Innovations: Emergency Psychiatry: Relative Accuracy of Breath and Serum Alcohol Readings in the Psychiatric Emergency Service
Abstract
Management of changes in physiologic and mental status due to alcohol is a core skill utilized in the psychiatric emergency service. Blood alcohol concentrations are commonly approximated by measuring breath alcohol at triage. However, the blood-breath ratio is highly variable, and breath tests have produced lower readings than blood tests. The authors assessed the accuracy of breath alcohol readings at triage in a medical emergency department compared with subsequent serum alcohol levels taken in the psychiatric emergency service. The mean breath ethanol concentration was significantly lower than the mean corrected serum ethanol concentration (.15±.05 grams per 210 liters and .23±.05 grams per 100 milliliters, respectively). The relative accuracy of breath alcohol tests decreased with increasing serum alcohol. Although its low false-positive rate makes the breath test acceptable for legal purposes, the blood alcohol level is more appropriate for clinical use in emergency settings, because breath tests can underestimate the degree of toxicity.
Approximately 20 to 35 percent of people who consult health care providers abuse or are dependent on alcohol (1). Alcohol intoxication is associated with depression, irritability, and violence and is indicative of chronic substance abuse or other mental health concerns. Sudden cessation of habitual alcohol abuse may prompt a withdrawal syndrome characterized by autonomic hyperactivity, delirium, or seizures.
Management of changes in physiological and mental status due to alcohol is a core skill in the psychiatric emergency service. Blood alcohol concentrations are commonly approximated by measuring breath alcohol at triage. Breath assays assume an equilibrium state between the alcohol in the blood surrounding the lung and the gas in the alveoli. In the United States breath alcohol tests are calibrated with the amount of alcohol (in grams) in 210 liters in breath, presumed to be equal to the amount of alcohol in 100 milliliters of blood—a blood-breath (to alcohol) ratio of 2,100:1. In practice the blood-breath ratio is highly variable, with reported values ranging from 1,981:1 to 2,833:1 (2).
The time of measurement relative to the time of alcohol consumption is important in establishing an accurate ratio. A deprivation period of ten to 20 minutes is recommended to minimize the effects of alcohol in the mouth (3,4). In addition, blood levels tend to peak within 30 to 45 minutes of alcohol consumption (4). After alcohol reaches its peak level in the blood and the elimination process begins, the blood-breath ratio increases, and the ratio averages about 2,300:1 (5). Thus the blood-alcohol levels of patients who are post-peak would tend to be underestimated with the standard 2,100:1 conversion.
Several other factors can affect the blood-breath ratio. The last portion of a continuous expiration—the end-expiratory breath—should be analyzed, because alcohol concentration does not tend to plateau until two-thirds of the breath has been exhaled. Rebreathing air has been shown to decrease the blood-breath ratio (6). Temperature can also affect the blood-breath ratio (7).
The marketed breath alcohol tests vary in accuracy. In an electrochemical oxidation-fuel cell device, such as the Alco-Sensor III used for the study reported in this column, a fuel cell converts a fuel (ethanol) and an oxidant (oxygen) into a direct current that is measured to determine the level of ethanol present. These devices are relatively specific and do not respond to typical interfering substances (7).
The preferred method of blood alcohol testing is gas chromatography, although various methods exist. To prepare a sample for gas chromatography, the sample may be diluted with an aqueous solution of internal standard and injected into the chromatograph. Headspace vapor sampling—a variation on gas chromatography—involves diluting a specimen with an aqueous solution of internal standard, heating it, and then injecting a sample of the gas phase into the chromatograph. This method is highly sensitive, detecting alcohol levels as low as 10 milligrams per deciliter; however, the process is complicated and time-consuming (8). Advantageous in emergency situations, direct injection of a diluted sample eliminates the 15- to 30-minute equilibration period required for headspace analysis (9).
Another method of serum alcohol measurement involves enzymatic assay. Ethanol in the sample is converted to acetaldehyde by alcohol dehydrogenase in the presence of nicotinamide adenine dinucleotide, which in a reduced form can be measured spectrophotometrically. Although this method is relatively precise and accurate, it cannot be performed on whole blood, which is often required for legal purposes (8).
