Suicidal Ideation and Pharmacotherapy Among STEP-BD Patients
Abstract
OBJECTIVE: Little is known about the effects of lithium on suicidal ideation or about the possible antisuicidal effects of divalproex, second-generation antipsychotics, or antidepressants among persons with bipolar disorder. METHODS: Using a cross-sectional design, the authors examined patterns of psychotropic drug use relative to suicidal ideation among 1,000 patients with bipolar disorder in the National Institute of Mental Health's Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD). RESULTS: The presence of suicidal ideation was similar between patients who were taking any lithium and those who were not (22.2 percent and 25.8 percent, respectively) and between those who were taking any divalproex and those who were not (20.3 percent and 21.5 percent). Suicidal ideation was significantly more prevalent among patients who were taking a second-generation antipsychotic than those who were not (26 percent and 17 percent) and those who were taking an antidepressant and those who were not (25 percent and 14 percent). After other variables had been controlled for, lithium prescriptions were significantly more common among patients who had suicidal ideation. CONCLUSIONS: Among patients with bipolar disorder who have suicidal ideation, antidepressants and second-generation antipsychotics appear to be prescribed by community practitioners more often than other medications, with lithium reserved for those with more severe illness characteristics.
Despite advances in pharmacotherapy, rates of attempted and completed suicide remain inordinately high among persons with bipolar disorder (1). Much of this elevated risk of suicidality appears to be driven by depression (2,3) and mixed mania (4)—clinical states for which existing treatments are often suboptimal. Standard antidepressants are often presumed to reduce suicide risk, with comparable efficacy among patients with either bipolar disorder or unipolar disorder (5). However, in the absence of controlled trials, the utility of long-term antidepressants for bipolar disorder remains subject to debate. Further investigations are needed to help clarify the relationships between pharmacotherapy and suicidality among patients with bipolar disorder.
The extent to which clinicians prescribe medications for bipolar disorder according to practice guideline recommendations or evidence-based algorithms is controversial (6,7,8,9). Suicidality as a target symptom represents one clinical variable of growing importance in prescribing decisions. Understandably, a considerable literature has emerged regarding the antisuicidal properties associated with some psychotropic drugs (10). Perhaps most notably, a six- to eight-fold reduction in the risk of suicide attempt or completion has been attributed to lithium therapy (11). Ahrens and Muller-Oerlinhausen (12) found this association to be independent of lithium's prophylactic benefit for affective episodes; however, these investigators did not control for antidepressant exposure. Angst and colleagues (1) found a protective effect for antidepressants and the combination of antidepressants or neuroleptics and lithium but not of lithium alone.
Goodwin and colleagues (13) found that suicide completion was 2.7 times more likely with divalproex than with lithium during an eight-year period among health plan enrollees with bipolar disorder. Again, that study did not assess the use of concomitant antidepressants or other pharmacotherapies and did not control for differences in severity of illness at baseline relative to prescription choice. Thus generalizations cannot easily be drawn about causal associations between different treatments and suicide risk. An alternative possible explanation for these findings is that primary care physicians are more inclined to prescribe newer medications than lithium, such as divalproex, for more severely or recently ill patients, who may be at the highest risk of suicide.
Little is known about the antisuicidal benefits of other new agents for bipolar disorder, particularly the second-generation antipsychotics. Among patients with schizophrenia, in a multicenter randomized blinded trial, clozapine was associated with a more extensive reduction in suicidal behavior than olanzapine (14). Secondary analyses of other schizophrenia trials suggest that olanzapine may have greater antisuicidal properties than risperidone (15) or haloperidol (16).
No studies have examined the effects of lithium and other medications on suicidal ideation as opposed to suicidal behaviors. It is possible that an agent could reduce a person's likelihood of acting on suicidal thoughts without necessarily reducing the presence of such thoughts. Suicidal ideation typically precedes a suicide attempt (17), appears to be a stronger distal than proximal predictor of suicidal behaviors (18), and may mediate the progression from depression to suicide attempts (19), particularly when suicidal ideation reaches its worst point (20).
