Executive Function and Employment Status Among Veterans With Bipolar Disorder
Bipolar disorder is a chronic illness with substantial psychosocial and occupational morbidity. Studies have documented that functional impairment—including unemployment—persists among many patients with bipolar disorder despite mood stabilization ( 1 , 2 , 3 , 4 , 5 ). Unemployment is often associated with personal devastation and poses a profound economic burden on society ( 6 ). Yet the reasons for persistent unemployment among patients with bipolar disorder remain unclear.
Factors other than mood episodes may contribute to poor occupational function ( 7 ). Impairment in executive functioning in schizophrenia is associated with poorer functional outcomes, including employment ( 8 , 9 , 10 ). Although persistent executive function deficits have been reported among some patients with bipolar disorder during euthymia ( 11 , 12 , 13 ), the impact, if any, of these deficits on the patients' occupational function has rarely been studied ( 13 , 14 , 15 ). The purpose of this study was to assess the association between neurocognitive function and occupational function by using data collected retrospectively from a large cohort of veterans with bipolar disorder. Employment status (employed versus unemployed) was used as a proxy measure of occupational function. We hypothesized that impairment in the executive domain would be associated with unemployment. This study represents an incremental advance in two ways. First, the sample was collected as part of a large, multisite effectiveness trial and thus sought to maximize enrollment of a heterogeneous population of patients with bipolar disorder, much like the population that would be seen in general clinical practices ( 16 ). Second, the relatively large sample allowed multivariate analyses to isolate neurocognitive effects specifically.
Methods
Data were collected between January 1, 1997, and December 31, 1999, from 306 patients with bipolar disorder, types I and II, who participated in an 11-site randomized controlled trial (Department of Veterans Affairs [VA] Cooperative Study 430: Reducing the Efficacy-Effectiveness Gap in Bipolar Illness) ( 16 , 17 ). The study was conducted to evaluate whether, for patients with bipolar disorder, an integrated, clinic-based treatment delivery system that emphasizes algorithm-driven somatotherapy, standardized patient education, and easy access to a single primary mental health care provider to maximize continuity of care could reduce weeks in affective episodes or hospitalization for affective episodes. This study was designed from the outset as an effectiveness study ( 16 , 17 ) and as such enrolled a sample with few exclusion characteristics so that it would resemble the population seen in general clinical practice.
The study was approved by the institutional review boards at all participating sites. Written informed consent was obtained from patients near the end of their inpatient hospitalization for a manic, major depressive, or mixed episode. A diagnosis of bipolar disorder was confirmed by using the Structured Clinical Interview for DSM-IV (SCID). Occupational information for the year before study entry was obtained retrospectively from the SCID and from one semistructured interview administered at or soon after discharge. On the basis of this information, patients were assigned to one of four categories reflecting their highest level of occupational function (employment) in the 12 months before admission. A participant was considered to be employed if he or she was working at a job, fulfilling domestic responsibilities in the home, or attending school. The four categories included full-time employment, part-time employment (less than 30 hours per week), unemployed for most of the year and not sure of being able to return to work, and unemployed and not expected to work. For the purposes of the study presented here, all patients with bipolar disorder younger than 55 years who were employed full- or part-time constituted the employed group, and those younger than 55 years who were unemployed and not expected to work constituted the unemployed group.
A total of 213 patients were in the final analysis. Of these, 99 (47%) were admitted for depression, 61 (29%) were admitted for mania, and 49 (23%) were admitted for mixed mood episodes. (Numbers do not total 213 because information was missing for four patients.) The distributions of patients with depression, mania, and mixed mood episodes at admission were not found to be significantly different between the employed and unemployed groups.