Emergency department research has indicated that breath alcohol levels derived from the Alco-Sensor III correlate strongly and significantly with blood alcohol concentrations; however, breath tests have produced lower readings than blood tests (10). Although current breath and blood alcohol assays appear to correlate relatively well in general, inaccurately low breath levels and individual variability may be clinically problematic.
The study reported here examined the accuracy of breath alcohol levels taken at triage in an emergency department compared with subsequent serum alcohol levels taken in the psychiatric emergency service. We hypothesized that there would be a strong overall correlation between breath and blood alcohol levels, but with significant individual variability.
Methods
This was a naturalistic study of the consistency of breath and blood measures of ethanol among intoxicated patients who presented to the emergency department of the University of Rochester Medical Center (URMC), where blood alcohol concentrations are commonly obtained for intoxicated patients who are transferred to the URMC psychiatric emergency service. A breath alcohol analysis is regularly completed at triage for patients who present with suspected intoxication. Depending on the level of intoxication and other clinical factors, the patient may be kept in the medical emergency department for observation and treatment. If the patient does not require medical intervention and the primary presenting problem is believed to be a psychiatric one, the patient may be immediately transferred to the psychiatric emergency service. A serum ethanol level is then routinely obtained for intoxicated patients who are transferred to the psychiatric emergency service.
To determine the consistency of breath and blood alcohol levels, we compared the readings of 65 intoxicated patients who presented to the URMC emergency department. These patients represented a convenience sample derived from the clinical population over the course of five months (July to November 2003). Breath alcohol analysis was performed for 61 of these patients, serum alcohol analysis for 59, and both breath and serum analysis for 55. The time of assessment for both measures was documented for 32 patients, who constituted the sample for whom data are reported here.
Equilibrating the measured blood ethanol concentration on the basis of time elapsed between the breath alcohol concentration at triage and the blood ethanol concentration taken in the psychiatric emergency service was required for meaningful comparison. We used a standard estimate of ethanol metabolism to approximate corrected serum alcohol—that is, what the blood ethanol concentration would have been at triage. Schuckit (1) reports that the average (70 kg) person can metabolize approximately one alcoholic drink per hour, effectively reducing serum ethanol by 15 to 20 milligrams per deciliter. We used the mean of these values—17.5 milligrams of alcohol per deciliter of blood per hour—for our corrected-concentration conversion. The equiv-alent value of .0175 g per 100 milliliter per hour was used in this analysis to correlate with reported serum ethanol in grams per 100 milliliters of blood, which is presumed to be equivalent to grams per 210 liters in breath, the units reported for breath ethanol measures.
Results
A substantial disparity was found in the time that elapsed between breath ethanol testing and serum ethanol measurement, with a range of .23 to 4.83 hours (mean±SD=1.28±1.02 hours). The degree of intoxication among participating patients who presented to the emergency department was also highly variable. The mean breath ethanol concentration measured at triage was .15±.05 grams per 210 liters in breath, with a range of .02 to .21. The mean corrected serum ethanol concentration was .23±.05 grams per 100 milliliters of blood, with individual values ranging from .06 to .32.
A two-tailed Pearson correlation coefficient was calculated for the relationship between breath and serum ethanol concentrations. A moderate positive correlation was found (r=.390, df=30, p<.03), indicating an overall consistent relationship between the variables. The lack of an especially strong correlation likely reflects the large discrepancies between breath and blood concentrations in certain cases.
A paired-samples t test was performed to determine whether the 2,100:1 blood-to-breath ratio produced an accurate estimation of blood ethanol. A significant difference between the means of blood and breath ethanol measurements was found (t=8.184, df=31, p<.001), indicating that average serum concentrations of ethanol were significantly higher than those indicated by breath ethanol.
With regard to individual variability, for 11 of 32 patients (34 percent) the corrected serum concentration varied by up to .05 from the measured breath ethanol level, and for 24 of 32 patients (75 percent) it varied by up to .10. Individual comparisons are shown in Figure 1.
For one patient, the breath ethanol concentration was actually higher than the serum concentration. Thus for eight of 32 patients (25 percent), corrected blood ethanol concentrations were more than .10 greater than those measured from breath. Serum ethanol was .23 higher in the most extreme case, indicating that in certain cases a patient's serum ethanol concentration may vary widely from a breath measurement.
