Racial and Ethnic Differences in the Relationship Between Depression Severity and Functional Status
Major depression, one of the most common psychiatric disorders, is associated with significant morbidity. It is known to have a negative impact on an individual's perceived well-being and health-related functioning ( 1 , 2 ). The poor functioning linked with depressive disorders is of particular interest because of the social costs associated with loss of productivity and use of health services. It has been estimated that about 62 percent of the $83 billion annual cost of depression in the United States is due to missed work or lowered productivity ( 3 ).
Several studies have examined the association between depressive disorders and multiple dimensions of functional impairment in the general population and among patients in multispecialty group practices ( 1 , 2 , 4 ). Wells and colleagues ( 4 ) used the Medical Outcomes Study 36-item Short Form Health Survey (SF-36)—a measure that has since been used extensively to evaluate health-related functional status in a variety of populations—to show poor physical, psychosocial, and role functioning among persons with depression. To measure functional impairment among individuals with depression in the community, Broadhead and colleagues ( 2 ) used the number of days within the past three months that an individual had missed work.
Two recent large studies—the Patient Health Questionnaire (PHQ) Primary Care Study and PHQ Obstetrics-Gynecology Study ( 5 , 6 )—have used similar measures of function and disability (the SF-20, disability days, and health care use) to assess functional impairment among primary care patients with varying levels of depression severity. To measure depression severity, these studies used the PHQ-9, the validated depression module of the self-administered version of the PRIME-MD diagnostic instrument ( 7 ). Analysis of the PHQ studies showed that increasing levels of depression, as measured by the PHQ-9, were associated with a substantial decrease in functional status ( 7 ).
However, none of these prior reports have explored the association between depression and functional disability among different racial or ethnic groups. A few smaller studies have compared depression and functional impairment among elderly persons and showed that compared with whites, African Americans had higher levels of functional disability at the same levels of depression ( 8 , 9 ). These studies have been conducted only among elderly populations, and none have included Latinos.
Assessing the relationship between depression and functional impairment in different racial or ethnic groups is a growing priority for the health care system. The U.S. Department of Health and Human Services ( 10 ) and the Institute of Medicine ( 11 ) have both issued reports that list the elimination of racial and ethnic disparities in health care as their main goals, and depression is one of the leading health indicators that the U.S. Department of Health and Human Services monitors. These efforts to eliminate health disparities and the growing diversity in the United States gives urgency to the need to understand the impact that depression has in different populations. Differential levels of functional impairment at similar depressive levels may indicate a need to adjust depression measurement instruments in different populations ( 12 ). More fundamentally, different levels of functional impairment may suggest that depression has a different social and economic cost in different racial or ethnic populations ( 13 ).
In this study, data from the PHQ Primary Care and Obstetrics-Gynecology Studies were analyzed to compare functional impairment at different levels of depression severity among non-Hispanic whites, African Americans, and Latinos. The association between depression severity and functional status in the three different racial or ethnic groups was assessed by examining the relationship between PHQ-9 depression scores and SF-20 functional status scores, disability days, health care use, and symptom-related difficulty ( 7 ).
Methods
Study design
With institutional review board approval from Rutgers University, data from the PHQ Primary Care and Obstetrics-Gynecology Studies were combined and analyzed. The process of participant selection, administration of instruments, and data collection of the PHQ Primary Care and Obstetrics-Gynecology Studies is described in detail elsewhere ( 5 , 6 ). Briefly, from May 1997 to November 1998, a total of 3,000 primary care patients (1,422 from five general internal medicine clinics and 1,578 from three family practice clinics) participated in the PHQ Primary Care Study. From May 1997 to March 1999, 3,000 patients from seven obstetrics-gynecology outpatient sites participated in the PHQ Obstetrics-Gynecology Study. Participants in both studies, all of whom were aged 18 or older, were selected by one of two methods to minimize sampling bias: consecutive patients for a given clinic session or every nth patient until the intended quota for that session was achieved. Study participants in both studies completed the PHQ-9 and functional status measures before seeing their physician. A total of 5,427 study participants were included in our analysis; 3,366 were non-Hispanic white, 808 were African American, and 1,253 were Latino.
