables, and analysis of variance tested for differences by job category (counselor, manager or supervisor, medical staff, and support staff). An analysis of covariance assessed relationships between job category and treatment beliefs and opinions. Covariates were entered simultaneously with the dependent variable (type III sum of squares). Differences in opinions by job category were assessed in analyses that controlled for the effects of gender (woman or man), minority group (minority group or white non-Hispanic), modality (outpatient or residential), and education (high school or less, associate's or bachelor's degree, or graduate degree). Alpha was set at p<.01 for all analyses. Scheffé post hoc comparisons assessed differences among the four job categories and the three levels of education.
Results
Respondents
Staff rosters from the treatment unit survey listed 6,030 potentially eligible individuals. Men and women who left their position before distribution of the survey (N=313), who had no patient contact (N=313), were on a leave of absence (N=67), or who did not read English (N=3) were considered ineligible (total N=696), which left 5,334 potential respondents. Usable data were obtained from 3,786 individuals (71% of those eligible), including 1,757 counselors, 522 managers or supervisors, 511 medical personnel, and 908 support staff who had patient contact. The total includes 88 respondents with missing data on job category. Table 1 provides summary descriptive information for the four job categories.
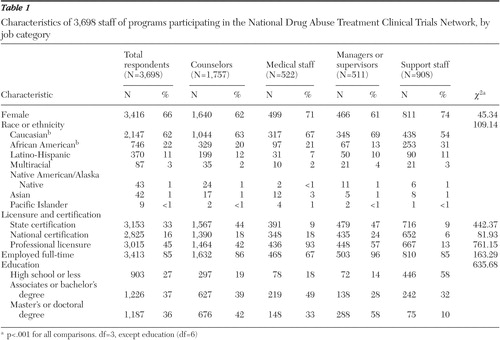 |
Two-thirds of the respondents were women (3,416 participants, or 66%). Women were more likely to occupy support positions (74%) and medical positions (71%) than counselor positions (62%) and manager-supervisor positions (61%). The group of participants was ethnically diverse: 746 were African Americans (22%), 87 were multiracial (3%), 42 were Asian-Pacific Islander (1%), and 43 were Native American (1%) (all non-Hispanic); an additional 370 participants (11%) noted a Latino-Hispanic ethnicity. Most participants (62%) were white non-Hispanic. African Americans were more likely to be working in support positions (33%) than in management or supervisor positions (15%). The highest proportion of Hispanics was found among counselors (12%) and the lowest proportion among medical staff (7%).
Full-time workers (35 or more hours per week) dominated the workforce ( Table 1 ). Medical personnel (66%) were least likely to be working full-time, and managers (96%) were most likely to be working full-time. Respondents reported a mean of 21.3±11.1 direct patient contact hours per week. Support staff had the most hours of patient contact per week (24.2±13.5) and managers-supervisors the least (14.7±9.9). The highest caseloads were found among counselors (23.5±18.4 patients) and medical staff (23.4±20.1); managers-supervisors had a mean caseload of 10.4±14.5 patients. Professional licensure was most common among medical staff (93%) and less common among managers (57%) and counselors (42%). Counselors and managers-supervisors had similar rates of state substance abuse certification (44% and 47%, respectively); managers-supervisors were more likely than counselors to have a national certification (24% and 18%, respectively).
Nearly three of four respondents reported either an associate's or bachelor's degree (1,226 respondents, or 37%) or a master's or doctoral degree (1,187 respondents, or 36%). Managers and counseling staff were more likely to have advanced degrees (58% and 42%, respectively), and a graduate degree was more common among counselors in outpatient settings (866 counselors, or 53%) than among residential counselors (734 counselors, or 30%). The most common master's degrees among counselors were social work (187 counselors, or 29% of counselors with masters degrees), counseling (175 counselors, or 27%), and psychology (138 counselors, or 22%). The 392 licensed medical staff included nurses (251 nurses, or 64%), physicians (77 physicians, or 20%), and nurse practitioners and physician assistants (32 staff, or 8%). Most support staff (58%) reported having a high school diploma (or less).