Because neuropsychological function was not a primary area of assessment for the goals of the VA Cooperative Study 430, a full neuropsychological battery was not obtained from patients in this study. However, executive function was assessed at the time of enrollment into the study by using a 22-item version of the Executive Interview (EXIT). The EXIT is a 15-minute structured interview that correlates well with other measures of executive cognitive function ( 18 ) and can be administered by lay personnel ( 19 ). The EXIT was designed as a quick, bedside clinical examination of executive cognitive function ( 19 ).The scale has been validated and used extensively to assess executive control function among patients with schizophrenia and dementia ( 20 , 21 , 22 ). The EXIT contains items that tap into a variety of executive cognitive domains, including perseveration, response set-switching, generation de novo of stories, generation of word lists, and executing tasks during interference. Clearly, such cognitive tasks may be quite relevant to adequate performance of work-related task. Many items are derived from existing instruments (for example, Luria hand sequences).The instrument differs from the Mini-Mental State Examination, which is highly memory oriented with few items directly testing executive function.
The score range of the 22-item EXIT is 0 to 40, with higher scores indicating greater executive impairment. The original 25-item EXIT has used a cutoff score of 15 to separate patients with dementia from those without dementia. The 22-item EXIT differed from the full 25-item EXIT only by the exclusion of the three items testing frontal release signs. These were excluded because such signs, while common in dementia, were not found among any nondemented patients with bipolar disorder in our pilot feasibility study ( 22 ). Healthy adults usually score 4 or less on the 25-item scale ( 23 ; Royall DR, personal communication, 2004). Thus for the 22-item scale, a score higher than 4 was chosen to identify, among nondemented individuals with bipolar disorder, those who had evidence of morbidity resulting from executive function deficits ( 23 ).
The main analysis was to assess whether neurocognitive status, as assessed by EXIT scores, was associated with employment status. However, we also looked at demographic variables (for example, age, gender, race, education, and marital status) and course-of-illness variables (for example, number of psychiatric hospitalizations, presence of psychosis at admission, and number of psychotropic medications) that might confound (explain) any association between EXIT scores and employment status. Bivariate analyses were used to assess the association of demographic, course-of-illness, and cognitive variables with employment status. One-way analysis of variance was used for the continuous variables, and chi square analysis was used for the categorical variables. The variables that showed statistically significant associations (p<.05) with employment status were entered into a correlation analysis to check for multicollinearity. This was followed by a stepwise multiple logistic regression to assess whether neurocognitive status as a predictor of employment still held up in the model. The dichotomous variable employment status was modeled as the response variable, and the variables significantly associated with employment status were entered as covariates.
Results
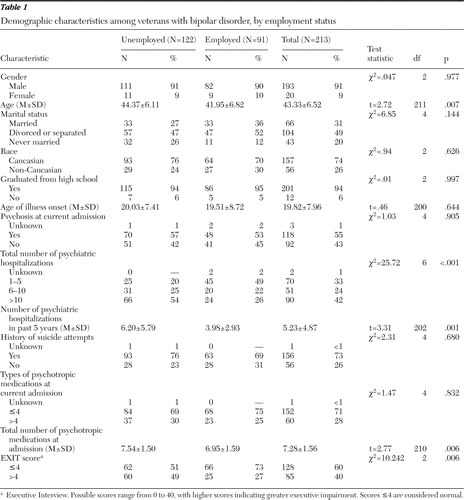
Table 1 depicts the demographic, neurocognitive (EXIT scores), and course-of-illness variables of the 213 patients, broken out by employment status with corresponding test statistics and p values. The results of the bivariate analyses indicated that five variables were significantly associated with unemployment. First, as predicted, there were significant between-group differences between the employed and unemployed groups for EXIT scores: 49% of the unemployed group scored greater than 4 on the EXIT compared with only 27% in the employed group (p=.006). Thus patients with poorer executive function performance as measured by the EXIT were significantly more likely to be unemployed. Additionally, compared with patients in the employed group, patients in the unemployed group were significantly older (p=.007), had a significantly greater number of total lifetime psychiatric hospitalizations (p<.001), had a significantly greater number of psychiatric hospitalizations in the past five years before participation in the study (p=.001), and were taking a significantly greater total number of psychotropic medications (p=.006). Therefore, we performed a multiple logistic regression using these variables as covariates to determine whether these variables were possible confounders that could explain the association between EXIT scores and employment status.
 |
First, the correlations among the five variables significantly associated with employment status were evaluated for multicollinearity. Mild correlations were present between EXIT scores and the three course-of-illness variables: total number of different psychotropic medications (r=.1), total number of psychiatric hospitalizations in the five years before participation in the study (r=.02), and total number of lifetime psychiatric hospitalizations (r=.14). Moderate correlations were present between EXIT scores and age (r=.33) and between the total number of psychiatric hospitalizations in the past five years and the total number of lifetime psychiatric hospitalizations (r=.4).
