Criminal Records of Persons Served in the Public Mental Health System
When persons with mental illness have symptoms that are not well controlled or experience difficulties in functioning, their behavior can result in criminal justice involvement. In a survey of 260 persons with relatives who have mental illness, 52% reported that the relative had at least one arrest ( 1 ).
From studying persons involved in the criminal justice system, researchers have established that the prevalence of mental disorders is high among jail and prison inmates ( 2 , 3 , 4 , 5 ), and indeed, persons with mental illness are crowding jails and prisons. A 2005 survey by the Bureau of Justice Statistics ( 6 ) found that 24% of state prison inmates, 14% of federal inmates, and 21% of those in local jails reported having mental health treatment in the past 12 months. Furthermore, 49% of state prison inmates, 40% of federal inmates, and 60% of those in local jails reported symptoms of mental illness. The 2000 Census of State and Federal Adult Correctional Facilities ( 7 ) found that one of every eight state prisoners was receiving some mental health therapy or counseling and 10% were receiving psychotropic medications ( 7 ).
In several large-scale projects, researchers in the United States and overseas also have probed the sensitive question of whether mental illness is linked to violence. They have calculated the risk of violence among persons with serious mental illness by comparing birth cohorts of persons with and without a diagnosis of mental illness and by documenting the criminal justice involvement of patients receiving intensive levels of treatment, such as inpatient care ( 8 , 9 , 10 , 11 , 12 , 13 , 14 , 15 ). They have established that violence and mental disorder are indeed linked. In addition, the strength of this association appears to vary by diagnosis. Persons with schizophrenia appear to be at higher risk of violence than others ( 16 , 17 , 18 , 19 , 20 ), whereas persons with depressive disorders may or may not be at higher risk of violence, depending in part on whether they also abuse substances ( 14 , 21 , 22 ). Violence often is assessed by inspecting arrest records.
Few studies have examined the full spectrum of criminal involvement of persons with mental illness, with coverage of crimes of all types ( 23 ). This gap is particularly important given that most jail inmates are not charged with violent crimes. In addition, samples seldom are representative of persons receiving mental health treatment ( 23 ). Reviewing this literature in a 2005 publication, Theriot and Segal ( 23 ) noted that available studies are "older or offer little perspective on community mental health outpatients because of overly restrictive or inclusive samples." They examined criminal justice records of 673 clients seen at ten community mental health centers and 11 self-help agencies. They recorded complete criminal justice involvement from arrest records but restricted their sample to new clients. These were clients who had not been seen in the organization or type of organization where they were assessed, and they received treatment for at least six months. The researchers found that 45% of new clients had at least one criminal justice contact before coming to the agency. Also, among persons with any criminal justice contact, the average number of contacts was almost eight. Criminal justice encounters subsequent to entering treatment were not assessed.
Few studies have addressed whether timely provision of mental health treatment prevents criminal justice involvement. Policy makers have gravitated to this possibility, believing that inadequate treatment in the community fuels a cycle of crisis hospitalizations, homelessness, and arrest that overwhelms state and local correctional systems ( 24 , 25 ). In particular, with respect to "usual care"—treatment routinely provided in the mental health system—we lack even preliminary data. In research literature to date, data are lacking on whether persons with mental illness who were arrested had in fact been treated or, if treated, the specific sequences and intervals between treatment and arrest ( 26 ).
To better understand criminal justice involvement of treated persons with mental illness, researchers need access to comprehensive mental health treatment data and comprehensive criminal justice data ( 1 , 26 , 27 ). Having such data frees researchers from addressing only particular kinds of clients, diagnoses, or types of arrests, or only particular clinics or program types. Merging comprehensive mental health treatment and criminal justice data is rarely attempted, however, because technical challenges to matching records can be formidable and because confidentiality concerns can prevent mental health and criminal justice officials from making data available for research.