Knowledge, attitudes, and beliefs
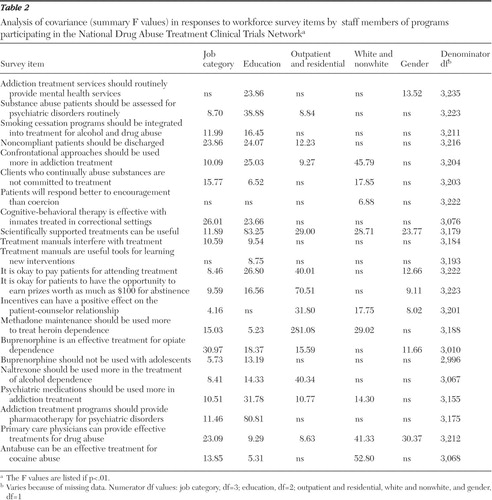
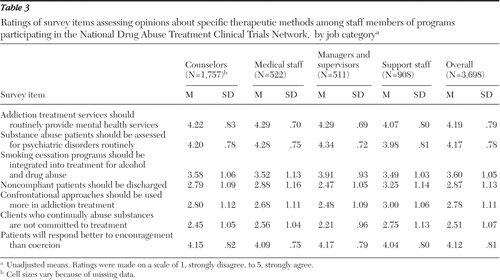
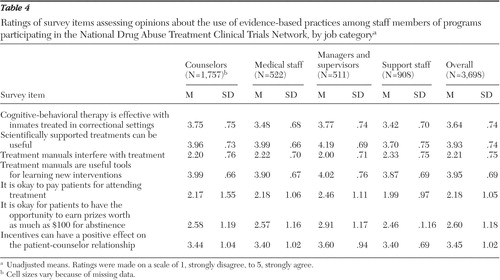
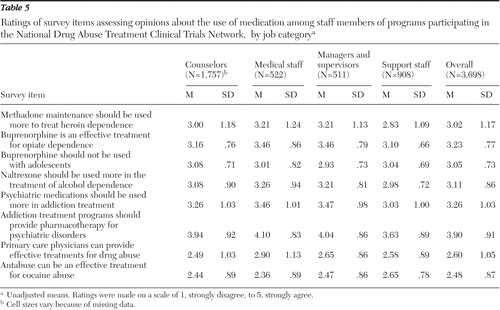
Survey items assessed opinions about specific practices and beliefs. Table 2 summarizes the analysis of covariance; F values are listed only if alpha is less than .01 for the independent variable or covariates. Unadjusted mean ratings for the four job categories are reported in Table 3 (therapeutic methods), Table 4 (specific evidence-based practices), and Table 5 (use of medications).
 |
 |
 |
 |
When the analysis controlled for the other independent variables, job category and education had statistically significant relationships with most of the items (19 and 20, respectively, of the 22 items). Managers-supervisors tended to have more positive opinions about specific evidence-based practices and more negative opinions about traditional beliefs. Medical staff had more positive opinions about the use of medications. Generally, individuals with graduate degrees had more positive opinions about evidence-based practices and more negative opinions about traditional beliefs. Respondents who worked in outpatient settings tended to be more supportive of pharmacotherapy and various behavioral interventions, whereas those in residential settings supported traditional beliefs. Level of care (outpatient or residential treatment) affected 13 of the items. Minority group and gender had independent relationships with fewer items (nine items and seven items, respectively).
Support was expressed for the routine delivery of mental health services and the assessment of psychiatric disorders within drug treatment programs. Univariate statistics are summarized in Table 2 , and Table 3 presents unadjusted mean ratings by job category. Women and individuals with more education indicated greater support for routine delivery of mental health services than those in the other categories examined. Individuals with more education had the highest level of support for routine psychiatric assessments. In addition, medical staff and managers-supervisors had more favorable opinions about routine assessment of psychiatric disorders and delivery of mental health services than did support workers. Personnel in outpatient settings were more supportive of routine assessment and treatment than those in residential programs.
Job category and education (support increased with education) was related to opinions about the integration of smoking cessation services into drug treatment. Managers-supervisors were more supportive than counselors, medical staff, and support staff. Individuals with graduate education were more supportive than their colleagues without degrees and those with undergraduate degrees. Three treatment beliefs were also related to job category: that drug use indicates a lack of treatment readiness, that confrontation should be used more often, and that noncompliant patients should be discharged. Individuals in support roles were consistently more supportive of these statements than managers-supervisors. Respondents from racial and ethnic minority groups regardless of job category were less likely to disagree with the use of confrontation and with discharge of patients who continue to use drugs. Staff in residential programs tended to support the use of confrontation and discharge of noncompliant patients. Individuals with more education disagreed more strongly with the statements.