It is inherently difficult to study suicide prospectively, given the low ratio of events to patient years, and even more difficult to conduct studies in randomized comparator trials. To provide a description of community-based pharmacotherapy treatments relative to suicidal ideation, in this article we report cross-sectional rates of suicidal ideation and use of psychotropic medications in a large, well-characterized group of patients with bipolar disorder upon their entry into a multisite outpatient study. The study examined the prevalence of prescriptions for mood stabilizers, second-generation antipsychotics, and antidepressants and the clinical features of patients who received these different classes of medications.
Methods
Study group
The study participants were the first 1,000 patients enrolled in the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD), a multisite nationwide clinical research program sponsored by the National Institute of Mental Health (NIMH) (21). Participants were recruited from the community through local, regional, and national advertisements. Patients who independently sought treatment from university-based bipolar disorder specialty clinics within the STEP-BD network were informed of the opportunity to participate in the STEP-BD program. The group was assessed between November 1999 and April 2001. These 1,000 participants represent a wide range of patients drawn from both academic and nonacademic treatment centers as well as Department of Veterans Affairs (VA) and community mental health centers. All participants provided written informed consent to participate in the study. The study protocol was approved by the institutional review boards at each of the STEP-BD sites.
The participants were at least 15 years of age and met DSM-IV criteria for bipolar I disorder, bipolar II disorder, cyclothymic disorder, bipolar disorder not otherwise specified, or schizoaffective manic or bipolar subtypes, based on the Modified International Neuropsychiatric Interview (MINI Plus Version 5.0) (22), administered by certified study diagnosticians (psychiatrists or clinical specialists with at least a master's degree in a relevant mental health discipline).
Clinical assessments
Detailed information about features of past and current illness, treatments, and aspects of current psychopathology were rated by the same staff, who used the Affective Disorders Evaluation (ADE), a standardized, semistructured instrument devised by Sachs and colleagues (23). The ADE incorporates a modified version of the mood and psychosis modules from the Structured Clinical Interview for DSM-IV while also assessing age at onset of mood disorders, the number of previous mood episodes, periods of recovery, suicidal behaviors, and past treatment responses. This instrument serves as the primary source of the history and characteristics of bipolar episodes and provides the basis for assigning a current clinical status. Diagnostic certification was achieved by all study personnel in the ADE by comparing ratings with benchmark ratings before collecting data for the study (21).
On the basis of their ADE responses, syndromic patients were assigned one of the following clinical status ratings according to DSM-IV criteria at entry into STEP-BD: major depression, mania, hypomania, or mixed episodes or cycling. Patients with no more than two symptoms of moderate severity or intensity for at least one week were considered to be euthymic.
Suicidal ideation was rated from the ADE by using a validated scale of 0 (absent) to 2 (present with high severity). For the purposes of this study, patients were considered to have suicidal ideation when they had at least several days of fleeting passive suicidal ideation in the previous week. Current use of psychotropics and other medications was obtained as part of the ADE, along with information about adherence to medications and doses missed in the preceding week. Global severity of illness was rated by a study psychiatrist using the Clinical Global Impressions Severity scale (CGI-S) (24). Severity of depressive symptoms at baseline was rated by using the first 17 items of the 23-item Hamilton Rating Scale for Depression (HAM-D) (25).
Statistical analyses
Data were initially analyzed with simple descriptive statistics. Mean group differences across multiple medication groups were analyzed with use of Kruskal-Wallis tests with post-hoc Tukey comparisons. Dichotomous variables were compared by using chi square or Fisher's exact tests. Logistic regression analyses were conducted to measure the strength of association between independent variables and the presence or absence of suicidal ideation (the dependent variable). The significance of the models was tested by using Wald chi square statistics and odds ratios with 95 percent confidence intervals. The statistical significance for all tests was set at p<.05. Because the analyses were exploratory, no correction was made for multiple tests.