These five explanatory variables were next placed in a stepwise logistic regression model to determine the variables that were most significantly associated with employment status in a multivariate scenario. The logistic regression was run using employment status as the response variable with stepwise selection. The EXIT scores still held up in the model as a significant predictor of employment, even after the other significant covariates were entered. The variables that contributed in the model as the most significant factors to explain the occupational role function for individuals with bipolar disorder were the EXIT scores ( χ2 =5.72, df=1, p=.017), total number of psychotropic medications ( χ2 =4.63, df=1, p=.031), and total number of lifetime psychiatric hospitalizations resulting from psychiatric illness ( χ2 =14.23, df=1, p<.001). The overall model was also significant ( χ2 =31.91, df=3, p<.001). When used to predict the employment status of the same participants, the model could predict correctly for 72% of the participants. Age and number of psychiatric hospitalizations in the past five years were not significant predictors of employment status.
The logistic regression analysis demonstrated that a 1-point increase in the EXIT score increased the odds of being unemployed by 11% (OR=.89, 95% CI=.80–.97), conditional on the total number of lifetime psychiatric hospitalizations and the total number of different psychotropic medication types. Additionally, the use of one more psychotropic medications, irrespective of type, increased the odds of being unemployed by 20% (OR=.80, CI=.65–.98), conditional on EXIT score and the total number of lifetime psychiatric hospitalizations. Similarly, an increase in the total number of lifetime psychiatric hospitalizations by one hospitalization increased the odds of being unemployed by 50% (OR=.50, 95% CI=.35–.72), conditional on the other two factors.
Discussion
The study presented here supports an association between impaired executive functioning and impaired work functioning among patients with bipolar disorder. This suggests that persisting functional disability may result, at least in part, from persisting neurocognitive impairment. To our knowledge, our study of 213 patients with bipolar disorder is the largest study assessing the relationship between employment status and demographic, illness, and cognitive variables. In addition, this effectiveness sample had few exclusion criteria, supporting generalizability of these findings to patients with this disorder seen in similar general practice venues.
In our total sample of 213 patients, 122 (57%) were unemployed and 91 (43%) were employed at the time of hospitalization. These results in this VA population are consistent with prior studies reporting high rates of occupational impairment (unemployment) among patients with bipolar disorder ( 1 , 2 , 4 , 24 , 25 , 26 , 27 ). A series of studies have documented poor role-function adjustment among patients with bipolar disorder despite prophylactic mood stabilization ( 1 , 2 , 5 , 28 , 29 , 30 , 31 , 32 , 33 ). One study followed 67 patients with bipolar disorder after an admission for mania ( 1 ). Six months after admission 44 (67%) were successfully followed. Of these 44 persons, 80% were symptom free (symptomatically recovered), but only 43% were employed and only 21% were working at their expected level of employment (functionally recovered). Similarly, other studies following patients with bipolar disorder from six months up to 1.7 years after an index admission for mania have documented syndromal recovery with persistent functional disability in up to 60% ( 2 , 3 , 24 , 34 ). These observations and those of the study presented here suggest that factors other than the persistence of affective syndromes might contribute to persistent poor vocational and psychosocial functioning in a substantial subset of patients with bipolar disorder.
Several studies have demonstrated persistent cognitive impairment among patients with bipolar disorder after they have recovered symptomatically ( 35 , 36 , 37 , 38 ). More recent studies of neurocognitive functioning among patients with bipolar disorder in the euthymic state have continued to demonstrate impairment in executive function ( 11 , 39 , 40 , 41 ) or verbal memory ( 11 , 12 , 42 , 43 , 44 ), compared with a control group. Deficits in these two cognitive domains have been demonstrated to be strong predictors of poor functional outcome in schizophrenia ( 8 , 9 , 45 , 46 , 47 ).