This exploratory, retrospective study used administrative data on treatment and criminal justice contact from a large, random sample of clients with disabilities who were receiving Medicaid-financed mental health treatment in Los Angeles County. We used these data to assess characteristics of individuals who were arrested and those who were not. Characteristics included mental illness diagnosis and average mental health service use; the number, seriousness, and disposition of arrests; associations between mental illness diagnosis and severity of arrest; and associations between arrest and treatment, specifically differences in patterns of care before and after arrest.
Methods
Data sources
We used administrative data from the California Medicaid claims and state arrest systems. First, we randomly drew 10,000 adults from Medicaid claims records of Los Angeles County mental health system providers. Because most previous research and policy discussions focus on this high-risk population, we were interested in adults with a mental illness that was serious enough to be disabling. We excluded individuals who were eligible for Medicaid for reasons other than disability and those who were not at least 18 years old as of July 1993. Following these criteria produced a sample of 6,624 adults with serious mental illness, which was used in the analysis.
The records for these individuals were matched against state criminal justice arrest records from July 1991 to 2001 on the basis of last name, gender, and date of birth. Separately, records also were matched on the basis of Social Security number. The Social Security number match yielded a slightly lower match rate. However, the results of the analysis were not substantially affected by the matching method used. The data sets were linked by the state department of justice. The analysis file used here contained encrypted, individual-level identifiers. The study received approval from the institutional review board at the University of California, Berkeley. The criminal justice file includes all events requiring fingerprints, including arrests and noncriminal events, such as certain employment applications. We excluded any records for noncriminal events for this analysis. The criminal justice data included the event date, the offense or offenses for which the individual was charged at the time of arrest, the type of disposition (such as dismissal, conviction, jail, probation, or diversion), and the disposition date.
An arrest could be associated with more than one type of offense. To arrive at a single offense for purposes of analysis, we assigned the most severe offense to each arrest on the basis of a hierarchy of crime types derived from categories established by the Federal Bureau of Investigation ( 28 ). The highest-ranking offense for a given arrest was then assigned to one of the following mutually exclusive groups: violent crime (such as murder or assault), other crime against a person (such as contributing to the delinquency or corruption of a minor, verbal assault, weapons possession, and reckless endangerment), drug crime, property crime (such as theft, burglary, unlawful entry, and larceny), minor and other crimes (primarily disorderly conduct but also public lewdness, traffic infractions, driving while intoxicated, public intoxication, and similar offenses).
For the full sample of 6,624 individuals, the state Department of Mental Health also provided information on all Medicaid claims for mental health treatment for eight years from July 1, 1993, to June 30, 2001. The Medicaid treatment files capture a range of covered services, including inpatient, emergency, day treatment, crisis management, case management, medication management, and physician visits. Following the Department of Mental Health, we defined inpatient services as the number of days in an acute or a psychiatric hospital for a mental health diagnosis. Crisis services were defined as the number of days on which an individual received one or more emergency or crisis case management services. Outpatient services were defined as the number of days on which an individual received a noncrisis outpatient service, including physician, clinic, case management, and medication visits. Amounts of services were calculated as the number of days on which a particular service was received. For example, an individual receiving two physician visits on one day was counted as having one outpatient service day. The claims data also include date of birth, gender, and race. In the following analyses age was defined as the individual's age as of July 1, 1993.
For the purposes of statistical comparison, individuals were separated into diagnostic categories based on the ICD-9 diagnosis reported in the claims. The claims data did not include secondary diagnoses. However, some patients were reported as having multiple diagnoses over time. Individuals were assigned to a diagnostic group on the basis of a hierarchy of diagnoses from highest to lowest: schizophrenia or schizoaffective disorder, psychotic disorder not otherwise specified or delusional disorder, bipolar disorder, depressive disorder (major depression and depressive illness), and other disorders. The state of California has separate delivery systems for substance abuse and mental health services, and therefore only a relatively small proportion of patients treated in the mental health system could have a primary diagnosis of a substance use disorder. We created a separate indicator for the presence of a substance abuse claim.