Results
The mean±SD age of the study participants was 40.6±2.7 years. Of the 1,000 patients, 588 (59 percent) were women, 919 (92 percent) were Caucasian, 39 (4 percent) were African American, 11 (1 percent) were Asian American, 74 (.8 percent) were Native American, and 25 (2.5 percent) were of other ethnic origins. Participants were classified as having bipolar disorder type I (710 participants, or 71 percent), bipolar disorder type II (239 participants, or 24 percent), bipolar disorder not otherwise specified (41 participants, or 4 percent), schizoaffective bipolar disorder (seven participants, or .7 percent), or "bipolar other" (cyclothymic disorder) (three participants, or .3 percent).
At the time of study entry, 605 (61 percent) of 998 participants were euthymic, 58 (6 percent) were manic or hypomanic, 87 (9 percent) were mixed or cycling, and 248 (25 percent) were depressed; two patients did not provide complete data on syndromal status and suicidal ideation. Among this group, 211 (21 percent) exhibited signs of suicidal ideation on the ADE. Suicidal ideation was significantly more common among persons who were experiencing depressed (49 percent) or mixed (47 percent) episodes than among those who were manic or hypomanic (9 percent) or who were euthymic (7 percent) (χ2=224.198, df=3, p<.001).
Pharmacotherapy at study intake
Most participants (849, or 85 percent) were taking psychotropic medications at the time of study entry. Clinical characteristics of participants across medication groups are summarized in Table 1.
A total of 362 participants (36 percent) were taking lithium (overall mean±SD dosage, 944.8±383.2 mg/day), and 349 (35 percent) were taking divalproex (overall mean±SD dosage, 1,181.9±578.4 mg/day). A total of 270 persons (27 percent) were taking antipsychotics; nearly all were taking second-generation agents (264 persons). About two-thirds of the participants who were taking a second-generation antipsychotic were also taking lithium or divalproex (174 of 264, or 66 percent). Specific agents included olanzapine (135 participants; mean±SD dosage, 10.7±10.5 mg/day), risperidone (73 participants; 3.9±14.9 mg/day), quetiapine (47 participants; 150.0±134.6 mg/day), ziprasidone (two participants; 90.0±99.0 mg/day), and clozapine (seven participants; 197.0±157.7 mg/day).
A total of 418 participants (42 percent) were taking an antidepressant (346, or 83 percent, were taking one antidepressant, and 72, or 17 percent, were taking at least two antidepressants) at study entry. Specific antidepressants or subclasses included bupropion (143 participants), selective serotonin reuptake inhibitors (239 participants), venlafaxine (61 participants), mirtazapine (17 participants), nefazodone (29 participants), and monoamine oxidase inhibitors (six participants).
Suicidal ideation and treatment at study entry
Rates of suicidal ideation were similar between participants who were taking any lithium and those who were not (80 of 361 participants, or 22 percent, and 131 of 638 participants, or 26 percent, respectively) and were similar between those who were and those who were not taking any divalproex (71 of 349 participants, or 20 percent, and 140 of 650 participants, or 22 percent, respectively). Mean±SD lithium dosages did not differ significantly between patients with suicidal ideation (909.5± 408.4 mg/day) and those without (954.7±376.5mg/day), and there were no differences between those who were suicidal and those who were not in mean±SD divalproex dosages (1,209.7±741.9 compared with 1,174.8±530.0 mg/day, respectively).
