Datapoints: Use of Information Technology by Psychiatrists and Other Medical Providers
The landmark Institute of Medicine (IOM) report, Crossing the Quality Chasm ( 1 ), concluded that information technology (IT) "must play a central role in the design of health care systems if a substantial improvement in health care quality is to be achieved."
There are concerns that psychiatry may lag behind other medical fields in adopting IT ( 2 ). To further investigate this issue, I used data from the 2004–2005 Community Tracking Study (CTS) Physician Survey to compare adoption of IT, including some of the applications highlighted by the IOM report, by psychiatrists and other medical providers.
The 2004–2005 survey involved 6,628 nonfederal U.S. physicians, of which 3,291 primary care physicians, 1,674 other medical specialists, and 367 psychiatrists were included in these analyses. The frequency of use of the different IT applications was compared across these groups while adjusting for survey sampling weights. To minimize type I error resulting from multiple testing and clustering, a conservative significance level (p<.001) was used to judge statistical significance.
There was an overall tendency for psychiatrists to use fewer IT applications compared with other providers ( Figure 1 ). In bivariate logistic regression analyses, the differences between psychiatrists and primary care physicians were statistically significant for exchanging clinical data and images with hospitals and laboratories (odds ratio [OR]=.27), obtaining information about treatment alternatives or guidelines (OR=.54), and generating reminders about preventive services (OR=.40). In multivariate analyses adjusting for type of practice and years in practice, the difference in data and image exchange remained statistically significant.
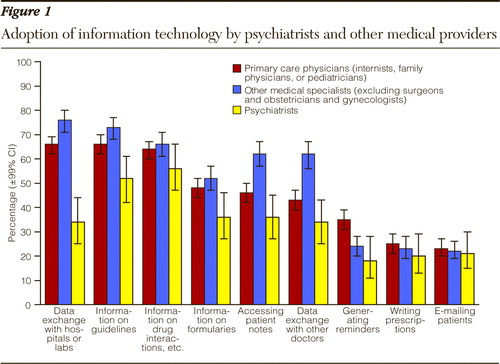
The differences between psychiatrists and other medical specialists reached significance for exchanging data and images with hospitals and laboratories (OR=.16); obtaining information about treatment alternatives or guidelines (OR=.40); obtaining information on formularies (OR=.53); accessing patient notes, medication or problem lists (OR=.34); and exchanging data and images with other physicians (OR=.31). In multivariate analyses, all the differences except for obtaining information on formularies remained statistically significant.
These data confirm concerns about psychiatrists lagging behind other medical providers in adopting IT ( 2 ). Although psychiatrists' lesser reliance on laboratory and imaging studies may explain differences in data exchange with hospitals and labs, concerns about patient privacy (for example, with regard to computerized patient notes) are shared among all medical providers. Adoption of national privacy standards may facilitate diffusion of IT in psychiatry as well as in other health care fields ( 1 ).
Acknowledgments and disclosures
Dr. Mojtabai has received consultant fees and research funding from Bristol-Myers Squibb.
1. Institute of Medicine: Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC, National Academies Press, 2001Google Scholar
2. Pincus HA, Page AE, Druss B, et al: Can psychiatry cross the quality chasm? Improving the quality of health care for mental and substance use conditions. American Journal of Psychiatry 164:712–719, 2007Google Scholar