Statistical procedures
Descriptive analyses were performed to compare characteristics of clients who were arrested and clients who were not arrested. All analyses were performed with Stata statistical software, version 8. We performed chi square tests to investigate differences in race and ethnicity, age, gender, and diagnosis. To test differences in the number of mental health services received per person, using continuous measures of inpatient days, crisis days, outpatient days, and any service days, we performed t tests. We developed logistic regression models to ascertain whether arrest varied by diagnosis, controlling for patient characteristics, specifically age, gender, and ethnicity. We present odds ratios (ORs) and 95% confidence intervals (CIs) for the multivariate regression results.
To examine whether clients received services before or after being arrested, we focused on data for only the clients who were arrested after July 1, 1994. To cover the possibility that clients received community treatment after arrest, we limited our analysis to those who received a community disposition for their offense (for example, dismissal or probation), not a jail or prison sentence. This gave us a sample of 481 clients. For clients with multiple arrests, we examined only the first arrest. For these 481 clients we calculated the proportion who received services before and after arrest (within 30 days and 180 days, respectively) and conducted McNemar chi square tests for statistical significance, which take into account the nonindependence of the observations. We assessed receipt of inpatient, crisis, and outpatient treatment separately.
Results
Individual and treatment characteristics of arrest
Over the ten-year period examined, nearly one-quarter of individuals in our sample were arrested. Among 6,624 individuals with serious mental illness, 1,563 (23.6%) had at least one arrest over the ten-year period. Consistent with crime trends in the general population ( 29 ), those who were arrested were significantly more likely to be male, younger, and African American than those who were not arrested ( Table 1 ). The multivariate logistic regression model, which controlled for age, gender, and race and ethnicity, also showed that those with arrest records differed in terms of mental health diagnosis. Compared with individuals with schizophrenia, those with bipolar disorder had higher odds of being arrested (OR=1.4, CI=1.1-1.7, p=.009), whereas those with depressive disorder had lower odds of being arrested (OR=.7, CI=.6-.8, p=.009).
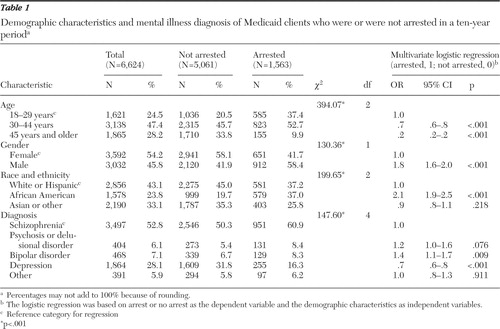 |
Individuals who were arrested at least once over the ten-year period received virtually the same number of mental health services on average as those who were not arrested over the time frame observed (data not shown). Arrested and nonarrested persons received 109.4 days of any service on average. Arrested persons received more outpatient services on average than persons without arrests, but the differences were not statistically significant at conventional levels. Individuals who were arrested had longer hospitalizations (4.1 days versus 1.8 days; t=10.53, df=6,622, p<.001) and more crisis services (2.7 visits versus 1.3 visits; t=9.61, df=6,622, p<.001) than persons who were not arrested.
Arrest and offense patterns
The 1,563 arrested individuals had an average of 3.3 arrests. Repeat contact was relatively common among those who were arrested. Among the arrested group, 895 (57.3%) were arrested more than once in the ten-year period examined (data not shown). However, the distribution of arrests was skewed, with 667 individuals (42.7%) arrested only once, 620 (39.7%) arrested two to five times, and 275 (17.6%) arrested more than five times over ten years.
Of the 5,132 observed arrests, 2,566 (50%) received dispositions that resulted in the case being dismissed, suspended, or similar, meaning there was no further action (data not shown). Forty-seven percent of the arrests led to conviction with a jail sentence, probation, fine, or restitution. Only 154 (3%) were diverted by the justice system to community services in lieu of further court processing.