The mean±SD number of medications being prescribed for patients with suicidal ideation—including multiple antidepressants, second-generation antipsychotics, and psychotropics in addition to lithium or divalproex—was significantly higher than for patients without suicidal ideation (1.64±.96 and 1.41±.96, respectively; Kruskal-Wallis χ2=11.64, df=1, p=.001). Multinomial regression adjusted for the effects of baseline HAM-D and GAF scores on the relationship between suicidal ideation and the number of medication groups (lithium, divalproex, second-generation antipsychotics, or antidepressants). Compared with persons who did not have suicidal ideation, those with suicidal ideation were more likely to be taking medications from two of these groups (p=.004) or three of these groups (p=.040) but not from all four groups.
Table 2 summarizes the proportions of study participants with and without suicidal ideation by medication groups. No significant differences in suicidal ideation were found across mood stabilizer combinations. Suicidal patients were more likely than nonsuicidal patients to have been taking an antidepressant (p<.001) or an antipsychotic (p<.05).
A logistic regression model was used to examine the strength of association between medication groups and patient characteristics (those that showed variation across medication groups) and the presence or absence of suicidal ideation (the dependent variable). Variables from Table 1 for which p was less than .10 were chosen for entry into the regression model.
As shown in Table 3, significant associations were evident between the presence of suicidal ideation and global severity of illness, current depressive episode, severity of current depression, a history of suicide attempts, and male gender (p<.05 for all). Use of lithium was significantly associated with suicidal ideation after these factors were controlled for, whereas no significant associations emerged between suicidal ideation and the use of divalproex, second-generation antipsychotics, or antidepressants.
Separate analyses were conducted to examine possible interactions between current HAM-D scores and lithium use relative to current suicidal ideation. In this model, HAM-D was highly associated with suicidal ideation (Wald χ2=65.94, df=1, p<.001), and lithium use was not, and there was no significant interaction. There also was no significant interaction between lithium use and a history of suicide attempts in predicting current suicidal ideation; a past suicide attempt in itself was significantly associated with current suicidal ideation (Wald χ2=18.70, df=1, p<.001), but lithium use was not.
Discussion
In this large cohort of patients with bipolar disorder who were evaluated at the time of entry into a specialized research-based treatment program, about one-fifth had suicidal ideation contemporaneous with taking lithium, divalproex, or a combination of the two. Atypical antipsychotics and antidepressants were both more likely to be taken by suicidal patients with bipolar disorder overall, although these distinctions were not maintained after baseline severity of illness characteristics and suicide attempt histories were controlled for.
Limitations of this study include the cross-sectional (rather than longitudinal) design, as well as the lack of control for treatment assignment, duration of treatment, and medication adherence. Although we report findings on practice patterns, causal inferences about treatment use and suicidality cannot be drawn.
Univariate analyses indicated that patients who were suicidal at study entry were more often receiving antidepressants or second-generation antipsychotics than patients without suicidal ideation. However, after suicidal patients' higher levels of illness severity, depression, and past suicide attempts were accounted for, practitioners were actually somewhat more likely than expected to prescribe lithium.
Our findings suggest that, after use of other medications and baseline severity indices were controlled for (such as severity of illness and history of suicide attempts), psychiatrists may be more likely to prescribe lithium for suicidal patients with bipolar disorder. It is possible that community practitioners will initially favor using antidepressants and second-generation antipsychotics for depressed patients with bipolar disorder who have suicidal features and reserve lithium for when greater signs of illness severity are present. However, the lack of an observed interaction between lithium use and current depressive severity or past suicide attempts relative to current suicidal ideation suggests that other factors mediate decisions about when to prescribe lithium for outpatients with bipolar disorder who have suicidal features. One could speculate that such factors might involve the degree to which practitioners may be apprehensive about the potential for lithium overdose, a preference for first using other medications with less narrow therapeutic indices or less intensive monitoring, and possibly an assumption that antidepressants are preferable to mood stabilizers among depressed and suicidal patients with bipolar disorder.