Our study has several limitations. First, it involves a VA population that is also predominantly male. How these findings might generalize to the nonveteran population or to women with bipolar disorder remains to be studied. Second, employment status was assessed retrospectively with a semistructured interview, rather than prospectively with a more rigorous scale or set of criteria. Finally, executive function was assessed with a "bedside" executive function assessment that is not commonly used in the field to explore employment and cognition in psychiatric illness. Unfortunately, because the main variables of interest in the larger study were not employment or neuropsychological function, a more detailed neuropsychological battery was not administered. A more extensive cognitive assessment may have explained more functional outcome variance. However, the EXIT scores contributed significantly to the discrimination of the employed from the unemployed groups in this study, even though the majority of the unemployed group scored in the normal range on the test. Nonetheless, other measures addressing executive and other cognitive domains may have discriminated between the two employment groups better.
Although our study suggests that unemployed patients with bipolar disorder are significantly more likely than employed patients with bipolar disorder to score in the abnormal range on a measure of executive functioning, a third limitation is that we assessed only this one cognitive domain. We cannot be sure whether this is the only cognitive domain that would be found in the sample to be associated with employment status. The degree to which neurocognitive deficits overall and neurocognitive deficits specifically in the domain of executive functioning influence work outcomes among patients with bipolar disorder remains understudied. However, two recent studies have also reported that executive impairment is associated with functional impairment among euthymic patients with bipolar disorder ( 13 , 48 ). Future studies with more precise measures of occupational and role function and a more extensive neuropsychological battery that assesses multiple cognitive domains are warranted.
Total number of psychiatric hospitalizations and total number of psychotropic medications at the time of admission were also significantly associated with employment status—that is, patients who were unemployed had a significantly greater number of lifetime psychiatric hospitalizations and a significantly greater number of psychotropic medications at the time of admission. Odds ratios indicated that the lifetime number of psychiatric hospitalizations contributed the most among the three significant predictors of employment—namely, EXIT score, total number of psychotropic medications, and number of lifetime psychiatric hospitalizations—in explaining unemployment among the patient cohort in this study.
In some studies ( 2 , 3 , 24 , 32 , 49 ), but not all ( 30 , 31 ), course-of-illness variables (mean number of episodes per year, number of prior psychiatric hospitalizations, and presence of psychotic symptoms on index admission) have been found to predict poor functional outcome. This raises interesting questions about the interrelationships of these variables and unemployment. The exact (causal) path between cognitive impairment, number of psychiatric hospitalizations, and current unemployment remains unclear. Multiple psychiatric hospitalizations resulting from relapse could create an interrupted work history that damages hiring potential and ultimately leads to unemployability. Alternatively, repeated episodes of severe mania or depression (requiring hospitalization) may themselves be toxic to the brain ( 50 ) and may possibly cause further neurocognitive deficits with each subsequent episode. Relapse could thus more directly contribute to poor executive function, in that reduced executive capacity could be the result of multiple relapses. Yet another possibility is that a core premorbid deficit in executive control could result in overall poor planning and poor organization skills, which could not only directly lead to disability in the workforce but could lead to problems with medication compliance as well. The latter might subsequently result in relapse and frequent hospitalization. However, most participants were high school graduates and therefore presumably without significant premorbid cognitive dysfunction at least from ages 18 to 20.
The total number of different psychotropic medications each participant was prescribed was found to be significantly associated with employment in the bivariate analysis and also emerged as a significant predictor of employment when adjusted for the EXIT score and the total number of psychiatric hospitalizations in the multivariate analysis. Again, the causal direction is not clear. However, although it is possible that a greater number of psychotropic medications impaired executive function and thus employment, it is notable that executive function itself provided a unique contribution to reduced likelihood of employment.
Conclusions
Our results in this VA population of patients with bipolar disorder are consistent with prior studies reporting high rates of occupational impairment (unemployment) among patients with bipolar disorder ( 1 , 2 , 4 , 24 , 25 , 26 , 27 ). Very few studies have explored potential etiologies of functional impairment by systematically examining the subset of patients in whom it occurs. Our study suggests that patients with bipolar illness who have functional impairment are likely to also have executive neurocognitive impairment, have a greater number of lifetime psychiatric hospitalizations, and take a greater number of psychotropic medications, compared with those without functional impairment.