We assessed the most serious offense over ten years for each person arrested ( Table 2 ) and found that 37.7% of individuals had as their most serious offense an arrest for a violent crime (murder or assault). For 22.8% the most serious offense was a drug offense, whereas for 18.5% a property offense (such as theft, burglary, unlawful entry, or larceny) was the most serious offense. Another 10.4% of the arrested sample had as their most serious offense nonviolent crimes against another person (such as contributing to the delinquency or corruption of a minor, verbal assault, weapons possession, reckless endangerment, and similar offenses), and 10.6% had as their most serious offense a minor or other crime (primarily disorderly conduct but also public lewdness, traffic infractions, driving while intoxicated, public intoxication, and similar offenses). Our study also showed that the distribution of offense types differed by mental health diagnosis. We examined the most serious offense for each individual arrested and found significant differences in arrests across mental health disorders ( χ2 =47.8, df=16, p<.001).
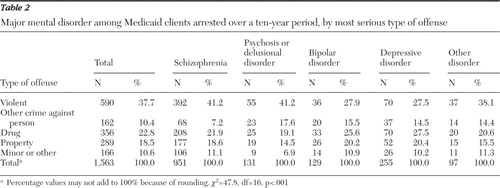 |
We then grouped individuals diagnosed with schizophrenia or psychosis or delusional disorders and compared them with persons with other disorders (data not shown). We tested whether the first group was more likely to have a violent crime as their most serious offense relative to any other offense type and found large and statistically significant differences across mental disorders (41.3% with schizophrenia or psychotic disorders compared with 29.7% for persons with other disorders had a violent offense; χ2 =19.0, df=1, p<.001). We then compared drug crimes with all other crimes and found that persons with schizophrenia, psychosis, or delusional disorders were somewhat less likely than other individuals to have been arrested for a drug crime (21.5% versus 25.6%), although the results were not significant.
Treatment patterns before and after arrest
For the next analysis we examined service use before and after arrest for 481 arrested individuals. Table 3 shows that many were not receiving Medicaid-funded mental health treatment in the 180 days before being arrested. Forty-seven percent received at least one service within 180 days of arrest, 44.3% received an outpatient visit, 9.6% a crisis service, and 10.6% were hospitalized.
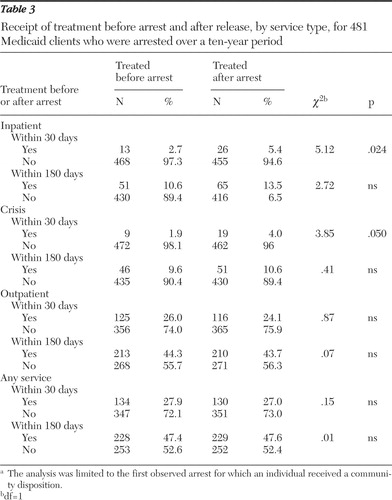 |
In the 30 days before arrest, slightly more than a quarter (27.9%) received any service, generally an outpatient visit (26.0%). Three percent had conditions severe enough to be hospitalized for their mental illness in the 30 days before arrest, and 1.9% received crisis services.
To determine whether arrest was associated with receiving subsequent services, we compared the proportion receiving services before arrest with the proportion receiving services after arrest ( Table 3 ). The difference in the likelihood of receiving any service before or after arrest was very small and not statistically significant. However, arrested individuals were more likely to receive inpatient services in the 30 days after arrest than before (5% versus 3%, χ2 =5.12, df=1, p=.024) and more likely to receive crisis services (4% versus 2%, χ2 =3.85, df=1, p=.050), indicating a possible flare-up of symptoms for some. Arrested individuals were not significantly more likely to receive outpatient services after arrest than before, regardless of the period assessed (30 or 180 days).
Discussion
Our study of 6,624 individuals with serious mental illness found a relatively high arrest rate (23.6%), with relatively frequent repeat arrest (57.3%) over a ten-year period in a community-based sample of persons with disabilities who received treatment in the public mental health system. Half of the arrests resulted in the case's being dismissed, suspended, or otherwise disposed of without further action. Overall, 8.9% of the sample were arrested for a violent crime. Most arrests were for nonviolent crimes, in sharp contrast to public perceptions that persons with severe mental illness are violent or dangerous.