Depression measure
The PHQ-9 is the depression module of the full PHQ and includes the nine DSM-IV criteria that are used to diagnose major depressive disorder. The reliability and validity of the PHQ-9 has been established in general primary care populations ( 7 ). The PHQ-9 score can range from 0 to 27, because each of the nine items can be scored from 0, not at all, to 3, nearly every day. An additional question asks patients who endorsed one or more PHQ-9 symptoms, "How difficult have these problems made it for you to do your work, take care of things at home, or get along with other people?" This question is scored from 0, not difficult at all, to 3, extremely difficult.
At all sites, the PHQ-9 was administered before visits with the physician. Additionally, study participants completed the Medical Outcomes Study 20-item Short Form Health Survey (SF-20) ( 14 ). The SF-20 measures functional status in six domains; possible scores range from 0 to 100, with 100 representing best health. The three domains of the SF-20—mental health, social functioning, and general health perceptions—have been shown in a prior study in general populations to be highly correlated with PHQ-9 scores ( 7 ). Also, patients estimated the number of physician visits and disability days (defined as days of no activity) during the past three months. In most cases, the PHQ-9 and SF-20 were completed by the patient in written form. If assistance was required, the questionnaires were read to the patient by a medical assistant. Patients who spoke only Spanish were administered Spanish versions of the questionnaires. Consistent with the process for translation of survey instruments outlined previously ( 15 ), translation and back translation of the Spanish language version of the PHQ-9 and other questionnaires was repeated until the translators felt that the Spanish version corresponded closely with the English version.
Statistical analysis
To test for potential sociodemographic differences, we compared gender, age, marital status, highest education level attained, and language ability between the different racial or ethnic groups. The chi square test was used for comparisons of categorical data, and analysis of variance was used for continuous data. Previous validation of the PHQ-9 has established five categories of increasing depression severity: scores of 0 to 4, 5 to 9, 10 to 14, 15 to 19, and 20 or more ( 7 ). Scores of 10 to 14 represent a moderate level of depression; 15 to 19, moderately severe depression; and 20 or more, severe depression. Mean PHQ-9 scores and the proportion of patients at each level of depression severity were compared between the three racial or ethnic groups.
The relationship between depression severity and functional status was measured by examining mean scores on the three SF-20 scales (mental health, social functioning, and general health perceptions) as well as self-reported disability days, clinic visits, and symptom-related difficulty over the five intervals of PHQ-9 scores. The Pearson correlation coefficients between these different measures of functional status and the total PHQ-9 score were calculated for each racial or ethnic group. These correlation coefficients were transformed to Z scores and compared for statistically significant differences by using Fisher's Z test ( 16 ).
To adjust for sociodemographic differences between groups, linear regression models were specified by using the PHQ-9 as the dependent variable. The independent variables for each model included an interaction term between race or ethnicity and functional score. The interactive terms in the linear regression for the score on the SF-20 mental health scale, for example, is the multiplication of a dummy variable for Latino ethnicity and the score on the SF-20 mental health scale. The multiplication of the dummy variable for African-American race and the score on the SF-20 mental health scale is the other interactive term. Age, gender, marital status, highest education level attained, and language ability were then added to the models to determine whether these sociodemographic factors had a significant effect on the relationship between dependent and independent variables.
All statistical analyses were done by using SPSS for Windows 9.0.
Results
Patient characteristics
Table 1 highlights differences in sociodemographic characteristics found between the three different racial or ethnic groups. The non-Hispanic white group was the oldest (41.0 years) and had the highest level of educational achievement (88.0 percent had at least a high school education). The Latino patients included in this analysis were the youngest group (29.6 years) and the most likely to be female (97.9 percent) and to be married (59.9 percent). Almost half the Latino group had less than a high school education (47.5 percent), and a majority of the Latino group spoke only Spanish (74.5 percent).
 |
Mean PHQ-9 scores and rates of depression severity
Table 2 compares mean PHQ-9 scores and levels of depression severity between the three racial or ethnic groups. Groups were similar in mean PHQ-9 scores, ranging from 4.4 among African Americans to 4.8 among non-Hispanic whites. Likewise, groups were similar in the proportion of individuals with a PHQ-9 score of 10 or greater, a threshold indicative of clinically important depression ( 7 ). Approximately one-third of the study participants in each racial or ethnic group exceeded this PHQ-9 threshold. Finally, groups did not differ in the distribution of study participants among the different levels of depression severity.