Our study in a large cohort of veterans with bipolar disorder highlights high rates of unemployment and an association between cognitive disability in the executive domain and unemployment, similar to that described among patients with schizophrenia ( 9 , 25 , 26 , 51 , 52 ). Whether executive impairment is primary and leads to both poor compliance and subsequent relapse or whether relapse and psychiatric hospitalization primarily contribute to the development of persistent executive impairment remains to be further studied. It is possible that both (number of psychiatric hospitalizations and executive dysfunction) contribute as two independent factors to poor occupational role function.
Despite the prevalence and cost of work disability and social dysfunction in both personal and societal terms, there is a paucity of information about the variables that contribute to these issues among patients with bipolar disorder. Persistent functional impairment is in the long term as important to patients and their families as remission of affective symptoms, if not more so. Future attempts to better understand how and among whom executive cognitive dysfunction occurs will provide a basis for intelligent intervention and rehabilitation.
Acknowledgments and disclosures
Funding for this project was provided by the Department of Veterans Affairs, Cooperative Study 430, Reducing the Efficacy-Effectiveness Gap in Bipolar Disorder.
Dr. Altshuler received grant and research support and honoraria from and served on a speaker's bureau and advisory board for Abbott; received honoraria from and served on an advisory board and speaker's bureau for Bristol-Meyers Squibb and Forest Laboratories; and received honoraria from and served on a speakers bureau for GlaxoSmithKline. Dr. Bauer served as a Data Safety Monitoring Board consultant for Repligen Corp. The other authors report no competing interests.
1. Dion GL, Tohen M, Anthony WA, et al: Symptoms and functioning of patients with bipolar disorder six months after hospitalization. Hospital and Community Psychiatry 39:652–657, 1988Google Scholar
2. Harrow M, Goldberg JF, Grossman LS, et al: Outcome in manic disorders: a naturalistic follow-up study. Archives of General Psychiatry 47:665–671, 1990Google Scholar
3. Tohen M, Waternaux CM, Tsuang MT: Outcome in mania: a 4-year prospective follow-up of 75 patients utilizing survival analysis. Archives of General Psychiatry 47:1106–1111, 1990Google Scholar
4. Suppes T, Leverich GS, Keck PE, et al: The Stanley Foundation Bipolar Treatment Outcome Network: II. demographics and illness characteristics of the first 261 patients. Journal of Affective Disorders 67:45–59, 2001Google Scholar
5. Coryell W, Scheftner W, Keller M, et al: The enduring psychosocial consequences of mania and depression. American Journal of Psychiatry 150:720–727, 1993Google Scholar
6. Wyatt RJ, Henter I: An economic evaluation of manic-depressive illness—1991. Social Psychiatry and Psychiatric Epidemiology 30:213–219, 1995Google Scholar
7. Bauer MS, Kirk GF, Gavin C, et al: Determinants of functional outcome and healthcare costs in bipolar disorder: a high-intensity follow-up study. Journal of Affective Disorders 65:231–241, 2001Google Scholar
8. Lysaker PH, Bell MD, Zito WS, et al: Social skills at work: deficits and predictors of improvement in schizophrenia. Journal of Nervous and Mental Disease 183:688–692, 1995Google Scholar
9. Green MF: What are the functional consequences of neurocognitive deficits in schizophrenia? American Journal of Psychiatry 153:321–330, 1996Google Scholar
10. McGurk SR, Mueser KT: Cognitive functioning, symptoms, and work in supported employment: a review and heuristic model. Schizophrenia Research 70:147–173, 2004Google Scholar
11. Altshuler LL, Ventura J, van Gorp WG, et al: Neurocognitive function in clinically stable men with bipolar I disorder or schizophrenia and normal control subjects. Biological Psychiatry 56:560–569, 2004Google Scholar