Among the 6,624 clients, there were 5,132 total arrests over the ten-year period. This translates to 775 arrests per 1,000 in the population over ten years. By comparison, the annual arrest rate in Los Angeles was 34.1 per 1,000 in the population in 2002 ( 30 ). Over a ten-year period, assuming constant arrest and population growth in the community, the community arrest rate would be less than half the arrest rate observed in our sample (341 compared with 775). This comparison is only approximate; it does not adjust for possible differences in key demographic factors.
The arrest rate in our study was lower than that of some other studies of persons with mental illness. Theriot and Segal ( 23 ) studied 673 new entrants to self-help agencies and community mental health centers and reported a considerably higher proportion of prior arrests (45% compared with less than 24% in our study) and convictions (79% of those arrested compared with 47%). Half of their sample was arrested for a violent offense compared with 38% in our sample. Contributing to criminal justice involvement, many in their study were homeless and abused substances. Conceivably, the criminal justice involvement of the consumers for Theriot and Segal's study might be greater than we observed because individuals in our sample were at least periodic users of mental health services. It is also possible that the difference reflects different local policing and crime enforcement policies.
Our study found that individuals diagnosed as having schizophrenia or psychosis were disproportionately arrested for violent crimes, whereas persons with other disorders were disproportionately arrested for drug crimes. Drug crimes likely reflect comorbid substance use disorders, which are relatively common among persons with serious mental illness. Persons with schizophrenia also may abuse illicit substances, but they may behave aggressively more than persons with depression. Arresting persons with schizophrenia for aggressive behavior may take precedence over arresting them for violating drug laws.
The study also found a high rate of arrest among African Americans. This result is consistent with community studies showing African Americans' higher rates of diagnosed schizophrenia, lower likelihood of receiving the latest psychiatric medications, and greater difficulty in achieving successful community integration ( 31 , 32 , 33 ). It is possible that their difficulties in accessing care lead to more severe symptoms, greater criminal involvement, and more frequent arrest.
Although jail environments may promote decompensation ( 34 ), we did not find that arrested individuals were more likely to receive treatment services after arrest than before. Arrest may be an indicator that symptoms of mental illness have flared up. Despite arrest and a diagnosis of mental illness associated with disability and a requirement of long-term treatment, however, only 27% of the sample received mental health treatment of any kind within 30 days from the date of arrest. Equally revealing, those who were treated were more likely to receive inpatient and crisis care after their arrest than before, and they were no more likely to receive outpatient care. The lack of change in outpatient service use after arrest points to potential missed opportunities to reconnect to treatment individuals whose arrest was indicative of increased symptoms or for whom arrest may have promoted decompensation.
The data point to a potentially large and important role that the criminal justice system could play in reconnecting individuals to services. Better communication between the mental health and criminal justice systems could reduce the time between release from jail and subsequent initiation of treatment. One response to high rates of arrest and incarceration of persons with mental illness has been to examine carefully the role played by the police, who are key gatekeepers who often must decide whether disruptive behavior should be treated as psychiatric or criminal ( 35 ). Mobile crisis intervention programs, where mental health expertise informs policing efforts, have been developed and deployed, and some have shown promising results ( 36 ).
When considering our findings, several limitations should be kept in mind. We were limited to a single site, which raises questions of geographic generalizability. However, our research site, Los Angles County, provides an important venue to study mental illness and criminal justice involvement. In fiscal year 2000 approximately 55,000 individuals received outpatient mental health services in jail in Los Angeles County ( 37 ). Because we observed only Medicaid-funded services, members of our sample may have lacked care because they did not seek or were not referred for services or because they lost Medicaid eligibility ( 38 ). Thus our results are indicative of problems in either access to services or in Medicaid enrollment. We cannot distinguish between these equally problematic alternatives, nor did we observe non-Medicaid-financed services, including more informal treatment or treatment provided in sectors other than Medicaid-funded specialty mental health services. Another limitation is that we had limited ability to measure co-occurring substance abuse or dependence and could not measure homelessness. Our ten-year window falls short, for many people, of encompassing complete treatment and arrest careers. Finally, our research design was correlational, not experimental, and we could not draw conclusions about cause and effect.
