Routine Laboratory Screening Among Newly Admitted Psychiatric Patients: Is It Worthwhile?
Medical illnesses are common (27% to 80%) among patients presenting with psychiatric symptoms ( 1 ). The aim of medical screening is to identify patients who should not be treated in a psychiatric inpatient ward because they have a serious and unstable comorbid medical condition in addition to a primary psychiatric disorder or because they have a primary medical condition or substance use disorder with secondary psychiatric symptoms ( 1 ). Other relevant goals of medical screening are to identify comorbid medical conditions and adverse effects of psychotropic medications, to determine the need to obtain medical consultations, to examine key risk factors in the population, and to assess the general health of the patient.
Despite the high comorbidity of medical illnesses among psychiatric patients, it is not clear which tests should be performed for newly hospitalized psychiatric patients. The guidelines published by the American Psychiatric Association (APA) in 2002 ( 2 ) recommended as part of the routine procedure during psychiatric emergency admissions "a comprehensive metabolic panel, complete blood count with differential, thyroid screening panel, urine toxicology, screening test for tertiary syphilis, psychiatric medication levels, and other studies as appropriate, based on the patterns of illness in the patients served." The APA has also issued specific recommendations for psychiatric disorders, such as schizophrenia, major depressive disorder, and bipolar disorder. However, in its most recent guideline for the psychiatric evaluation of adults ( 3 ), the APA states that "there are no specific guidelines about which tests should be 'routinely' done," and that "the potential utility of a test will be determined by multiple interrelated factors." According to the APA guideline ( 3 ) these factors include the likelihood that an individual from a population of similar patients (for example, of similar age, gender, or treatment setting) would have the condition (that is, the prevalence of the condition in that population); the probabilities that the test will correctly detect a condition that is present (true positive), incorrectly identify a condition as present when it is not (false positive), correctly identify a condition as absent (true negative), or incorrectly identify a condition as absent when it is actually present (false negative); and the treatment implications of the test results.
The aim of the study presented here was to compare the prevalence of abnormal results of laboratory tests routinely performed among newly hospitalized psychiatric patients in the hospital setting and the cost-effectiveness of such tests.
Methods
The design of the study is a retrospective chart review of 510 patients admitted to the Psychiatric Brief Hospitalization Unit at Puerta de Hierro Hospital (Madrid, Spain), from January 2000 to December 2005. We reviewed all the patients' charts and recorded the results of the routine laboratory tests that were performed upon admission. We recorded psychiatric diagnoses upon discharge according to ICD-9 criteria.
The research was reviewed and approved by a duly constituted ethics committee and by the hospital medical director.
To estimate cost-effectiveness, we examined the prevalence of values outside the normal range for all the tests. For all the laboratory tests, we compared the number needed to screen to find one abnormal result (NNSAR=1/prevalence of abnormal results in the studied population) and the direct cost spent to find one abnormal result (DCSAR=NNSAR × direct cost per test). The results are presented in international dollars of 2000 (I$). An I$ has the same purchasing power as the U.S. dollar has in the United States. Costs in local currency units are converted to I$ using purchasing power parity exchange rates developed by the World Health Organization ( 4 ). Confidence intervals were calculated using Wald's method ( 5 ).
Results
Among the participants, 265 (52%) were male and 245 (48%) were female. The mean±SD age was 40.1±15.6 years. Clinical variables of the study participants are presented in Table 1 . Schizophrenia, schizotypal, and delusional disorders and mood disorders were the most frequent diagnostic blocks in the sample.
 |
The prevalence of values outside the normal range, NNSAR values, and DCSAR values are presented in Table 2 . The prevalence of values outside the normal range ranged from 1% for free thyroxine (FT4) to 36% for total cholesterol. The NNSAR ranged from 2.8 for total cholesterol to 127.3 for FT4. The DCSAR ranged from .38 I$ for chloride to 402.27 I$ for FT4.
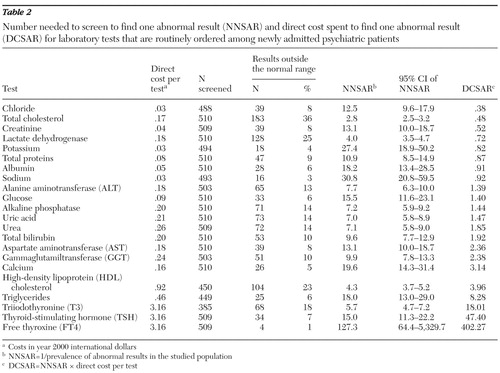 |
The highest rates of abnormal values were for total cholesterol (36%), lactate dehydrogenase (25%), and high-density lipoprotein (HDL) cholesterol (23%).
Discussion
Several authors have warned of the dangers of ubiquitous, unselective screening ( 1 , 6 ). According to the APA one of the factors that should determine the clinical utility of a test is the prevalence of the condition in the study population ( 3 ). The prevalence of abnormal values was quite high for some of the laboratory tests, such as total cholesterol (36%), lactate dehydrogenase (25%), and HDL cholesterol (23%), and therefore the NNSARs were low (2.8, 4.0, and 4.3, respectively). In contrast, the prevalence of abnormal values was quite low for other laboratory tests, such as FT4 (1%) or sodium (3%), and therefore the NNSARs are high (127.3 and 30.8, respectively).