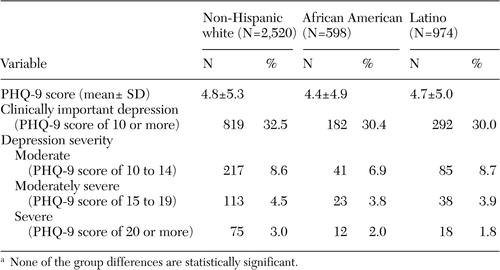 |
a None of the group differences are statistically significant.
Functional impairment
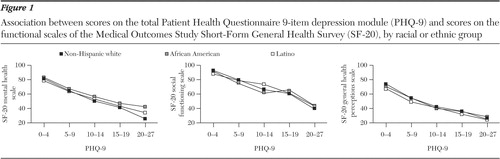
As shown in Figure 1 , for all three racial or ethnic groups there was a very similar association between increasing PHQ-9 depression severity scores and worsening function on the three SF-20 scales. Pearson correlation coefficients for scores on the SF-20 mental health scale and PHQ-9 scores among non-Hispanic whites, African Americans, and Latinos were -.74, -.64, and -.60, respectively; for the scores on the SF-20 social functioning scale and the PHQ-9 scores, -.51, -.42, and -.30, respectively; and for scores on the SF-20 general health perceptions scale and PHQ-9 scores, -.56, -.47, and -.47, respectively. Statistically significant differences (p<.01) between the non-Hispanic white group and Latino group were seen in all three sets of correlations. No other group differences were seen except in the correlations between scores on the SF-20 mental health scale and PHQ-9 scores between non-Hispanic whites and African Americans (p<.001).
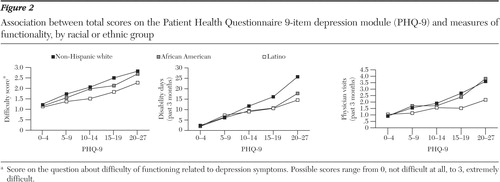
In Figure 2 , for all three racial or ethnic groups increasing depression severity was associated to a lesser degree with worsening function on the other measures of functional disability. Again, compared with the other two groups, the Latino group displayed consistently lower levels of functional difficulty at any given level of PHQ-9 depression severity. Pearson correlation coefficients for disability days and PHQ-9 scores among non-Hispanic whites, African Americans, and Latinos were .38, .32, and .27, respectively; for the number of physician visits and PHQ-9 scores, .24, .24, and .10, respectively; and for the question on the difficulty of functioning caused by the depression symptoms and PHQ-9 scores, .58, .55, and .46, respectively. Statistically significant differences (p<.001) between the non-Hispanic white group and the Latino group was seen in all three sets of correlations. There were no other group differences.
Results of sequential linear regressions showed no significant effect of age, gender, marital status, educational level, or the ability to speak English on the association of race or ethnicity and functional measure to PHQ-9 score. Also, an analysis of the Latino group who spoke only Spanish showed no difference with the English-speaking Latino group in the relationship between depression and function.
Discussion
To our knowledge, this is the first large analysis comparing the effect of depression on functional status across different racial or ethnic groups. We found a positive association between depression severity and functional impairment among non-Hispanic whites, African Americans, and Latinos. This association of depression and lower functional status was comparable between the three racial or ethnic groups across multiple measures of functionality, although the correlation coefficients were less robust for African-American and Latino study participants. Latinos, in particular, reported significantly less functional impairment compared with non-Hispanic whites at equivalent levels of depression severity. Although this finding was statistically significant in every measure of function, it should be noted that there was only a small absolute difference (on average 5 points) in scores on all three SF-20 scales between the Latino and non-Hispanic white groups at each level of depressive severity.
The lower correlation between functional impairment and depression severity among Latinos compared with non-Hispanic whites has several potential explanations. First of all, Latinos may express higher levels of depressive symptoms at similar levels of function, which would be consistent with prior research showing a higher expression of depressive symptoms in certain Latino populations ( 17 , 18 ).