Table 4 lists the unadjusted mean ratings of specific behavioral therapy approaches. Individuals with more education were more likely to agree (or disagree) with each statement. Managers-supervisors and counselors were more likely than medical and support staff to agree that "Cognitive-behavioral therapy is effective with inmates treated in correctional settings." Managers-supervisors were also more likely to support the statement "Scientifically supported treatments can be useful" (support workers had the lowest level of agreement); also more supportive were outpatient staff (compared with residential staff), men (compared with women), and whites (compared with other racial-ethnic groups). Conversely, managers were the least supportive and support staff the most supportive of the statement "Treatment manuals interfere with treatment" (those with more education had lower levels of agreement). For the converse of this item, "Treatment manuals are useful tools for learning new interventions," the level of support was primarily related to education (support increased with years of education).
Items assessing the use of contingency management received lower levels of support. Practitioners in outpatient settings were less negative than their counterparts in residential treatment programs. Respondents disagreed most with the statement "It is okay to pay patients for attending treatment." Less likely to disagree were managers (compared with other job categories), men (compared with women), and respondents with graduate degrees (compared with those with undergraduate degrees and no degrees). Respondents tended to disagree with the statement "It is okay for patients to have the opportunity to earn prizes worth as much as $100 for abstinence." Managers, men, and respondents with a graduate degree were less likely to disagree. Modest levels of support were shown for the final item, "Incentives can have a positive effect on the patient-counselor relationship"; nonwhite respondents were more positive than non-Hispanic whites.
Table 5 presents data on beliefs about the use of medications. Generally, individuals with more education were more supportive of using medication to treat alcohol and drug disorders. Job category also had a consistent association; medical personnel and managers-supervisors were more likely to support use of medications in treatment plans. Support levels, however, tended toward neutrality in the response scale, which suggested that opinions about the use of medication were not well developed. Medical staff and managers, for example, were more likely than counselors and support staff to agree with the item "Methadone maintenance should be used more in the treatment of heroin dependence"; levels of agreement were also higher among nonwhites, individuals with more formal education, and staff in outpatient settings. Similarly, levels of support for the item "Buprenorphine is an effective treatment for opioid dependence" were only slightly above the midpoint of the scale; agreement was strongest among medical staff and managers, respondents with more education, and individuals in outpatient settings. Responses to the item "Buprenorphine should not be used with adolescents" suggest uncertainty; the strongest association was a negative relationship with education—individuals with a graduate degree were less likely to support the statement. There was little support for the statement that "Naltrexone should be used more in the treatment of alcohol dependence"; outpatient staff and individuals with a graduate degree were more positive. Agreement with the statement "Psychiatric medications should be used more in addiction treatment" was also weak; support increased with education and was higher among medical staff and managers-supervisors. White non-Hispanic respondents were also more supportive than nonwhites. Conversely, there was stronger agreement that "Addiction treatment programs should provide pharmacotherapy for psychiatric disorders." Support increased with education and was highest among medical staff. Conversely, there was disagreement with the statement that "Primary care physicians can provide effective treatments for drug abuse"; nonwhites and men were less likely to disagree than white non-Hispanic staff and women, respectively; more supportive were medical staff (compared with support staff) and individuals with graduate training (compared with those without graduate degrees).
Discussion
Drug abuse treatment programs participating in the CTN have a multifaceted workforce. In the sample surveyed in this study, two-thirds of the employees were women, 38% had a master's or doctoral degree, and 34% were from racial or ethnic minority groups. Graduate degrees were more common among counselors and managers; 42% of the total counselor workforce and 58% of the outpatient counselors had a master's or doctoral degree. A national survey of outpatient counselors ( 13 ), the National Treatment Center Study ( 12 ), and the CSAT survey of counselors and program directors ( 15 ) reported similar rates of counselors with graduate degrees and of women in the workforce. The characteristics of the CTN workforce, therefore, seem to be consistent with data from previous assessments of the clinical workforce.
One workforce aspect that may be unexpected was the relatively high proportion of medical staff (14% of the respondents). Many alcohol and drug treatment services do not have medical personnel. However, the proportion of participating treatment programs affiliated with medical settings (25%) in the CTN is substantially higher than that reported in the National Survey of Substance Abuse Treatment Services (N-SSATS) (2%) and reflects the CTN's linkages with medical schools and medical centers ( 19 ). The CTN also has a lower proportion of freestanding alcohol and drug treatment centers than N-SSATS (53% compared with 61%). As a result, programs affiliated with the CTN are more likely to have medical staff. Moreover, most counselor surveys have not included medical and support staff as respondents. Therefore, the actual number of nurses, physicians, and physician assistants-nurse practitioners in drug abuse treatment centers is unknown.