12. Van Gorp WG, Altshuler L, Theberge DC, et al: Cognitive impairment in euthymic bipolar patients with and without prior alcohol dependence: a preliminary study. Archives of General Psychiatry 55:41–46, 1998Google Scholar
13. Martinez-Aran A, Penades R, Vieta E, et al: Executive function in patients with remitted bipolar disorder and schizophrenia and its relationship with functional outcome. Psychotherapy and Psychosomatics 71:39–46, 2002Google Scholar
14. Zarate CA Jr, Tohen M, Land M, et al: Functional impairment and cognition in bipolar disorder. Psychiatric Quarterly 71:309–329, 2000Google Scholar
15. Dickerson FB, Boronow JJ, Stallings CR, et al: Association between cognitive functioning and employment status of persons with bipolar disorder. Psychiatric Services 55:54–58, 2004Google Scholar
16. Bauer MS, McBride L, Williford WO, et al: Collaborative care for bipolar disorder: part I: intervention and implementation in a randomized effectiveness trial. Psychiatric Services 57:927–936, 2006Google Scholar
17. Bauer MS, McBride L, Williford WO, et al: Collaborative care for bipolar disorder: part II: impact on clinical outcome, function, and costs. Psychiatric Services 57:937–945, 2006Google Scholar
18. Royall DR, Chiodo LK, Polk MJ: Correlates of disability among elderly retirees with "subclinical" cognitive impairment. Journals of Gerontology: Series A, Biological Sciences and Medical Sciences 55:M541–M546, 2000Google Scholar
19. Royall DR, Mahurin RK, Gray KF: Bedside assessment of executive cognitive impairment: the executive interview. Journal of the American Geriatrics Society 40:1221–1226, 1992Google Scholar
20. Royall DR, Mahurin RK, True JE, et al: Executive impairment among the functionally dependent: comparisons between schizophrenic and elderly subjects. American Journal of Psychiatry 150:1813–1819, 1993Google Scholar
21. Royall DR, Mahurin RK, Cornell J: Effect of depression on dementia presentation: qualitative assessment with the Qualitative Evaluation of Dementia (QED). Journal of Geriatric Psychiatry and Neurology 8:4–11, 1995Google Scholar
22. Royall DR, Cabello M, Polk MJ: Executive dyscontrol: an important factor affecting the level of care received by older retirees. Journal of the American Geriatrics Society 46:1519–1524, 1998Google Scholar
23. Bauer MS, McBride L, Shea N, et al: Screening for executive cognitive dysfunction in bipolar disorder. Biological Psychiatry 35:79A, 1994Google Scholar
24. Tohen M, Waternaux CM, Tsuang MT, et al: Four-year follow-up of twenty-four first-episode manic patients. Journal of Affective Disorders 19:79–86, 1990Google Scholar
25. Gold JM, Queern C, Iannone VN, et al: Repeatable battery for the assessment of neuropsychological status as a screening test in schizophrenia: I. sensitivity, reliability, and validity. American Journal of Psychiatry 156:1944–1950, 1999Google Scholar
26. Gold JM, Goldberg RW, McNary SW, et al: Cognitive correlates of job tenure among patients with severe mental illness. American Journal of Psychiatry 159:1395–1402, 2002Google Scholar
27. Levine J, Chengappa KN, Brar JS, et al: Illness characteristics and their association with prescription patterns for bipolar I disorder. Bipolar Disorders 3:41–49, 2001Google Scholar
28. Coryell W, Keller M, Endicott J, et al: Bipolar II illness: course and outcome over a five-year period. Psychological Medicine 19:129–141, 1989Google Scholar
29. Keller MB, Lavori PW, Coryell W, et al: Bipolar I: a five-year prospective follow-up. Journal of Nervous and Mental Disease 181:238–245, 1993Google Scholar
30. Goldberg JF, Harrow M, Grossman LS: Course and outcome in bipolar affective disorder: a longitudinal follow-up study. American Journal of Psychiatry 152:379–384, 1995Google Scholar