Another possible explanation is that the Latinos in this study may not have allowed depressive symptoms to affect their work or social functioning as much as other individuals. This explanation is supported by the fact that the Latino group had mean depression severity scores similar to those of the other two groups and answered the question on the difficulty of functioning caused by the depression symptoms (How difficult have these problems made it for you to do your work, take care of things at home, or get along with other people?) with lower scores at every level of depressive severity. A prior study of depression among Latinos also found that they were less likely to say that they cannot work, regardless of their level of depression ( 19 ). The same pattern is seen with medical illnesses: Latinos with diabetes are less likely to claim work disability than individuals from other racial or ethnic groups ( 20 ).
Future studies can help clarify the reason for this difference between racial or ethnic groups in the relationship with depression severity and function. Investigator-rated depression measurement instruments can provide a more objective assessment of depression severity. Comparison of investigator-rated depression severity with self-assessed measures can also help ascertain whether certain study participants are more willing to admit to emotional distress than others. Investigator-rated assessments of function and surveys assessing individual changes in function—for example, "Have you been less productive at work than at baseline since becoming depressed?"—can also provide more impartial and specific information about how the depressive symptoms have affected function.
Our findings help explain, in part, the high levels of unmet need for mental health treatment among persons from racial or ethnic minority groups ( 21 ). In addition to the barriers to treatment that they encounter, patients from racial or ethnic minority groups, particularly Latinos, may be more stoic in the face of depressive symptoms and not seek treatment, just as they are less likely to take disability days or visit health care facilities. Clinicians who treat persons from racial or ethnic minority groups should be aware that they may not report as much functional disturbance as non-Hispanic whites with the same level of depressive symptoms. Screening for depressive disorders, as recommended by the U.S. Preventive Services Task Force, among Latinos and other racial or ethnic minority groups may be a critical step for reducing disparities in access to mental health treatment ( 22 ). It is also important to emphasize to patients the need for them to receive appropriate treatment for major depressive disorder.
Our study has several limitations. First, data on the place of birth and year of entry in the United States were not included in our analyses. Prior studies have shown that among Latinos the expression of depressive symptoms varies widely depending on an individual's country of origin and the length of time that he or she has lived in the United States ( 23 ). This information was not collected in the original PHQ studies and, therefore, could not be used in our analyses to assess whether these factors might account for some of the differences that we report. Future studies on this topic would benefit from inclusion of this information. Data about the socioeconomic status of study participants were also not collected. However, prior studies have established that education level can be used as a substitute measure for socioeconomic status ( 24 ).
A second limitation is that, although our study included three of the largest racial or ethnic groups in the United States, Asian Americans, Native Americans, and other important groups were not represented here. The relationship between depression and functional impairment in these other racial or ethnic groups is also important and should be of interest to clinicians, researchers, and health policy makers.
Conclusions
Our study indicates that functional impairment increases as depression symptoms worsen in a similar manner among non-Hispanic whites, African Americans, and Latinos. African Americans and Latinos report slightly lower functional impairment than non-Hispanic whites at comparable levels of depression severity, with Latinos having a significantly lower level of functional impairment compared with Non-Hispanic whites. Future studies that further explore the relationship of functional impairment and depression in different populations can help deepen our understanding of the effect of culture on the social effect of depression and develop strategies that can more proactively engage these groups for earlier intervention in depressive disorders.
Acknowledgments
The authors thank Scott Bilder, M.S., for statistical consultation. This study was supported by grants T32-MH-16242 (Dr. Huang) and P60-MD-000538 (Dr. Huang and Dr. Chung) from the National Institute of Mental Health.