The relative accuracy of breath alcohol tests decreased with increasing serum alcohol. When the corrected serum alcohol concentration was up to .20, breath and corrected serum ethanol means were not significantly different. Conversely, when corrected serum ethanol was greater than .20 grams per 100 milliliters, breath alcohol and corrected serum ethanol means were significantly different (t=8.199, df=25, p<.001).
Discussion and conclusions
Among 25 percent of the patients in this study, measured breath concentrations were at least .10 less than projected serum alcohol concentrations. Although there are several possible explanations for an aberrantly low breath ethanol value, the most likely one is that the patient did not provide an appropriate breath sample. It has been demonstrated that patient cooperation influences the strength of correlation between blood and breath alcohol concentrations (10).
Breath ethanol tests have the benefit of relatively simple application and are less invasive than blood ethanol tests. Furthermore, breath ethanol testing devices are generally portable and available for use in the field, giving them utility in law enforcement. Although a low false-positive rate makes the breath test acceptable for legal purposes, the blood alcohol level is more appropriate for clinical use in emergency settings, because breath tests can underestimate the level of toxicity. Clinical assessment of an appropriate time for patient assessment and disposition may be preferable to reliance on highly variable breath tests.
Dr. Currier and Mr. Walsh are affiliated with the department of psychiatry at the University of Rochester School of Medicine, 300 Crittenden Boulevard, Rochester, New York 14642 (e-mail, [email protected]). Dr. Currier is also with the department of emergency medicine at the school. Mr. Trenton is affiliated with the Nova Southeastern School of Medicine in Fort Lauderdale, Florida. Douglas H. Hughes, M.D., is editor of this column.
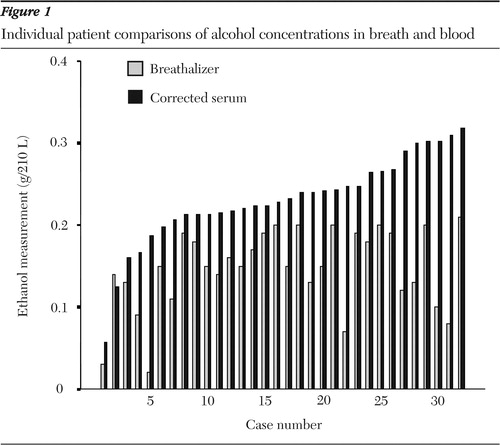
Figure 1. Individual patient comparisons of alcohol concentrations in breath and blood
1. Schuckit MA: Alcohol-related disorders, in Kaplan and Sadock's Comprehensive Textbook of Psychiatry. Edited by Sadock BJ, Sadock VA. Philadelphia, Lippincott Williams and Wilkins, 2000Google Scholar
2. Kwong TC: Toxicology, in Clinical Laboratory Medicine, 2nd ed. Edited by McClatchey KD. New York, Lippincott Williams and Wilkins, 2002Google Scholar
3. Trafford DJH, Makin HLJ: Breath-alcohol concentration may not always reflect the concentration of alcohol in blood. Journal of Analytical Toxicology 18:225–228,1994Crossref, Medline, Google Scholar
4. About Alcohol. St. Louis, Mo, Intoximeters, Inc. Available at www.intox.comGoogle Scholar
5. Moore R: Concerning breath alcohol measurements during absorption and elimination [letter]. Journal of Analytical Toxicology 15:346–347,1991Crossref, Medline, Google Scholar
6. Jones AW: Role of rebreathing in determination of the blood-breath ratio of expired ethanol. Journal of Applied Physiology 55:1237–1241,1983Crossref, Medline, Google Scholar
7. Dubowski KM: The Technology of Breath-Alcohol Analysis. Rockville, Md, US Department of Health and Human Services, 1991Google Scholar
8. Laposata M: Assessment of ethanol intake: current tests and new assays on the horizon. American Journal of Clinical Toxicology 112:443–450,1999Google Scholar
9. Hlastala MP: The alcohol breath test: a review. Journal of Applied Physiology 84:401–408,1998Crossref, Medline, Google Scholar
10. Gibb KA, Yee AS, Johnston CC, et al: Accuracy and usefulness of a breath alcohol analyzer. Annals of Emergency Medicine 13:516–520,1984Crossref, Medline, Google Scholar