Support for evidence-based practices
An unexpected range of support for science-based approaches to treatment was observed among the four broad job categories (counselor, manager-supervisor, medical staff, and support staff). Generally, when education, gender, and race were controlled statistically, managers-supervisors were most likely to indicate agreement with statements advocating greater use of treatment innovations. Conversely, support staff expressed significantly less enthusiasm for these techniques and were more likely to support confrontation and coercion. Although support personnel do not provide counseling services, responses to the workforce survey suggest that they make up 24% of the CTN workforce and have more hours of direct patient contact than do counselors and medical personnel. Their lack of support for evidence-based practices, therefore, could inhibit the introduction and effectiveness of contemporary science-based treatment strategies. Treatment programs that are initiating changes in therapeutic approaches may benefit from including all employees and not just counselors in training and organizational change efforts.
Training alone, however, does not ensure adoption of new practices ( 20 ). New practices are most likely to be sustained and maintained when administrative support (resources and leadership) is provided in the work setting, when coaching and consultation are provided on an ongoing basis, and when mechanisms are in place to give staff feedback on fidelity to the expected model ( 20 , 21 ). At this stage of development, the CTN is conducting a limited number of trials in selected sites. The CTN is not attempting to systematically influence counselors' use of evidence-based practices and is not providing training, coaching, and feedback, except within the context of trials.
As expected from research on technology transfer ( 22 ), acceptance of new practices was found to be strongly correlated with education. Therefore, continued increases in the number of counselors with graduate degrees should lead to more support for evidence-based practices. However, there are few data on the content of many counselor training programs and the extent to which they incorporate science-based therapies. Support personnel, moreover, tend to be high school graduates without college degrees and may have more influence on patients because they are more similar to the patients.
The survey found only modest levels of support for the use of medications to treat alcohol and drug problems. There was moderate support for increased use of methadone (about 35% of the respondents agreed or agreed strongly) and less support for buprenorphine for opioid dependence among adults (28% agreement) or adolescents (14% agreement). Support for greater use of naltrexone for the treatment of alcohol dependence was weak (29%). Most respondents, moreover, seemed to be unaware of recent research suggesting that disulfiram may be effective for treating cocaine dependence ( 23 ) (only 7% agreed with the statement). Apparently, many individuals working in programs participating in the CTN are not learning of findings from the latest research. The CTN and the field of drug abuse treatment have much work to do before the use of medication becomes a routine part of treatment plans. The good news is that opinions were not strongly negative, and education and training appear to promote more positive opinions. Participation in trials may also be influential. Individuals working in clinics that implemented the buprenorphine trials were significantly more likely than staff in other clinics to agree that "Buprenorphine is an effective treatment for opiate dependence" (3.4±.8 versus 3.2±.8; F=7.8, df=1 and 3,156, p<.01).
Responses were also neutral in regard to the use of contingency management strategies. Although a majority of staff endorsed a statement that incentives can support relationships between patients and counselors, only a minority concurred that it is appropriate to pay patients for attendance or that prizes should be awarded for abstinence. Contingency management techniques are gaining acceptance but remain controversial. It appears that the way in which the use of contingency management is framed may influence opinions—that is, incentives to support therapeutic alliances are more acceptable than payments for abstinence. Moreover, employees of clinics that participated in the contingency management trials were more likely than employees of nonparticipating clinics to agree with the statement that specifically addressed the opportunity to win prizes for abstinence (3.2±1.1 versus 2.6±1.2; F=75.1, df=1 and 3,386, p<.001). Although these differences are based on small numbers and could have preceded the initiation of the contingency management trials, the difference supports the notion that participation in a clinical trial and experience with the intervention can influence opinions.
Systematic efforts may be required to overcome the field's reluctance to embrace medications and contingency management as part of treatment plans. Models to promote the adoption of pharmaceutical therapies ( 24 , 25 ) and behavioral therapies ( 21 ) have been proposed and need to be applied and tested. The CTN may be an excellent venue for these applications.
Limitations
With more than 3,700 respondents and a 71% response rate, the CTN workforce survey may be the most extensive assessment of staff working in alcohol and drug abuse treatment programs. However, programs participating in the CTN are not a random sample of drug abuse treatment providers; programs were selected because of their capacity and willingness to participate in research trials and are disproportionately affiliated with medical centers. As a result, the programs and the workforce are likely to be more research and medically oriented. The relatively weak support for evidence-based practices in this select group of treatment programs highlights the challenge of promoting widespread adoption of these therapies.