Although reports of the potential antisuicidal benefits of lithium are extensive, the data in this area derive mainly from uncontrolled studies that did not account for factors such as concomitant use of other medications (for example, antidepressants), rates and reasons for attrition, and clinicians' prescribing biases (for example, concerns about lethality in overdose) (10). As in the study we report here, Coryell and associates (26) found that lithium therapy was more common among persons who attempted or completed suicide than among those who did not attempt suicide. In addition, Angst and colleagues (1) found during a 34- to 38-year follow-up period that significantly fewer suicide completions occurred among patients with mood disorders who took lithium plus antidepressants, but no such reduction was evident among those who took lithium alone.
Only two prospective long-term randomized trials have specifically assessed suicide risk with lithium compared with an active comparator: Thies-Flechtner and colleagues (27), over a 2.5-year study of 378 patients with bipolar disorder, unipolar disorder, or schizoaffective disorder, found significantly more suicide attempts or completions with carbamazepine (nine patients) than with lithium (zero patients). Prien and colleagues (28), over a two-year period in which they studied 205 patients with bipolar disorder, observed no suicide completions with lithium or imipramine, compared with two completions in a placebo group. A recent meta-analysis of controlled trials of lithium use among patients with mood disorders showed a significant reduction in suicide deaths and deliberate self-harm (29), although the possibility exists that the optimal antisuicide effects of lithium become attenuated under conditions of ordinary clinical practice.
The observed cross-sectional association between lithium use and higher rates of suicidal ideation raises a number of further points of clinical and theoretical importance. Although one could hypothesize from our findings that lithium might induce suicidal ideation among patients with bipolar disorder, a causal link cannot be tested or substantiated on the basis of our cross-sectional design. Moreover, such an explanation would be unlikely and would be inconsistent with previous evidence (10). On the basis of current cross-sectional observations, other, more plausible hypotheses warrant future prospective examination.
First, lithium use could lead to a dissociation between suicidal ideation and suicidal behaviors. That is, lithium could diminish the likelihood of acts related to suicidality—for example, via modulatory effects on impulsivity or aggression—even if it fails to diminish suicidal thoughts. This hypothesis is consistent with findings that suicide attempts and completions are more closely associated with impulsivity than premeditation (30) and that lithium reduces impulsivity and aggression (31). No previous studies have addressed the potential impact of lithium or other psychotropic agents on suicidal thoughts as opposed to suicidal acts.
Second, it is possible that lithium could reduce suicidality through its effects on depression among patients with bipolar disorder (2). In the study we report here, a majority of persons who had suicidal features were seeking treatment for a current depressed or mixed episode—that is, patients for whom current medications had, by definition, not provided optimal thymoleptic benefits. The potential antisuicidal properties of lithium relative to other compounds with demonstrated antidepressant effects—such as standard antidepressants or lamotrigine—deserves investigation (10).
A third consideration involves uncertainty about when clinicians may have chosen to prescribe lithium, or other medications, relative to longitudinal changes in psychopathology. Although data on the duration of lithium treatment and adherence to adequate dosing were not available, such factors play a critical role in assessments of the efficacy of lithium (32) and attempts to discern changes in suicide risk over time. Such considerations become highlighted by previous observations that most patients with bipolar disorder discontinue lithium within three months of starting it (33) and that suicidal behaviors may increase above baseline rates in the year after discontinuation of lithium (2). Recent findings also indicate that the use of a maximally supportive formal treatment program may be an essential ingredient to optimize the antisuicidal benefits of lithium (34).
Our data raise the possibility that practitioners may reserve lithium use for more severely ill, high-risk patients. Because the prophylactic value of lithium appears better when lithium is introduced early rather than late in the lifetime course of illness, it is possible that its antisuicidal benefit also may attenuate if it is not introduced early in treatment. Longitudinal studies are needed to examine this hypothesis.