Conclusions
Our study shows that almost a quarter of persons with serious mental illness were arrested in a ten-year period. Many of these individuals were arrested for violent crimes, with drug crimes the second most common category of crime. However, half of the arrests did not lead to conviction. Furthermore, the seriousness of the offense varied with the person's diagnosis. We also found that arrest was not associated with meaningful increases in service use, pointing to potential missed opportunities to reconnect those individuals to treatment. Future research should address whether receipt of community-based mental health care causally reduces the probability of arrest, and if so, what intensity of community-based care has the largest effect on arrest, and whether these relationships vary by type of crime or diagnosis.
Acknowledgments and disclosures
This research was supported by a grant to Dr. Snowden from the California Program for Access to Care and by grant K01-MH-067086 to Dr. Cuellar from the National Institute of Mental Health.
The authors report no competing interests.
1. McFarland BH, Faulkner L, Bloom JD, et al: Chronic mental illness and the criminal justice system. Hospital and Community Psychiatry 40:718-723, 1989Google Scholar
2. Teplin LA: The prevalence of severe mental disorder among male urban jail detainees: comparison with the Epidemiologic Catchment Area program. American Journal of Public Health 80:663-669, 1990Google Scholar
3. Steadman HJ, Fabisiak S, Dvoskin J, et al: A survey of mental disability among state prison inmates. Hospital and Community Psychiatry 38:1086-1090, 1989Google Scholar
4. Powell TA, Holt JC, Fondacaro KM: The prevalence of mental illness among inmates in a rural state. Law and Human Behavior 21:427-438, 1997Google Scholar
5. Guy E, Platt E, Zwerling I, et al: Mental health status of prisoners in an urban jail. Criminal Justice and Behavior 12:29-53, 1985Google Scholar
6. James DJ, Glaze LE: Mental Health Problems of Prison and Jail Inmates. Washington, DC, US Department of Justice, Office of Justice Programs, September 2006Google Scholar
7. Beck AJ, Maruschak LM: Mental Health Treatment in State Prisons, 2000. Washington, DC, US Department of Justice, Office of Justice Programs, July 2001Google Scholar
8. Brennan PA, Mednick SA, Hodgins S: Major mental disorders and criminal violence in a Danish birth cohort. Archives of General Psychiatry 57:494-500, 2000Google Scholar
9. Link B, Andrews H, Cullen F: The violent and illegal behavior of mental patients reconsidered. American Sociological Review 57:275-292, 1992Google Scholar
10. Steadman HJ, Mulvey EP, Monahan J, et al: Violence by people discharged from acute psychiatric inpatient facilities and by others in the same neighborhoods. Archives of General Psychiatry 55:393-401, 1998Google Scholar
11. Swanson JW, Holzer CE, Ganju VK, et al: Violence and psychiatric disorder in the community: evidence from the Epidemiologic Catchment Area surveys. Hospital and Community Psychiatry 41:761-770, 1990Google Scholar
12. Tilhonen J, Isohanni M, Rasanen P, et al: Specific major mental disorders and criminality: a 26-year prospective study of the 196 northern Finland birth cohort. American Journal of Psychiatry 154:840-845, 1997Google Scholar
13. Karson C, Bigelow LB: Violent behavior in schizophrenic inpatients. Journal of Nervous and Mental Disease 175:178-188, 1987Google Scholar
14. Pearson M, Wilmont E, Padi M: A study of violent behavior among in-patients in a psychiatric hospital. British Journal of Psychiatry 149:232-235, 1986Google Scholar
15. Shader RI, Jackson AH, Harmatz JS: Patterns of violent behavior among schizophrenic inpatients. Diseases of the Nervous System 38:13-16, 1977Google Scholar
16. Lindqvist P, Allebeck P: Schizophrenia and crime: a longitudinal follow-up of 644 schizophrenics in Stockholm. British Journal of Psychiatry 157:345-350, 1990Google Scholar