When estimating the cost-effectiveness of laboratory tests among newly admitted psychiatric patients, one should take into account not only the direct cost per test but also the prevalence of abnormal results in that population. The population of psychiatric inpatients differs considerably from the general population in terms of sociodemographic characteristics, risk factors, pharmacological treatments, prevalence of laboratory abnormalities, and comorbid medical diseases. Therefore, we could not compare our results with those of similar studies performed in the general population. Unfortunately, there is limited information regarding laboratory findings among hospitalized psychiatric patients. Most of the reports focus on patients with a specific diagnosis, such as schizophrenia ( 7 ).
In one of the most recent studies that included all patients admitted to a psychiatric emergency facility during one month (N=214), the prevalence of laboratory values outside the normal range was much higher than those found in our study for some tests (glucose, 34% versus 7% in our study; gammaglutamiltransferase, 29% versus 10%; alanine aminotransferase, 38% versus 13%; aspartate aminotransferase, 34% versus 8%; sodium, 10% versus 3%; potassium, 16% versus 4%) ( 8 ). There were similarities in the age and gender distribution in Schillerstrom and colleagues' study ( 8 ) and our sample; however, the findings were different. The differences may be explained by the fact that the laboratory values in Schillerstrom and colleagues' study were obtained in the emergency setting. Moreover, in Schillerstrom and colleagues' study 35 patients (16%) experienced acute agitation and received intramuscular medication and 35 patients (16%) tested positive for alcohol. The prevalence of abnormal thyroid function values in our sample was similar to the figures reported in the literature.
The high prevalence of abnormal HDL cholesterol and total cholesterol levels among our study participants may be related to metabolic syndrome, which is prevalent among psychiatric patients, particularly among those diagnosed as having schizophrenia ( 7 ) or depression ( 9 ). It would be of interest to examine the other criteria for metabolic syndrome among patients in our study—for example, central obesity, elevated triglycerides, elevated blood pressure, and elevated fasting plasma glucose. However, we only had data on triglycerides and fasting plasma glucose, which indicated low rates of abnormal values (6% for triglycerides and 6% for fasting plasma glucose). Moreover, both high and low levels of total cholesterol and low levels of HDL cholesterol have been linked to depression and suicide ( 10 ), and an increase in total cholesterol levels has been observed among patients with depression after treatment with antidepressants, mood stabilizers, or both ( 11 ).
Most of the tests have DCSAR values less than 2.00 I$, but some tests have much higher DCSAR values, such as FT4 (402.27 I$) or thyroid-stimulating hormone (TSH) (47.40 I$). The direct cost per test ranges from .03 I$ for sodium, chloride, and potassium to 3.16 I$ for FT4, triiodothyronine (T3), and TSH. The absolute differences in the direct cost per test are small (range of 3.13 I$), but the differences in the DCSAR are much larger (range of 401.89 I$).
Because there are no clear guidelines regarding the tests that should be performed among newly admitted psychiatric patients and because there are no prospective studies assessing the long-term benefits of screening in this population, it may be argued that the differences in the prevalence of abnormal test results and in the direct cost of the different tests might be used when deciding whether or not to perform a test. However, it should not be forgotten that the costs derived from some undetected alterations (such as altered thyroid function tests) may be much higher than the direct costs of detecting a single case (DCSAR). For example, among psychiatric patients lower levels of thyroid hormones and higher levels of TSH have been associated with a poorer response to treatment (that is, longer time to remission) ( 12 ) and longer hospital length of stay ( 13 ). Relative hypothyroidism may play a role in the development of some treatment-resistant depressive disorders ( 14 ). The DCSARs for TSH and FT4 are 47.40 I$ and 402.27 I$, respectively, but the costs of additional days of hospital stay may be much higher (189.92 I$ per hospital bed per day according to the World Health Organization; data available at www.who.int/choice/country/esp/cost/en/index.html).
The question of whether it is worthwhile to perform TSH tests for every psychiatric patient and spend 47.40 I$ to find one person with results outside the normal range, compared with spending .48 I$ to find a psychiatric patient with abnormal total cholesterol, should be answered by future prospective research. However, it is our opinion that the costs of finding one patient with abnormal results are quite reasonable for most of the tests, compared with the potential costs of missing the diagnosis of a treatable medical condition.
In order to compare the cost-effectiveness of all the different laboratory tests, we have used the concepts of NNSAR and DCSAR. We are aware that cost-effectiveness estimation is far more complex than that and is influenced by many other factors. In order to evaluate the cost-benefit ratio of laboratory function tests among psychiatric patients, we would need to know the costs derived from each undetected laboratory test alteration and the potential benefits of an early diagnosis followed by adequate treatment. A new statistic has already been developed to compare the efficacy of screening strategies: the number needed to screen (NNS, defined as the number of people who need to be screened for a given duration to prevent one death or adverse event) ( 15 ). The NNS is somewhat similar to the number needed to treat (NNT, defined as the number of people who need to be treated for a given duration to prevent one death or one adverse event and calculated as the reciprocal of the absolute risk reduction), which is a widely known statistic that was developed to compare the clinical benefit of different treatments. However, because we lacked follow-up data of the study participants regarding deaths and adverse events and because the screening was performed in a cross-sectional manner, we decided to use the NNSAR and the DCSAR, which provide an estimate of the comparative cost-effectiveness of each laboratory test regarding only direct costs.