Suicidal behavior is a heterogeneous and multideterminate phenomenon. Numerous factors mediate or moderate the relationship between thymoleptic drug therapies and suicide risk. Such factors may include elements specific to treatment itself (for example, medication adherence, duration of treatment, adequacy of therapy, and pharmacokinetic synergies) as well as illness-related characteristics (for example, comorbid illnesses). Subsequent longitudinal study of drug therapies, mediating variables, and suicidal thoughts or behaviors may help to shed greater light on the prevention of suicide among patients with bipolar disorder.
Conclusions
Suicidal ideation appears to be present among about one-fifth of patients with bipolar disorder who seek care through specialty treatment programs for bipolar disorder, regardless of whether they take lithium, divalproex, or a combination of the two at the time of initial presentation. Community-based practitioners appear more likely to introduce lithium in the case of depressed, suicidal patients with bipolar disorder who have had past suicide attempts and more severe illness features. Prospective, longitudinal studies are needed to help clarify the optimal impact of mood stabilizers on subsequent suicide risk relative to other psychotropic agents.
Acknowledgments
Portions of this research were funded by K-23 Career Development Award MH-01936 from the National Institute of Mental Health (NIMH), a National Alliance for Research on Schizophrenia and Depression Young Investigator Award, and a grant from the American Foundation for Suicide Prevention. Partial federal funding from NIMH was provided under contract N01-MH-80001.
Dr. Goldberg is affiliated with the affective disorders program at Silver Hill Hospital, 208 Valley Road, New Canaan, Connecticut 06840 (e-mail, [email protected]). Dr. Allen and Dr. Chessick are with the department of psychiatry of the University of Colorado School of Medicine in Denver. Dr. Miklowitz is with the department of psychology of the University of Colorado in Boulder. Dr. Bowden is with the department of psychiatry of the University of Texas Health Science Center in San Antonio. Ms. Endick is with the department of psychiatry of The Feinberg School of Medicine at Northwestern University in Chicago. Dr. Wisniewski and Ms. Miyahara are with the department of epidemiology of the School of Public Health at the University of Pittsburgh. Dr. Sagduyu is with the School of Medicine and the University of Missouri in Kansas City. Dr. Thase is with the Western Psychiatric Institute and Clinic at the University of Pittsburgh. Dr. Calabrese is with the department of psychiatry of Case Western Reserve University in Cleveland, Ohio. Dr. Sachs is with the department of psychiatry at Massachusetts General Hospital in Boston. This paper was presented in part at the annual meeting of the American College of Neuropsychopharmacology held December 8 to 12, 2002, in San Juan, Puerto Rico.
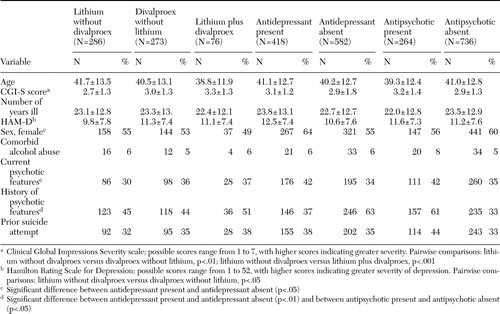 |
Table 1. Characteristics of illness in a sample of patients in the Systematic Treatment Enhancement Program for bipolar disorder, by primary medication
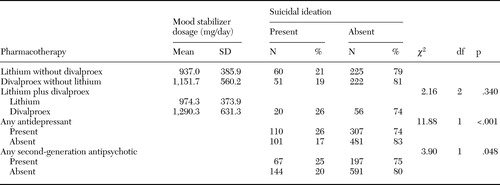 |
Table 2. Suicidal ideation in a sample of patients with bipolar disorder, by current pharmacotherapy
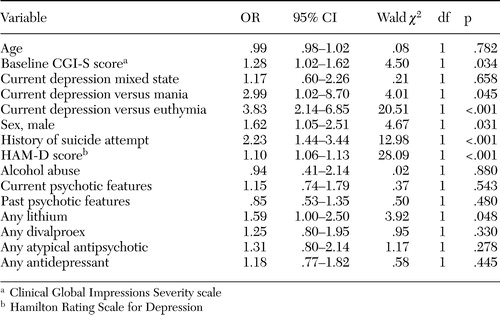 |
Table 3. Results of logistic regression analysis examining suicidal ideation relative to pharmacotherapy and major clinical characteristics