17. Modestin J, Ammann R: Mental disorder and criminality: male schizophrenia. Schizophrenia Bulletin 22:69-82, 1996Google Scholar
18. Wessely S: The epidemiology of crime, violence, and schizophrenia. British Journal of Psychiatry 170:8-11, 1997Google Scholar
19. Tardiff K, Marzuk PM, Leon AC, et al: Violence by patients admitted to a private psychiatric hospital. American Journal of Psychiatry 154:88-93, 1997Google Scholar
20. Quinsey VL, Harris GT, Rice ME, et al: Violent Offenders: Appraising and Managing Risk. Washington, DC, American Psychological Association, 1998Google Scholar
21. Myers KM, Dunner DL: Self and other directed violence on a closed acute-care ward. Psychiatry Quarterly 54:178-188, 1984Google Scholar
22. Rossi AM, Jacobs M, Monteleone M, et al: Characteristics of psychiatric patients who engage in assaultive or other fear-inducing behavior. Journal of Nervous and Mental Disease 174:154-160, 1986Google Scholar
23. Theriot MT, Segal SP: Involvement with the criminal justice system among new clients at outpatient mental health agencies. Psychiatric Services 56:179-185, 2005Google Scholar
24. Achieving the Promise: Transforming Mental Health Care in America. Pub no SMA-03-3832. Rockville, Md, Department of Health and Human Services, President's New Freedom Commission on Mental Health, 2003Google Scholar
25. The Criminal Justice/Mental Health Consensus Project. New York, Council of State Governments, June 2002Google Scholar
26. Veysey BM, Steadman HJ, Morrissey JP, et al: In search of missing linkages: continuity of care in U.S. jails. Behavioral Health Sciences and the Law 15:383-397, 1997Google Scholar
27. Teplin LA: Criminalizing mental disorder: the comparative arrest rate of the mentally ill. American Psychologist 39:794-803, 1984Google Scholar
28. Federal Bureau of Investigation: Crime in the United States, 2000, Uniform Crime Reports. Washington, DC, US Department of Justice, 2000Google Scholar
29. California Department of Justice: Crime and Delinquency in California. Sacramento, Calif, Criminal Justice Statistics Center, 2003Google Scholar
30. Statistical Digest. Los Angeles, Los Angeles Police Department, Information Technology Division, 2003Google Scholar
31. Skaer TL, Sclar DA, Robison LM, et al: Trends in rate of depressive illness and use of antidepressant pharmacotherapy by ethnicity/race: an assessment of office-based visits in the United States, 1992-1997. Clinical Therapeutics 22:1575-1589, 2000Google Scholar
32. Young AS, Klap R, Sherbourne CD, et al: The quality of care for depressive and anxiety disorders in the United States. Archives of General Psychiatry 58:55-61, 2001Google Scholar
33. Blazer DG, Hubels CF, Simonsick EM, et al: Marked differences in antidepressant use by race in an elderly community sample: 1986-1996. American Journal of Psychiatry 157:1089-1094, 2000Google Scholar
34. Lamb HR, Grant RW: The mentally ill in an urban county jail. Archives of General Psychiatry 39:17-22, 1982Google Scholar
35. Lamb HR, Weinberger LE, DeCuir WJ Jr: The police and mental health. Psychiatric Services 53:1266-1271, 2002Google Scholar
36. Lamb HR, Shaner R, Elliott DM, et al: Outcome for psychiatric emergency patients seen by an outreach police-mental health team. Psychiatric Services 46:1267-1271, 1995Google Scholar
37. California Department of Mental Health: Involuntary Detentions in California: Fiscal Years 1990-1991 Through 1999-2000. Sacramento, Calif, Department of Mental Health, State of California Health and Human Services Agency, 2002Google Scholar
38. Morrissey JP, Steadman HJ, Dalton K, et al: Assessing gaps between policy and practice in Medicaid enrollment of jail detainees with severe mental illness. Psychiatric Services 57:803-808, 2006Google Scholar