1. Wells KB, Stewart A, Hays RD, et al: The functioning and well-being of depressed patients: results from the Medical Outcomes Study. JAMA 262:914-919, 1989Google Scholar
2. Broadhead WE, Blazer DG, George LK, et al: Depression, disability days, and days lost from work in a prospective epidemiologic survey. JAMA 264:2524-2528, 1990Google Scholar
3. Greenberg PE, Kessler RC, Birnbaum HG, et al: The economic burden of depression in the United States: how did it change between 1990 and 2000? Journal of Clinical Psychiatry 64:1465-1475, 2003Google Scholar
4. Wells KB, Burnam MA, Rogers W, et al: The course of depression in adult outpatients: results from the Medical Outcomes Study. Archives of General Psychiatry 49:788-794, 1992Google Scholar
5. Spitzer RL, Kroenke K, Williams JB: Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study: primary care evaluation of mental disorders: Patient Health Questionnaire. JAMA 282:1737-1744, 1999Google Scholar
6. Spitzer RL, Williams JB, Kroenke K, et al: Validity and utility of the PRIME-MD patient health questionnaire in assessment of 3,000 obstetric-gynecologic patients: the PRIME-MD Patient Health Questionnaire Obstetrics-Gynecology Study. American Journal of Obstetrics and Gynecology 183:759-769, 2000Google Scholar
7. Kroenke K, Spitzer RL, Williams JB: The PHQ-9: validity of a brief depression severity measure. Journal of General Internal Medicine 16:606-613, 2001Google Scholar
8. Cummings SM, Neff JA, Husaini BA: Functional impairment as a predictor of depressive symptomatology: the role of race, religiosity, and social support. Health and Social Work 28:23-32, 2003Google Scholar
9. Brown C, Schulberg HC, Sacco D, et al: Effectiveness of treatments for major depression in primary medical care practice: a post hoc analysis of outcomes for African American and white patients. Journal of Affective Disorders 53:185-192, 1999Google Scholar
10. Healthy People 2010: Understanding and Improving Health. Washington, DC, US Government Printing Office, Nov 2000Google Scholar
11. Institute of Medicine: Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC, National Academies Press, 2003Google Scholar
12. Dressler WM, Badger LW: Epidemiology of depressive symptoms in black communities: a comparative analysis. Journal of Nervous and Mental Disease 173:212-220, 1985Google Scholar
13. Kleinman A, Good B: Culture and depression: introduction to the problem, in Culture and Depression: Studies in Anthropology and Cross-Cultural Psychiatry of Affect and Disorder. Edited by Kleinman A, Good B. Berkeley, University of California Press, 1985Google Scholar
14. Stewart AL, Hays RD, Ware JE Jr: The MOS Short-Form General Health Survey: reliability and validity in a patient population. Medical Care 26:724-735, 1988Google Scholar
15. Shumaker SA, Berzon RA: The International Assessment of Health-Related Quality of Life: Theory, Translation, Measurement, and Analysis. Oxford, United Kingdom, Rapid Communications, 1995Google Scholar
16. Zar JH: Biostatistical Analysis, 4th ed. Upper Saddle River, NJ, Prentice-Hall, 1999Google Scholar
17. Aneshensel CS, Clark VA, Frerichs RR: Race, ethnicity, and depression: a confirmatory analysis. Journal of Personality and Social Psychology 44:385-398, 1983Google Scholar
18. Golding JM, Lipton RI: Depressed mood and major depressive disorder in two ethnic groups. Journal of Psychiatric Research 24:65-82, 1990Google Scholar
19. Azocar F, Arean P, Miranda J, et al: Differential item functioning in a Spanish translation of the Beck Depression Inventory. Journal of Clinical Psychology 57:355-365, 2001Google Scholar
20. Mayfield JA, Deb P, Whitecotton L: Work disability and diabetes. Diabetes Care 22:1105-1109, 1999Google Scholar
21. Wang PS, Lane M, Olfson M, et al: Twelve-month use of mental health services in the United States: results from the National Comorbidity Survey Replication. Archives of General Psychiatry 62:629-640, 2005Google Scholar
22. Pignone MP, Gaynes BN, Rushton JL, et al: Screening for depression in adults: a summary of the evidence for the US Preventive Services Task Force. Annals of Internal Medicine 136:765-776, 2002Google Scholar
23. Weinick RM, Jacobs EA, Stone LC, et al: Hispanic healthcare disparities: challenging the myth of a monolithic Hispanic population. Medical Care 42:313-320, 2004Google Scholar
24. Liberatos P, Link BG, Kelsey JL: The measurement of social class in epidemiology. Epidemiologic Reviews 10:87-121, 1988Google Scholar