Our study has limitations. First, we lacked information regarding the number of patients for whom positive screens identified treatable problems and the costs of the interventions that were provided. There were no data available regarding the cost of missed abnormalities in the laboratory tests—for example, days of additional hospital stay and unnecessary or inadequate treatment. Second, the sample was small and limited to one hospital. Finally, the costs of tests may vary across sites and countries. Therefore, the results of the study presented here should be regarded as a preliminary contribution to the calculation of cost-effectiveness of routine screening among psychiatric patients.
Conclusions
When estimating the cost-effectiveness of laboratory tests, one should take into account not only the direct cost per test but also the prevalence of abnormal results in the population.
Our study found large differences in the prevalence of abnormal test results (NNSAR) and cost-effectiveness (DCSAR) of laboratory tests routinely performed among newly admitted psychiatric patients. The benefits of routine laboratory screening of newly admitted psychiatric patients need to be evaluated in prospective studies that include data about deaths, adverse events, the costs derived from each undetected laboratory test alteration, and the potential benefits of early diagnosis followed by adequate treatment.
Acknowledgments and disclosures
This article was supported by grant FIS I060092 and grant RD06/0011/0016 from the Fondo de Investigacion Sanitaria (FIS) and by the Conchita Rabago Foundation and the Harriet and Esteban Vicente Foundation.
Dr. Baca-Garcia is the Lilly Suicide Scholar at Columbia University, New York. The other authors report no competing interests.
1. Gregory RJ, Nihalani ND, Rodriguez E: Medical screening in the emergency department for psychiatric admissions: a procedural analysis. General Hospital Psychiatry 26:405–410, 2004Google Scholar
2. Allen MH, Forster P, Zealberg J, et al: Report and Recommendations Regarding Psychiatric Emergency and Crisis Services: A Review and Model Program Descriptions. Arlington, Va, American Psychiatric Association, APA Task Force on Psychiatric Emergency Services, 2002. Available at www.psych.org/edu/otherres/libarchives/ar chives/tfr/tfr200201.pdfGoogle Scholar
3. Vergare MJ, Binder RL, Cook IA, et al: Practice Guideline for the Psychiatric Evaluation of Adults, 2nd ed. Arlington, Va, American Psychiatric Association, 2006. Available at www.psych.org/psychpract/treatg/pg/PsychEval2ePG04-28-06.pdfGoogle Scholar
4. Purchasing Power Parity 2000. Geneva, World Health Organization. Available at www.who.int/choice/costs/ppp/enGoogle Scholar
5. Bender R: Calculating confidence intervals for the number needed to treat. Controlled Clinical Trials 22:102–110, 2001Google Scholar
6. Grimes DA, Schulz KF: Uses and abuses of screening tests. Lancet 359:881–884, 2002Google Scholar
7. De Hert M, Van Winkel R, Van Eyck D, et al: Prevalence of diabetes, metabolic syndrome and metabolic abnormalities in schizophrenia over the course of the illness: a cross-sectional study. Clinical Practice and Epidemiology in Mental Health 2:14, 2006Google Scholar
8. Schillerstrom TL, Schillerstrom JE, Taylor SE: Laboratory findings in emergently medicated psychiatry patients. General Hospital Psychiatry 26:411–414, 2004Google Scholar
9. Heiskanen TH, Niskanen LK, Hintikka JJ, et al: Metabolic syndrome and depression: a cross-sectional analysis. Journal of Clinical Psychiatry 67:1422–1427, 2006Google Scholar
10. Lester D: Serum cholesterol levels and suicide: a meta-analysis. Suicide and Life-Threatening Behavior 32:333–336, 2002Google Scholar
11. Gabriel A: Changes in plasma cholesterol in mood disorder patients: does treatment make a difference? Journal of Affective Disorders 99:273–278, 2007Google Scholar
12. Cole DP, Thase ME, Mallinger AG, et al: Slower treatment response in bipolar depression predicted by lower pretreatment thyroid function. American Journal of Psychiatry 159:116–121, 2002Google Scholar
13. Abulseoud O, Sane N, Cozzolino A, et al: Free T4 index and clinical outcome in patients with depression. Journal of Affective Disorders 100:271–277, 2007Google Scholar
14. Hickie I, Bennett B, Mitchell P, et al: Clinical and subclinical hypothyroidism in patients with chronic and treatment-resistant depression. Australian and New Zealand Journal of Psychiatry 30:246–252, 1996Google Scholar
15. Rembold CM: Number needed to screen: development of a statistic for disease screening. British Medical Journal 317:307–312, 1998Google Scholar