31. Goldberg JF, Harrow M, Grossman LS: Recurrent affective syndromes in bipolar and unipolar mood disorders at follow-up. British Journal of Psychiatry 166:382–385, 1995Google Scholar
32. O'Connell RA, Mayo JA, Flatow L, et al: Outcome of bipolar disorder on long-term treatment with lithium. British Journal of Psychiatry 159:123–129, 1991Google Scholar
33. Carlson GA, Kotin J, Davenport YB, et al: Follow-up of 53 bipolar manic-depressive patients. British Journal of Psychiatry 124:134–139, 1974Google Scholar
34. Strakowski SM, Keck PE Jr, McElroy SL, et al: Twelve-month outcome after a first hospitalization for affective psychosis. Archives of General Psychiatry 55:49–55, 1998Google Scholar
35. Freedman MD, Culver CM, Ferrell RB: On the safety of long-term treatment of lithium. American Journal of Psychiatry 134:1123–1126, 1977Google Scholar
36. Savard RJ, Rey AC, Post RM: Halstead-Reitan Category Test in bipolar and unipolar affective disorders: relationship to age and phase of illness. Journal of Nervous and Mental Disease 168:297–304, 1980Google Scholar
37. Sapin LR, Berrettini WH, Nurnberger JI Jr, et al: Mediational factors underlying cognitive changes and laterality in affective illness. Biological Psychiatry 22:979–986, 1987Google Scholar
38. Bulbena A, Berrios GE: Cognitive function in the affective disorders: a prospective study. Psychopathology 26:6–12, 1993Google Scholar
39. Martinez-Aran A, Vieta E, Reinares M, et al: Cognitive function across manic or hypomanic, depressed, and euthymic states in bipolar disorder. American Journal of Psychiatry 161:262–270, 2004Google Scholar
40. Martinez-Aran A, Vieta E, Colom F, et al: Cognitive impairment in euthymic bipolar patients: implications for clinical and functional outcome. Bipolar Disorders 6:224–232, 2004Google Scholar
41. Van Gorp WG, Altshuler L, Theberge DC, et al: Declarative and procedural memory in bipolar disorder. Biological Psychiatry 46:525–531, 1999Google Scholar
42. Ferrier IN, Stanton BR, Kelly TP, et al: Neuropsychological function in euthymic patients with bipolar disorder. British Journal of Psychiatry 175:246–251, 1999Google Scholar
43. Krabbendam L, Honig A, Wiersma J, et al: Cognitive dysfunctions and white matter lesions in patients with bipolar disorder in remission. Acta Psychiatrica Scandinavica 101:274–280, 2000Google Scholar
44. Deckersbach T, McMurrich S, Ogutha J, et al: Characteristics of non-verbal memory impairment in bipolar disorder: the role of encoding strategies. Psychological Medicine 34:823–832, 2004Google Scholar
45. Kern RS, Green MF, Satz P: Neuropsychological predictors of skills training for chronic psychiatric patients. Psychiatry Research 43:223–230, 1992Google Scholar
46. Buchanan RW, Holstein C, Breier A: The comparative efficacy and long-term effect of clozapine treatment on neuropsychological test performance. Biological Psychiatry 36:717–725, 1994Google Scholar
47. Lysaker P, Bell M, Beam-Goulet J: Wisconsin Card Sorting Test and work performance in schizophrenia. Psychiatry Research 56:45–51, 1995Google Scholar
48. Zubieta JK, Huguelet P, O'Neil RL, et al: Cognitive function in euthymic bipolar I disorder. Psychiatry Research 102:9–20, 2001Google Scholar
49. Bauwens F, Tracy A, Pardoen D, et al: Social adjustment of remitted bipolar and unipolar out-patients: a comparison with age- and sex-matched controls. British Journal of Psychiatry 159:239–244, 1991Google Scholar
50. Altshuler LL: Bipolar disorder: are repeated episodes associated with neuroanatomic and cognitive changes? Biological Psychiatry 33:563–565, 1993Google Scholar
51. Bell MD, Bryson G: Work rehabilitation in schizophrenia: does cognitive impairment limit improvement? Schizophrenia Bulletin 27:269–279, 2001Google Scholar
52. Bryson G, Bell MD, Kaplan E, et al: The functional consequences of memory impairments on initial work performance in people with schizophrenia. Journal of Nervous and Mental Disease 186:610–615, 1998Google Scholar