1. Angst F, Stassen HH, Clayton PJ, et al: Mortality of patients with mood disorders: follow-up over 34–38 years. Journal of Affective Disorders 68:167–181,2002Crossref, Medline, Google Scholar
2. Tondo L, Baldessarini J, Hennen J, et al: Lithium treatment and risk of suicidal behavior in bipolar disorder patients. Journal of Clinical Psychiatry 59:404–414,1998Crossref, Google Scholar
3. Strakowski SM, McElroy SL, Keck PE Jr, et al: Suicidality among patients with mixed and manic bipolar disorder. American Journal of Psychiatry 153:674–676,1996Link, Google Scholar
4. Goldberg JF, Garno JL, Leon AC, et al: Association of recurrent suicidal ideation with nonremission from acute mixed mania. American Journal of Psychiatry 155:1753–1755,1998Link, Google Scholar
5. Möller JH, Grunze H: Have some guidelines for the treatment of acute bipolar depression gone too far in the restriction of antidepressants? European Archives of Psychiatry and Clinical Neuroscience 250:57–58,2000Google Scholar
6. Goldberg JF: Treatment guidelines: current and future management of bipolar disorder. Journal of Clinical Psychiatry 61(suppl 13):12–18,2000Google Scholar
7. Levine J, Chengappa KNR, Brar JS, et al: Psychotropic drug prescription patterns among patients with bipolar I disorder. Bipolar Disorders 2:120–130,2000Crossref, Medline, Google Scholar
8. Suppes T, Rush AJ, Dennehy EB, et al: Texas Medication Algorithm Project, Phase 3 (TMAP-3): clinical results for patients with a history of mania. Journal of Clinical Psychiatry 64:370–382,2003Crossref, Medline, Google Scholar
9. Lloyd AJ, Harrison CL, Ferrier IN, et al: The pharmacologic treatment of bipolar affective disorder: practice is improving but could still be better. Journal of Psychopharmacology 17:230–233,2003Crossref, Medline, Google Scholar
10. Ernst CL, Goldberg JF: Antisuicide properties of psychotropic drugs: a critical review. Harvard Review of Psychiatry 12:14–41,2004Crossref, Medline, Google Scholar
11. Baldessarini RJ, Tondo L, Hennen J: Lithium treatment and suicide risk in major affective disorders: update and new findings. Journal of Clinical Psychiatry 64(suppl 5):44–52,2003Medline, Google Scholar
12. Ahrens B, Muller-Oerlinghausen B: Does lithium exert an independent antisuicide effect? Pharmacopsychiatry 34:132–136,2001Google Scholar
13. Goodwin FK, Fireman B, Simon GE, et al: Suicide risk in bipolar disorder during treatment with lithium and divalproex. JAMA 290:1467–1473,2003Crossref, Medline, Google Scholar
14. Meltzer HY, Alphs L, Green AI, et al: International Suicide Prevention Trial Study Group. Clozapine for suicidality in schizophrenia: International Suicide Prevention Trial (InterSePT). Archives of General Psychiatry 60:82–89,2003Crossref, Medline, Google Scholar
15. Tran PV, Hamilton SH, Kuntz AJ, et al: Double-blind comparison of olanzapine versus risperidone in the treatment of schizophrenia and other psychotic disorders. Journal of Clinical Psychopharmacology 17:407–418,1997Crossref, Medline, Google Scholar
16. Glazer WM: Formulary decisions and health economics. Journal of Clinical Psychiatry 59(suppl 19):23–29,1998Medline, Google Scholar
17. Kessler RC, Borges G, Walters EE: Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Archives of General Psychiatry 56:617–626,1999Crossref, Medline, Google Scholar