Moreover, the data are cross-sectional and reflect one moment in time. Findings, however, are consistent with those of previous studies. The large number of respondents and the diversity of the participating programs suggest that the results provide useful insights into the contemporary addiction treatment workforce.
Conclusions
The National Drug Abuse Treatment Clinical Trials Network was designed in part to foster the adoption of treatment innovations. It will be useful to continue to monitor community treatment programs and the opinions of individuals working in participating programs to determine whether opinions change over time. The initial analysis of the CTN workforce suggests that manager-supervisors can play lead roles in promoting the adoption of evidence-based practices and tend to be the most supportive of these practices. Efforts to facilitate the use of evidence-based practices, however, need to recognize the heterogeneity of the addictions workforce. Although the proportion of staff with graduate degrees has increased over time, individuals without graduate degrees are still a dominant influence in the workforce. Change efforts, therefore, should address and engage support and medical staff as well as counselors and managers.
Acknowledgments and disclosures
The following cooperative agreements from the National Institute on Drug Abuse supported the design, distribution, collection, and analysis of the organizational, treatment unit, and workforce surveys within the CTN at the following nodes: California-Arizona, U10-DA15815; Delaware Valley, U10-DA13043; Florida, U10-DA13720; Great Lakes, U10-DA13710; Long Island, U10-DA13035; Mid-Atlantic, U10-DA13034; New England, U10-DA13038; New York, U10-DA13046; North Carolina, U10-DA13711; Northern New England, U10-DA15831; Ohio Valley, U10-DA13732; Oregon, U10-DA13036; Pacific, U10-DA13045; Rocky Mountain, U10-DA13716; South Carolina, U10-DA13727; Southwest, U10-DA15833; and Washington, U10-DA13714. The Center for Health Research of Kaiser Permanente developed the Web-based instrumentation, coordinated data collection, and facilitated data analysis; the authors are grateful to center staff Kimberly Funkhouser, B.S., Suzanne Gillespie, M.S., and Clifton Hindmarsh, B.S. The authors appreciate the support and participation of executive directors, treatment unit directors, and employees. They are especially grateful to the following individuals for assistance with distribution and collection of data: Ellen Silber, B.B.A., Arthur Alterman, Ph.D., Doreen Cardillo, Susan Gordon, Ph.D., Dan Santistiban, Ph.D., Val Jackson, M.S., LuAnn Beamer, Ph.D., Michael Liepman, M.D., Eva Kourniotis, M.S., Jennifer Lima, M.P.H., Shanna Coan, B.S., Kay Debski, B.S., Patrick McAuliffe, M.B.A., Paul McLaughlin, M.A., Patricia Novo, M.P.A., Agatha Kulaga, M.S.W., Melissa Chu, M.S., Terry Leon, R.M.A., Larry Taub, C.S.W., Jill Anderson, M.S., Jennifer Sharpe Potter, Ph.D., Irene Janis, B.A., Angela Casey-Willingham, B.A., Eugene Somoza, M.D., Ph.D., Mitch Greenlick, Ph.D., Lynn Kunkel, M.A., Anna Sosnowski, B.A., Al Hasson, M.S.W., Allison Ober, L.C.S.W., Reggie Gladney, Susan Quello, Royce Sampson, M.S.N., Mikyta Daughtery, Robert J. Meyers, Ph.D., and Dan Kivlahan, Ph.D.
The authors report no competing interests.