18. Fawcett J, Scheftner WA, Fogg L, et al: Time-related predictors of suicide in major affective disorder. American Journal of Psychiatry 148:1092–1093,1991Link, Google Scholar
19. Dieserud G, Roysamb E, Ekeberg O, et al: Toward an integrative model of suicide attempt: a cognitive psychological approach. Suicide and Life-Threatening Behavior 31:153–168,2001Crossref, Medline, Google Scholar
20. Beck AT, Brown GK, Steer RA, et al: Suicide ideation at its worst point: a predictor of eventual suicide in psychiatric outpatients. Suicide and Life-Threatening Behavior 29:1–9,1999Medline, Google Scholar
21. Sachs GS, Thase ME, Otto MW, et al: Rationale, design, and methods of the Systematic Treatment Enhancement Program for Bipolar Disorder (STEP-BD). Biological Psychiatry 53:1028–1042,2003Crossref, Medline, Google Scholar
22. Sheehan DV, Lecrubier Y, Harnett-Sheehan K, et al: Reliability and validity of the MINI International Neuropsychiatric Interview (MINI): according to the SCID-P. European Psychiatry 12:232–241,1997Crossref, Google Scholar
23. Sachs GS: Use of clonazepam for bipolar affective disorder. Journal of Clinical Psychiatry 51(suppl):31–34,1990Google Scholar
24. Guy W: ECDEU Assessment Manual for Psychopharmacology, Revised. US Department of Health, Education, and Welfare publication (ADM) 76–338. Rockville, Md, National Institute of Mental Health, 1976Google Scholar
25. Hamilton M: Development of a rating scale for primary depressive illness. British Journal of Social and Clinical Psychology 6:278–296,1967Crossref, Medline, Google Scholar
26. Coryell W, Arndt S, Turvey C, et al: Lithium and suicidal behavior in major affective disorder: a case-control study. Acta Psychiatrica Scandinavica 104:193–197,2001Crossref, Medline, Google Scholar
27. Thies-Flechtner K, Muller-Oerlinghausen B, Seibert W, et al: Effect of prophylactic treatment on suicide risk in patients with major affective disorders: data from a randomized prospective trial. Pharmacopsychiatry 29:103–107,1996Crossref, Medline, Google Scholar
28. Prien RF, Klett CJ, Caffey EM: Lithium prophylaxis in recurrent affective illness. American Journal of Psychiatry 131:198–203,1974Link, Google Scholar
29. Cipriani A, Pretty H, Hawton K, et al: Lithium use in the prevention of suicidal behavior and all-cause mortality in patients with mood disorders: a systematic review of randomized trials. American Journal of Psychiatry 162:1805–1819,2005Link, Google Scholar
30. Baca-Garcia E, Diaz-Sastre C, Basurte E, et al: A prospective study of the paradoxical relationship between impulsivity and lethality of suicide attempts. Journal of Clinical Psychiatry 62:560–564,2001Crossref, Medline, Google Scholar
31. Sheard M: Effect of lithium on human aggression. Nature 230:113–114,1971Crossref, Medline, Google Scholar
32. Perlis RH, Sachs GS, Lafer B, et al: Effect of abrupt change from standard to low serum levels of lithium: a reanalysis of double-blind lithium maintenance data. American Journal of Psychiatry 159:1155–1159,2002Link, Google Scholar
33. Johnson RE, McFarland BH: Lithium use and discontinuation in a health maintenance organization. American Journal of Psychiatry 153:993–1000,1996Link, Google Scholar
34. Rucci P, Frank E, Kostelnik B, et al: Suicide attempts in patients with bipolar I disorder during acute and maintenance phases of intensive treatment with pharmacotherapy and adjunctive psychotherapy. American Journal of Psychiatry 159:1160–1164,2002Link, Google Scholar