1. National Drug Abuse Treatment Clinical Trials Network. Bethesda, Md, National Institute on Drug Abuse. Available at www.drugabuse.gov/CTNGoogle Scholar
2. Amass L, Ling W, Freese TE, et al: Bringing buprenorphine-naloxone detoxification to community treatment programs: the NIDA Clinical Trial Network field experience. American Journal on Addictions 13 (suppl 1):S42-S66, 2004Google Scholar
3. Ling W, Amass L, Shoptow M, et al: A multi-center randomized trial of buprenorphine-naloxone versus clonidine for opioid detoxification: findings from the National Institute on Drug Abuse's Clinical Trial Network. Addiction 100:1090-1100, 2005Google Scholar
4. Carroll KM, Ball SA, Nich C, et al: Motivational interviewing to improve treatment engagement and outcome in individuals seeking treatment for substance abuse: a multisite effectiveness study. Drug and Alcohol Dependence 81:301-312, 2006Google Scholar
5. Peirce JM, Petry NM, Stitzer MC, et al: Effects of lower-cost incentives on stimulant abstinence in methadone maintenance treatment: a National Drug Abuse Treatment Clinical Trials Network Study. Archives of General Psychiatry 63:201-208, 2006Google Scholar
6. Petry NM, Peirce JM, Stitzer ML, et al: Prize-based incentives increase retention in outpatient psychosocial treatment programs: results of the National Drug Abuse Treatment Clinical Trials Network Study. Archives of General Psychiatry 62:1148-1156, 2005Google Scholar
7. Changing the Conversation: Improving Substance Abuse Treatment: The National Treatment Plan Initiative. DHHS pub no SMA-00-3479. Rockville, Md, Substance Abuse and Mental Health Services Administration, 2000Google Scholar
8. Partners for Recovery. Rockville, Md, Substance Abuse and Mental Health Services Administration. Available at partnersforrecovery.samhsa.gov/leadershipinstitutes.htmlGoogle Scholar
9. Annapolis Coalition on the Behavioral Health Workforce. Available at www.annapoliscoalition.org/about.phpGoogle Scholar
10. Camp JM, Kurtz NR: Redirecting manpower for alcoholism treatment, in Prevention, Intervention and Treatment: Concerns and Models. Edited by de Luca J. DHHS pub no ADM-1192 ed. Bethesda, Md, National Institute on Alcohol Abuse and Alcoholism, 1982Google Scholar
11. Mulligan DH, McCarty D, Potter D, et al: Counselors in public and private alcoholism and drug abuse treatment programs. Alcoholism Treatment Quarterly 6:75-89, 1989Google Scholar
12. Johnson JA, Knudsen HK, Roman PM: Counselor turnover in private facilities. Frontlines: Linking Alcohol Services Research and Practice, Nov 2002, pp 5, 8Google Scholar
13. Harwood HJ: Survey on Behavioral Health Workplace. Frontlines: Linking Alcohol Services Research and Practice, Nov 2002, p 3Google Scholar
14. The Clinical Workforce in the Substance Abuse Treatment System. Fairfax, Va, Lewin Group, 2001Google Scholar
15. Mulvey KP, Hubbard S, Hayashi S: A national study of the substance abuse treatment workforce. Journal of Substance Abuse Treatment 24:51-57, 2003Google Scholar
16. Forman R, Bovasso G, Woody GE: Staff beliefs about addiction treatment. Journal of Substance Abuse Treatment 21:1-9, 2001Google Scholar
17. Arfken CL, Agius E, Dickson MW, et al: Clinicians' beliefs and awareness of substance abuse treatments in research and nonresearch-affiliated programs. Journal of Drug Issues 35:547-558, 2005Google Scholar
18. Lehman WEK, Greener JM, Simpson DD: Assessing organizational readiness for change. Journal of Substance Abuse Treatment 22:197-209, 2002Google Scholar
19. National Survey of Substance Abuse Treatment Services: 2004 Data on Substance Abuse Treatment Facilities. Rockville, Md, Substance Abuse and Mental Health Services Administration, 2005Google Scholar
20. Fixsen DL, Naoom SF, Blase KA, et al: Implementation Research: A Synthesis of the Literature. Tampa, Fl, University of South Florida, Louis de la Parte Florida Mental Health Institute, National Implementation Research Network, 2005Google Scholar
21. Simpson DD: A conceptual framework for transferring research to practice. Journal of Substance Abuse Treatment 22:171-182, 2002Google Scholar
22. Rogers EM: Diffusion of Innovations, 5th ed. New York, Free Press, 2003Google Scholar
23. Carroll KM, Fenton LR, Ball SA, et al: Efficacy of disulfiram and cognitive behavior therapy in cocaine-dependent outpatient. Archives of General Psychiatry 61:264-272, 2004Google Scholar
24. Thomas CP, Wallack S, Lee SS, et al: Research to practice: factors affecting the adoption of naltrexone in alcoholism treatment. Journal of Substance Abuse Treatment 24:1-11, 2003Google Scholar
25. Thomas CP, McCarty D: Adoption of drug abuse treatment technology in specialty and primary care settings, in Immunotherapies and Depot Medications for the Treatment and Prevention of Drug Dependence. Edited by Harwood HJ. Washington, DC, National Academies Press, 2004Google Scholar



